Abstract
Objectives
The purpose of this study was to establish two preoperative nomograms to evaluate the risk for axillary lymph node (ALN) metastasis in early breast cancer patients based on ultrasonographic-clinicopathologic features.
Methods
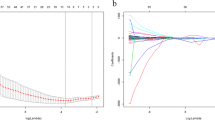
We prospectively evaluated 593 consecutive female participants who were diagnosed with cT1-3N0-1M0 breast cancer between March 2018 and May 2019 at Sun Yat-Sen Memorial Hospital. The participants were randomly classified into training and validation sets in a 4:1 ratio for the development and validation of the nomograms, respectively. Multivariate logistic regression analysis was performed to identify independent predictors of ALN status. We developed Nomogram A and Nomogram B to predict ALN metastasis (presence vs. absence) and the number of metastatic ALNs (≤ 2 vs. > 2), respectively.
Results
A total of 528 participants were evaluated in the final analyses. Multivariable analysis revealed that the number of suspicious lymph nodes, long axis, short-to-long axis ratio, cortical thickness, tumor location, and histological grade were independent predictors of ALN status. The AUCs of nomogram A in the training and validation groups were 0.83 and 0.78, respectively. The AUCs of nomogram B in the training and validation groups were 0.87 and 0.87, respectively. Both nomograms were well-calibrated.
Conclusion
We developed two preoperative nomograms that can be used to predict ALN metastasis (presence vs. absence) and the number of metastatic ALNs (≤ 2 vs. > 2) in early breast cancer patients. Both nomograms are useful tools that will help clinicians predict the risk of ALN metastasis and facilitate therapy decision-making about axillary surgery.
Key Points
• We developed two preoperative nomograms to predict axillary lymph node status based on ultrasonographic-clinicopathologic features.
• Nomogram A was used to predict axillary lymph node metastasis (presence vs. absence). The AUCs in the training and validation groups were 0.83 and 0.78, respectively. Nomogram B was used to estimate the number of metastatic lymph nodes ( ≤ 2 vs. > 2). The AUCs in the training and validation group were 0.87 and 0.87, respectively.
• Our nomograms may help clinicians weigh the risks and benefits of axillary surgery more appropriately.





Similar content being viewed by others
Abbreviations
- ACOSOG:
-
American College of Surgeons Oncology Group
- ALN:
-
Axillary lymph node
- ALND:
-
Axillary lymph node dissection
- ASCO:
-
American Society of Clinical Oncology
- ER:
-
Estrogen receptor
- FNR:
-
False-negative rate
- Her-2:
-
Human epidermal growth factor receptor-2
- MSKCC:
-
Memorial Sloan-Kettering Cancer Center
- PR:
-
Progesterone receptor
- SLN:
-
Sentinel lymph node
- SLNB:
-
Sentinel lymph node biopsy
- TILs:
-
Tumor-infiltrating lymphocytes
References
Soerjomataram I, Louwman MW, Ribot JG, Roukema JA, Coebergh JW (2008) An overview of prognostic factors for long-term survivors of breast cancer. Breast Cancer Res Treat 107(3):309–330
Xie F, Yang H, Wang S et al (2012) A logistic regression model for predicting axillary lymph node metastases in early breast carcinoma patients. Sensors (Basel) 12(7):9936–9950
Giuliano AE, Hunt KK, Ballman KV et al (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305(6):569–575
Giuliano AE, Ballman KV, McCall L et al (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318(10):918–926
Donker M, van Tienhoven G, Straver ME et al (2014) Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol 15(12):1303–1310
Lucci A, McCall LM, Beitsch PD et al (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol 25(24):3657–3663
Lyman GH, Guiliano AE, Somerfield MR et al (2005) Americal Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early stage breast cancer. J Clin Oncol 23:7703–7720
Diepstraten SC, Sever AR, Buckens CF et al (2014) Value of preoperative ultrasound-guided axillary lymph node biopsy for preventing completion axillary lymph node dissection in breast cancer: a systematic review and meta-analysis. Ann Surg Oncol 21(1):51–59
Gentilini O, Veronesi U (2012) Abandoning sentinel lymph node biopsy in early breast cancer? A new trial in progress at the Eurpean Institute of Oncology of Milan (SOUND: Sentinel node vs Observation after axillary UltraSouND). Breast 21(5):678–681
Bevilacqua JL, Kattan MW, Fey JV, Cody HS, Borgen PI, Van Zee KJ (2007) Doctor, what are my chances of having a positive sentinel node? A validated nomogram for risk estimation. Clin Oncol 25:3670–3679
Klar M, Foeldi M, Markert S, Gitsch G, Stickeler E, Watermann D (2009) Good prediction of the likelihood for sentinel lymph node metastasis by using the MSKCC nomogram in a German breast cancer population. Ann Surg Oncol 16(5):1136–1142
Qiu PF, Lui JJ, Wang YS et al (2012) Risk factors for sentinel lymph node metastasis and validation study of the MSKCC nomogram in breast cancer patients. Jpn J Clin Oncol 42(11):1002–1007
Ecanow JS, Abe H, Newstead GM, Ecanow DB, Jeske JM (2013) Axillary staging of breast cancer: what the radiologist should know. Radiographics 33(6):1589–1612
Yang WT, Chang J, Metreweli C (2000) Patients with breast cancer: differences in color Doppler flow and gray-scale US features of benign and malignant lymph nodes. Radiology 215(2):568–573
