Abstract
Objectives
The presence of non-alcoholic fatty liver disease (NAFLD) has been associated with major adverse cardiovascular events (MACEs); however, the mechanisms that initiate the risk for MACEs in patients with NAFLD remain unknown. We sought to investigate whether plaque progression (PP), determined by coronary CT angiography (CCTA), moderate the relationship between NAFLD and MACEs.
Methods
A total of 1683 asymptomatic participants (mean age, 63.3 ± 9.4 [range, 38–85] years; 1117 men) who underwent baseline and follow-up CCTA examination were prospectively included in our study. All of the participants were divided into the NAFLD and non-NAFLD groups. PP was determined by follow-up CCTA. The primary endpoint was MACEs, defined as the composite of all-cause death, nonfatal myocardial infarction, and unplanned hospitalization for acute coronary syndrome leading to revascularization.
Results
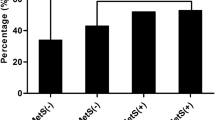
At follow-up CCTA, participants with NAFLD showed higher incidence of PP than those without [33.0% (248/752) vs. 16.6% (155/931), p < 0.001]. Compared with non-NAFLD participants, participants with NAFLD had a lower 9.7-year event-free survival rate (80.9 vs. 66.4%, log-rank p < 0.001). Cox regression analysis revealed NAFLD was significantly associated with MACEs (HR = 1.63, 95% CI: 1.28 to 2.06, p < 0.001) after adjusting for covariables. However, this association was no longer significant after adjustment for PP (HR = 1.10, 95% CI: 0.84 to 1.45, p = 0.496). The mediation analysis revealed that PP had a significant indirect effect (β = 0.0587, 95% CI: 0.0424 to 0.08, p < 0.001) and mediated 99.8% (p = 0.002) for the relationship between NAFLD and MACEs.
Conclusions
Plaque progression, identified by follow-up CCTA, mediates the relationship between NAFLD and MACEs.
Key Points
-
The incidence of CCTA–identified PP was higher for participants with NAFLD than those without NAFLD (248/752 [33.0%] vs. 155/931 [16.6%], p < 0.001).
-
Participants with NAFLD had a lower 9.7-year event-free survival rate than those without NAFLD (66.4% vs. 80.9%, log-rank p < 0.001).
-
The mediation analysis revealed that PP had a significant indirect effect (β = 0.0587, 95% CI: 0.0424 to 0.08, p < 0.001) and mediated 99.8% (p = 0.002) for the relationship between NAFLD and MACEs.





Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery disease
- CAD-RADS:
-
Coronary Artery Disease Reporting and Data System
- CCTA:
-
Coronary CT angiography
- CI:
-
Confidence interval
- CPV:
-
Calcified plaque volume
- CVD:
-
Cardiovascular disease
- HR:
-
Hazard ratio
- ICC:
-
Intra-class correlation coefficients
- MACEs:
-
Major adverse cardiovascular events
- NAFLD:
-
Non-alcoholic fatty liver disease
- NCPV:
-
Non-calcified plaque volume
- NCV:
-
Necrotic core volume
- PCI:
-
Percutaneous coronary intervention
- PP:
-
Plaque progression
- TPV:
-
Total plaque volume
References
Zhou J, Zhou F, Wang W et al (2020) Epidemiological feature of NAFLD from 1999 to 2018 in China. Hepatology. https://doi.org/10.1002/hep.31150
Chalasani N, Younossi Z, Lavine JE et al (2018) The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67:328–357
Pais R, Redheuil A, Cluzel P, Ratziu V, Giral P (2019) Relationship among fatty liver, specific and multiple-site atherosclerosis, and 10-year Framingham score. Hepatology 69:1453–1463
Sinn DH, Kang D, Chang Y et al (2017) Non-alcoholic fatty liver disease and progression of coronary artery calcium score: a retrospective cohort study. Gut 66:323–329
Kim D, Choi SY, Park EH et al (2012) Nonalcoholic fatty liver disease is associated with coronary artery calcification. Hepatology 56:605–613
Lee SB, Park GM, Lee JY et al (2018) Association between non-alcoholic fatty liver disease and subclinical coronary atherosclerosis: an observational cohort study. J Hepatol 68:1018–1024
Meyersohn NM, Mayrhofer T, Corey KE et al (2020) Association of hepatic steatosis with major adverse cardiovascular events, independent of coronary artery disease. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2020.07.030
Labenz C, Huber Y, Michel M et al (2020) Impact of NAFLD on the incidence of cardiovascular diseases in a primary care population in Germany. Dig Dis Sci 65:2112–2119
Puchner SB, Lu MT, Mayrhofer T et al (2015) High-risk coronary plaque at coronary CT angiography is associated with nonalcoholic fatty liver disease, independent of coronary plaque and stenosis burden: results from the ROMICAT II trial. Radiology 274:693–701
Motoyama S, Ito H, Sarai M et al (2015) Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J Am Coll Cardiol 66:337–346
Yu M, Li W, Lu Z, Wei M, Yan J, Zhang J (2018) Quantitative baseline CT plaque characterization of unrevascularized non-culprit intermediate coronary stenosis predicts lesion volume progression and long-term prognosis: a serial CT follow-up study. Int J Cardiol 264:181–186
