Abstract
Objectives
To evaluate the incidence of adverse drug reactions (ADRs), including hypersensitivity reactions (HSRs) and post-contrast acute kidney injury (PC-AKI), after intra-arterial (IA) administration of ioversol.
Methods and materials
A systematic literature search was performed (1980–2021) and studies documenting IA use of ioversol, and reporting safety outcomes were selected. Key information on study design, patients’ characteristics, indication, dose, and type of safety outcome were extracted.
Results
Twenty-eight studies (including two pediatric studies) with 8373 patients exposed to IA ioversol were selected. Studies were highly heterogenous in terms of design, PC-AKI definition, and studied population. PC-AKI incidence after coronary angiography was 7.5–21.9% in a general population, 4.0-26.4% in diabetic patients, and 5.5–28.9% in patients with chronic kidney disease (CKD). PC-AKI requiring dialysis was rare and reported mainly in patients with severe CKD. No significant differences in PC-AKI rates were shown in studies comparing different iodinated contrast media (ICM). Based on seven studies of ioversol clinical development, the overall ADR incidence was 1.6%, comparable to that reported with other non-ionic ICM. Pediatric data were scarce with only one study reporting on PC-AKI incidence (12%), and one reporting on ADR incidence (0.09%), both after coronary angiography.
Conclusions
After ioversol IA administration, PC-AKI incidence was highly variable between studies, likely reflecting the heterogeneity of the included study populations, and appeared comparable to that reported with other ICM. The rate of other ADRs appears to be low. Well-designed studies are needed for a better comparison with other ICM.
Key Points
• PC-AKI incidence after IA administration of ioversol appears to be comparable to that of other ICM, despite the high variability between studies.
• The need for dialysis after IA administration of ioversol is rare.
• No obvious difference was found regarding the safety profile of ioversol between IA and IV administration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ioversol (Optiray®, Guerbet), a non-ionic monomeric low-osmolar iodinated contrast medium (ICM, LOCM), has been used for more than three decades in a variety of X-ray-based modalities involving intravenous (IV) administration such as CT, angiography, and venography or intra-arterial (IA) administration such as coronary, cerebral, or peripheral angiography.
Complications after the use of ICM include hypersensitivity reactions (HSRs), which can be either immediate or non-immediate [1], and post-contrast acute kidney injury (PC-AKI), typified by a deterioration of renal function after intravascular injection of ICM and associated with increased morbidity, mortality, and longer hospital stay especially in patients with chronic kidney disease (CKD) [2,3,4,5].
Whether the incidence of adverse drug reactions (ADRs) and specifically HSRs is higher after IA or IV administration of ICM is still debated, and comparative studies are lacking. For instance, a nested case-control analysis of more than 133,000 patients exposed to iopromide showed that HSRs were significantly less frequent after IA administration compared to IV administration [6]. On the other hand, a phase II study showed that ADR incidence was relatively higher with IA administration of both iodixanol and iosimenol compared to IV administration [7].
In contrast with IV and IA administration with second-pass renal exposure (such as right heart, pulmonary, carotid, subclavian, brachial, coronary, mesenteric, iliac, femoral arteries administration), the ICM after IA administration with first-pass renal exposure (such as left heart, thoracic and suprarenal abdominal aorta, and renal arteries administration) reach the renal arteries in a relatively concentrated form, hence increasing PC-AKI risk [8, 9]. PC-AKI incidence may be higher in studies involving ICM IA vs. IV administration. This could be due to the fact that cardiac angiography is performed with catheters, which can dislodge athero-emboli, and the ICM dose in this procedure may be more abrupt and concentrated to the kidneys [10], especially from backflow of ICM from the coronary arteries into the aortic arch or when arch angiography or left ventriculography is part of the examination.
In part 1 of our systematic review [11], it has been shown that ADR/HSR incidence with IV ioversol (0.13–1.80%, depending on the outcome), especially those of severe intensity (0–0.02%), was among the lowest compared to other ICM. The reported PC-AKI incidence was variable (1–42%); nevertheless, ioversol exposure per se did not seem to increase PC-AKI incidence.