Bedi DG, Krishnamurthy R, Krishnamurthy S et al (2008) Cortical morphologic features of axillary lymph nodes as a predictor of metastasis in breast cancer: in vitro sonographic study. AJR Am J Roentgenol 191(3):646–652
Lee B, Lim AK, Krell J et al (2013) The efficacy of axillary ultrasound in the detection of nodal metastasis in breast cancer. AJR Am J Roentgenol 200(3):W314–W320
Wolff AC, Hammond ME, Schwartz JN et al (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 131(1):18–45
Salgado R, Denkert C, Demaria S et al (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26(2):259–271
Coates AS, Winer EP, Goldhirsch A et al (2015) Tailoring therapies--improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol 26(8):1533–1546
Banerjee M, George J, Song EY, Roy A, Hryniuk W (2004) Tree-based model for breast cancer prognostication. J Clin Oncol 22(13):2567–2575
Galimberti V, Cole BF, Zurrida S et al (2013) Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol 14(4):297–305
Choi JS, Kim MJ, Moon HJ, Kim EK, Yoon JH (2012) False negative results of preoperative axillary ultrasound in patients with invasive breast cancer: correlations with clinicopathologic findings. Ultrasound Med Biol 38(11):1881–1886
Zong Q, Deng J, Ge W, Chen J, Xu D (2020) Establishment of simple nomograms for predicting axillary lymph node involvement in early breast cancer. Cancer Manag Res 12:2025–2035
Hieken TJ, Trull BC, Boughey JC et al (2013) Preoperative axillary imaging with percutaneous lymph node biopsy is valuable in the contemporary management of patients with breast cancer. Surgery 154(4):831–838 (discussion 838–840)
Washington University School of Medicine. Axillary ultrasound with or without sentinel lymph node biopsy in detecting the spread of breast cancer in patients receiving breast conservation therapy [ClinicalTrials.gov identifier NCT01821768]. US National Institutes of Health, ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT01821768.
Abe H, Schmidt RA, Kulkarni K, Sennett CA, Mueller JS, Newstead GM (2009) Axillary lymph nodes suspicious for breast cancer metastasis: sampling with US-guided 14-gauge core-needle biopsy--clinical experience in 100 patients. Radiology 250(1):41–49
Choi YJ, Ko EY, Han BK, Shin JH, Kang SS, Hahn SY (2009) High-resolution ultrasonographic features of axillary lymph node metastasis in patients with breast cancer. Breast 18(2):119–122
Mainiero MB, Cinelli CM, Koelliker SL, Graves TA, Chung MA (2010) Axillary ultrasound and fine-needle aspiration in the preoperative evaluation of the breast cancer patient: an algorithm based on tumor size and lymph node appearance. AJR Am J Roentgenol 195:1261–1267
Pilewskie M, Mautner SK, Stempel M, Eaton A, Morrow M (2016) Does a positive axillary lymph node needle biopsy result predict the need for an axillary lymph node dissection in clinically node-negative breast cancer patients in the ACOSOG Z0011 era? Ann Surg Oncol 23(4):1123–1128
Harris CK, Tran HT, Lee K et al (2017) Positive ultrasound-guided lymph node needle biopsy in breast cancer may not mandate axillary lymph node dissection. Ann Surg Oncol 24(10):3004–3010
Abe H, Schacht D, Sennett CA, Newstead GM, Schmidt RA (2013) Utility of preoperative ultrasound for predicting pN2 or higher stage axillary lymph node involvement in patients withnewly diagnosed breast cancer. AJR Am J Roentgenol 200(3):696–702
Alvarez S, Anorbe E, Alcorta P, Lopez F, Alonso I, Cortes J (2006) Role of Sonography in the Diagnosis of Axillary Lymph Node Metastases in Breast Cancer: A Systematic Review. AJR Am J Roentgenol 186(5):1342–1348
Chen JY, Chen JJ, Yang BL et al (2012) Predicting sentinel lymph node metastasis in a Chinese breast cancer population: assessment of an existing nomogram and a new predictive nomogram. Breast Cancer Res Treat 135(3):839–848
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (81972467), the Guangdong Natural Science Foundation (2020A1515010458), and the Guangzhou Science Technology and Innovation Commission (202102010221, 20212200003). We appreciate the assistance from Artificial Intelligence Lab, Sun Yat-sen Memorial Hospital. We thank all the individuals who took part in these studies and all the researchers, clinicians, and technicians who have enabled this work to be carried out.
Funding
This study has received funding from the National Natural Science Foundation of China (81972467), the Guangdong Natural Science Foundation (2020A1515010458), and the Guangzhou Science Technology and Innovation Commission (202102010221, 20212200003).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Fengyan Yu, MD, PHD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Yaping Yang (Diagnostic Department, Breast Tumor Center, Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University, Guangzhou, China) specializes in statistical analysis and provided statistical advice in this study.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 34 kb)
Rights and permissions
About this article
Cite this article
Fong, W., Tan, L., Tan, C. et al. Predicting the risk of axillary lymph node metastasis in early breast cancer patients based on ultrasonographic-clinicopathologic features and the use of nomograms: a prospective single-center observational study. Eur Radiol 32, 8200–8212 (2022). https://doi.org/10.1007/s00330-022-08855-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08855-8