Smit JM, van Rosendael AR, El Mahdiui M et al (2020) Impact of clinical characteristics and statins on coronary plaque progression by serial computed tomography angiography. Circ Cardiovasc Imaging 13:e009750
Budoff MJ, Dowe D, Jollis JG et al (2008) Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 52:1724–1732
Lee SE, Chang HJ, Sung JM et al (2018) Effects of statins on coronary atherosclerotic plaques: the PARADIGM Study. JACC Cardiovasc Imaging 11:1475–1484
Cury RC, Abbara S, Achenbach S et al (2016) CAD-RADS™: Coronary Artery Disease - Reporting and Data System: an expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J Am Coll Radiol 13:1458–1466 e1459
Kodama Y, Ng CS, Wu TT et al (2007) Comparison of CT methods for determining the fat content of the liver. AJR Am J Roentgenol 188:1307–1312
Speliotes EK, Massaro JM, Hoffmann U et al (2008) Liver fat is reproducibly measured using computed tomography in the Framingham Heart Study. J Gastroenterol Hepatol 23:894–899
Hicks KA, Tcheng JE, Bozkurt B et al (2015) 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol 66:403–469
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51:1173–1182
Preacher KJ, Hayes AF (2004) SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput 36:717–731
Kim U, Leipsic JA, Sellers SL et al (2018) Natural history of diabetic coronary atherosclerosis by quantitative measurement of serial coronary computed tomographic angiography: results of the PARADIGM Study. JACC Cardiovasc Imaging 11:1461–1471
Niikura T, Imajo K, Ozaki A et al (2020) Coronary artery disease is more severe in patients with non-alcoholic steatohepatitis than fatty liver. Diagnostics (Basel) 10
Idilman IS, Akata D, Hazirolan T, Doganay Erdogan B, Aytemir K, Karcaaltincaba M (2015) Nonalcoholic fatty liver disease is associated with significant coronary artery disease in type 2 diabetic patients: a computed tomography angiography study 2. J Diabetes 7:279–286
Wu S, Wu F, Ding Y, Hou J, Bi J, Zhang Z (2016) Association of non-alcoholic fatty liver disease with major adverse cardiovascular events: a systematic review and meta-analysis. Sci Rep 6:33386
Villanova N, Moscatiello S, Ramilli S et al (2005) Endothelial dysfunction and cardiovascular risk profile in nonalcoholic fatty liver disease. Hepatology 42:473–480
Bieghs V, Rensen PC, Hofker MH, Shiri-Sverdlov R (2012) NASH and atherosclerosis are two aspects of a shared disease: central role for macrophages. Atherosclerosis 220:287–293
Speliotes EK, Yerges-Armstrong LM, Wu J et al (2011) Genome-wide association analysis identifies variants associated with nonalcoholic fatty liver disease that have distinct effects on metabolic traits. PLoS Genet 7:e1001324
Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C (2016) Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol 65:589–600
Zeb I, Li D, Budoff MJ et al (2016) Nonalcoholic fatty liver disease and incident cardiac events: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol 67:1965-1966
Stone GW, Maehara A, Lansky AJ et al (2011) A prospective natural-history study of coronary atherosclerosis. N Engl J Med 364:226–235
Zaman T, Agarwal S, Anabtawi AG et al (2012) Angiographic lesion severity and subsequent myocardial infarction. Am J Cardiol 110:167–172
Yokoya K, Takatsu H, Suzuki T et al (1999) Process of progression of coronary artery lesions from mild or moderate stenosis to moderate or severe stenosis: a study based on four serial coronary arteriograms per year. Circulation 100:903–909
Ahmadi A, Argulian E, Leipsic J, Newby DE, Narula J (2019) From subclinical atherosclerosis to plaque progression and acute coronary events: JACC state-of-the-art review. J Am Coll Cardiol 74:1608–1617
Ahmadi A, Narula J (2017) Primary and secondary prevention, or subclinical and clinical atherosclerosis. JACC Cardiovasc Imaging 10:447–450
Funding
This study is supported by the National Natural Science Foundation of China (Grant No.: 82102033), Shanghai Sailing Program (Grant No.: 20YF1435900), Zhongshan Hospital Fudan University Science Foundation for Youth (Grant No.: 2021ZSQN03), Shanghai Municipal Key Clinical Specialty (Grant No.: shslczdzk03202) and Shanghai Clinical Research Center for Interventional Medicine (Grant No.: 19MC1910300).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Meng-Su Zeng.
Conflict of interest
Zhi-Han Xu, MD, is an employee of Siemens Healthineers. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all participants in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 5987 kb)
Rights and permissions
About this article
Cite this article
Yu, MM., Tang, XL., Zhao, X. et al. Plaque progression at coronary CT angiography links non-alcoholic fatty liver disease and cardiovascular events: a prospective single-center study. Eur Radiol 32, 8111–8121 (2022). https://doi.org/10.1007/s00330-022-08904-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08904-2