In this part 2, we sought to analyze the incidence of ADRs, HSRs, and PC-AKI after IA administration of ioversol and to position its safety profile among the different ICM.
Materials and methods
This systematic literature review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12]. The detailed methodology was previously published [11]. Briefly, MEDLINE (PubMed) and EMBASE (Elsevier) were systematically searched for studies published between January 1980 and May 2021 using keywords evocative of ICM–associated adverse events such as “allergic reaction,” “hypersensitivity,” “anaphylactic,” “nephrotoxicity,” and “kidney injury.”
Study selection
Clinical studies documenting IA administration of ioversol and other ICM and the presence or absence of ADRs, and/or HSRs, and/or PC-AKI were selected. Reviews, commentaries, letters, or case reports were excluded. Studies with < 5 patients were excluded. Study selection was conducted and reconciled between two independent authors. Publications were first screened based on title and abstract, then a full-text screening was performed. Additional publications were identified by cross-referencing.
Data extraction and study quality assessment
Key information, such as patient characteristics, type of procedure, number of patients, administered dose, type of safety outcome, and incidence, was extracted. When PC-AKI was the outcome of interest, its definition was also extracted.
Methodological quality of non-randomized studies was assessed as previously described [11] using a modified Newcastle-Ottawa scale (NOS) [13] with a score ranging from 0 to 8, based on eight questions related to patient selection, comparability of cohorts, and outcome assessment. Scores of 7–8 and 5–6 indicated high- and moderate-quality studies, respectively. The revised Cochrane Risk of Bias assessment tool for randomized trials (ROB 2) algorithm was used for randomized controlled trials (RCT) [13, 14]. The heterogeneity between studies reporting PC-AKI incidence was assessed using I2 statistics.
Results
Study selection
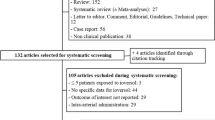
The systematic search identified 556 articles, and a full-text screening was performed for 129 articles. Twenty-eight studies were selected [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42], including four identified through citation tracking and two performed on pediatric patients [24, 28] (Fig. 1). The selected studies included 8373 patients (2412 pediatric) exposed to ioversol.
Multiple ICM were used in 10 studies [16, 23, 27, 30, 33,34,35,36, 38, 39] and seven were randomized for ICM allocation [27, 33,34,35,36, 38, 39]. In studies where the NOS was applied, three were of high quality and 19 of medium quality. RCT for ICM allocation had a low risk of bias (Table 1).
PC-AKI incidence was the main outcome studied (19 studies), while the incidence of ADRs or HSRs was studied in nine studies [28, 30, 33,34,35,36,37,38,39]. Coronary angiography was the main type of procedure (19 studies) [15,16,17,18,19,20, 22,23,24,25, 27, 28, 30,31,32, 35, 36, 39] followed by peripheral (five studies) [15, 21, 25, 33, 34] and cerebral angiography (three studies) [26, 29, 38] (Table 1).
Used ioversol dose was reported in 25 studies. The mean dose was variable in studies with adults and ranged between 29 and 232 mL (101–196 mL in diabetic patients [23, 31, 32] and 85–139 mL in CKD patients who underwent coronary angiography [15, 17, 18, 20, 27]). The mean or median dose in pediatric patients who underwent coronary angiography was ≈ 4 mL/kg [24, 28] (Table 1).
Post-contrast acute kidney injury
Almost all studies involved IA administration with second-pass renal exposure. A high heterogeneity between studies was observed (I2 = 92.04%, p < 0.0001), and the overall PC-AKI incidence was highly variable (1.5–35.5%), depending on the PC-AKI definition and studied population (Table 2). Prophylactic measures included IV hydration [15,16,17,18,19,20, 23, 24, 27, 31, 42], anti-hyperlipidemic drugs [15, 22, 42] and N-acetylcysteine administration [18, 19, 23, 27], and bicarbonate infusion [19, 20].
Post-contrast acute kidney injury in general population undergoing PCI or coronary angiography
Five studies included a general population of patients who mainly underwent percutaneous coronary intervention (PCI), and PC-AKI incidence was 7.5–21.9% [16, 19, 22, 40, 42].
In Azzalini et al [16], PC-AKI incidence with ioversol (13%) was not statistically different from that reported with other ICM (10.2–13.9%). The incidence of stage 3 PC-AKI with ioversol was 1.9% compared to 0.3–1.3% with other ICM (no statistical difference). The risk of PC-AKI requiring dialysis was nil in the ioversol group. Propensity score adjustment for multiple treatments showed that all LOCM used in this study had similar adjusted risk of PC-AKI compared to iodixanol.
In El-Saadani et al [22], patients were randomized to three groups (no load, low and high load of atorvastatin). PC-AKI was reported in seven patients (11.7%, mainly in the no-load group) and none needed dialysis.
In Fu et al [42], patients were randomized to receive or not probucol (anti-hyperlipidemic drug with antioxidant properties). PC-AKI incidence was 7.5%, and probucol + hydration was more effective in decreasing PC-AKI incidence (4% vs. 11% in the hydration group, p = 0.01). One patient in the hydration group required temporary dialysis.
In Cao et al [40], patients underwent PCI with or without upper arm remote ischemic postconditioning (RIPostC). PC-AKI incidence was 21.9%, and RIPostC was more protective against PC-AKI incidence (10% vs. 31% in the control group, p = 0.04).
Call et al [19] included patients who underwent hand or automated injection of ioversol. PC-AKI incidence was significantly lower in the automated injection group (13.3% vs. 19.3% for hand injection).
Post-contrast acute kidney injury in diabetic patients undergoing coronary angiography or PCI
PC-AKI incidence in diabetic patients who underwent coronary angiography and/or PCI was reported in five studies (4.0–26.4%) [19, 23, 27, 31, 32].
In Hernandez et al [23], where 70% of patients had an estimated glomerular filtration rate (eGFR) ≥ 60 mL/min/1.73 m2, PC-AKI incidence was 8.3% with ioversol and 2.5% with iodixanol (p = 0.047). None required dialysis. The type of ICM was found as an independent predictor of PC-AKI while ICM volume was not.
In Zaki et al [32], 78.4% of patients had an eGFR > 90 mL/min and no prophylactic measures were undertaken. PC-AKI incidence was 23.2% and none required dialysis. PC-AKI incidence in patients who underwent coronary angiography was significantly lower than in those who underwent PCI (11.4% vs. 43.5%, respectively).
In Wróbel et al [31], PC-AKI incidence was comparable between patients who had oral hydration for PC-AKI prevention (4%) and those IV hydrated (5.8%). None required dialysis.
In Call et al [19], PC-AKI incidence in diabetic patients was 18.7% in the automated injection group and 23.4% in the hand injection group (p = 0.26). In Rudnick et al [27], PC-AKI incidence in diabetic patients with CKD was 26.4% with ioversol and 21.9% with iodixanol (p = 0.57).
Post-contrast acute kidney injury in CKD patients undergoing coronary angiography or PCI
PC-AKI incidence in CKD patients who underwent coronary angiography and/or PCI was reported in five studies (5.5–28.9%) [15, 17,18,19,20, 23, 27].
Rudnick et al [27] is a double-blind study where patients were randomly administered ioversol or iodixanol. Overall, PC-AKI incidence with ioversol was 23.8% compared to 21.8% with iodixanol (p = 0.78).
In Cho et al [20], patients were randomized to four prophylactic groups (Table 1). Overall PC-AKI incidence was 11%, and no significant difference was observed between the four groups.
In Baskurt et al [18], patients were randomized to three prophylactic groups: IV hydration with normal saline alone (group 1) or supplemented with N-acetylcysteine (group 2) or with N-acetylcysteine + theophylline (group 3). Overall PC-AKI incidence was 5.5% (12 patients): five patients in group 1 (6.9%) and seven in group 2 (9.6%). None needed dialysis. In Abaci et al [15], patients who underwent coronary or peripheral angiography were assigned to receive rosuvastatin or not (control group). The overall PC-AKI incidence was 7.2%, none required dialysis, and no significant difference was observed between the groups. The incidence for each indication was not provided.
In Azzalini et al [17], severe CKD patients underwent an ultra-low contrast volume PCI (ULC-PCI, n = 8, mean of 8.8 mL) or a conventional PCI (n = 103, 90 mL). No cases of PC-AKI were reported in the ULC-PCI group. PC-AKI incidence in the conventional PCI group was 15.5%. Dialysis was needed in five patients (4.9%). The difference in PC-AKI incidence between the two groups was not statistically significant.
In Hernandez et al [23], PC-AKI incidence in diabetic patients with CKD was 17.1% with ioversol (vs. 4.9% with iodixanol, p = 0.082). In Call et al [19], PC-AKI incidence in CKD patients was 21.6–28.9% depending on the injection group.
Post-contrast acute kidney injury in pediatric patients undergoing coronary angiography
In Hirsch et al [24], PC-AKI in pediatric patients with congenital heart disease undergoing coronary angiography was reported in 11 patients (12%) (sCr change ≥ 50% at 6 h in five patients and at 24 h post-procedure in six patients).
Post-contrast acute kidney injury in patients undergoing direct renal stenting
In Komenda et al [25], PC-AKI incidence in CKD patients who underwent stenting of renal artery stenosis (77%) or coronary angiography (23%) was 9.1% and none required dialysis.
Post-contrast acute kidney injury in other indications
Four studies investigated PC-AKI incidence in other angiographic procedures [21, 26, 29, 41].
Cury et al [21], included patients who underwent lower limb angiography for critical limb ischemia. All patients were IV hydrated with a normal saline solution before and after the procedure. Overall, 69% of the patients were diabetic and 21.4% had a stage 3 CKD. PC-AKI incidence was 35.5% and none required dialysis.
Sharma et al [29] included patients who underwent endovascular treatment for acute ischemic stroke. Overall, 25% of patients were diabetic and 16% had CKD. PC-AKI was reported in three patients (1.5%) including one who had CKD.
In Krol et al [26], patients undergoing cerebral angiography had a PC-AKI incidence of 3% and none required dialysis.
In Xu et al [41], PC-AKI incidence in patients undergoing angiography was 8% using a sCr–based definition and 24% with a serum cystatin C (sCys C)–based definition. None required dialysis.
Other safety outcomes
Nine studies reported other safety outcomes [28, 30, 33,34,35,36,37,38,39]. In seven small studies of ioversol clinical development (310 patients) [33,34,35,36,37,38,39], ADRs were reported in five patients (1.6%) and consisted of urticaria, nausea, angina (one patient each), angina and chills in one patient (doubtfully related to contrast), dizziness and blurred vision in another patient. Incidence was comparable to that reported with other non-ionic LOCM (Table 3).
In Sohn et al [30], the incidence of immediate HSRs in patients who underwent coronary angiography was 2.7% and 5.3% and that of delayed HSRs was 12.5% and 18.8% (p = 0.022) with ioversol and iodixanol, respectively. Two severe HSRs were reported and PC-AKI incidence was 0.7%, but no difference between the two ICM was reported.
Senthilnathan et al [28] included pediatric patients requiring coronary angiography with or without intervention. ADRs possibly related to ioversol were reported in two patients (0.09%): dizziness, slurred speech, and amnesia in a 13-year-old patient, and PC-AKI in a 1-day-old patient.
Discussion
In this systematic review investigating the incidence of ADRs, HSRs, and PC-AKI after IA administration of ioversol, most of the selected studies focused on PC-AKI incidence after IA administration with second-pass renal exposure.
PC-AKI incidence after IA administration of ioversol was highly variable and ranged between 1.5 and 35.5%. This could be due to several factors such as the study design, clinical practice according to different countries, studied populations (general population, CKD or diabetic patients), indication (coronary angiography with or without intervention, cerebral or peripheral angiography), and, finally, the variety of definitions used in these studies.
In patients who underwent coronary angiography with or without PCI with ioversol, PC-AKI incidence was 7.5–21.9% in a general population, 4.0–26.4% in diabetic patients, and 5.5–28.9% in patients with CKD. PC-AKI incidence was comparable in three of four studies using multiple ICM. The fourth study [23] had a major limitation as patients were not treated within the same period. One comparative study using ioversol, iohexol, and iopamidol showed a similar rate of PC-AKI readmission within 30 days (i.e., 0.1%) [43]. A recent review [5] reported PC-AKI incidences of 2.7–15% in patients undergoing coronary angiography with or without PCI and 3.2–20.6%. in patients undergoing PCI, similar to the incidences reported with ioversol.
A similar high variability in PC-AKI incidence was reported after IV administration of ioversol (1–42%) [11]. This heterogeneity was due to the same reasons as those described above for IA administration, and is therefore limiting the possibility to draw conclusions regarding the two administration routes. Nevertheless, as most selected studies for this review involved second-pass renal exposure, differences in PC-AKI incidence with IV administration are not expected. In patients who underwent IV or IA iobitridol administration, PC-AKI was more frequent in those who underwent cardiac catheterization angiography (13.2%) compared to coronary CT angiography (5.6%) [44]. Conversely, other studies with patients who underwent IA diagnostic or interventional procedures and IV contrast-enhanced CT showed no difference in PC-AKI incidence [45,46,47,48,49]. Overall, this is supporting the idea that the risk of PC-AKI is similar between IV and IA administration with second-pass renal exposure.
It is clear that renal impairment is the most important risk factor for PC-AKI [10, 50]. In the past, diabetes per se was not considered as an independent risk factor for PC-AKI [8, 51, 52]. In a recent meta-analysis of 1.1 million contrast-exposed patients, diabetes mellitus was significantly associated with PC-AKI in CKD patients but not in patients with normal renal function [53]. These results suggest that appropriate PC-AKI prophylactic measures should be taken in diabetic patients with renal impairment (e.g., IV bicarbonate and/or saline hydration, withholding metformin) [54].
Few studies have specifically examined PC-AKI in pediatric populations. One case of PC-AKI was reported in a 1-day-old patient by Senthilnathan et al [28]. However, the authors identified other factors such as gentamicin and diuretics administration that could have contributed to the renal dysfunction in addition to the high ioversol dose, which may reflect the complexity of the procedure.
A low incidence of PC-AKI after cerebral angiography (1.5–3%) was reported with ioversol. The proportion of patients with CKD was low (0.9%) in one study [26] and represented 16% of all patients in the second study, with a PC-AKI incidence in these CKD patients of 3.2% [29]. Other studies performed on CKD patients showed PC-AKI incidences between 0.54 and 20.3%, depending on the ICM used (iodixanol, iopamidol, iohexol, or iomeprol) [55,56,57]. Thus, it could be reasonably concluded that PC-AKI incidence is low in patients receiving ioversol for cerebral angiography.
PC-AKI incidence was higher (35.5%) in patients who underwent lower limb angiography for critical limb ischemia with ioversol [21]. Likewise, a systematic review with more than 11,300 patients highlighted high incidences of PC-AKI for this type of procedures (range 0–45% and median of 10%) [58].
PC-AKI requiring dialysis was rare and mainly reported in patients with severe CKD [17], consistent with what has been reported with other ICM (0.3–1.5%) [16, 43, 59,60,61].
A meta-analysis showed that the risk of PC-AKI after IA administration was not significantly lower with iodixanol, overall and in CKD patients [62]. Another showed significant PC-AKI risk reduction using the sCr increase definition “≥ 0.5 mg/dL” but not “≥ 25%” [63]. Moreover, both studies showed reduced PC-AKI risk with iodixanol as compared to iohexol. However, it is not clear whether the IOCM iodixanol is different from other LOCM regarding clinical outcomes such as the need for hemodialysis, progression of CKD, rehospitalization, or mortality.
Only few studies investigated HSR incidence after IA administration of ioversol. HSR incidences after IA administration were higher than those reported in studies with IV administration of ioversol (0.2–1.8%) [11]. In contrast, a study with > 152,000 patients from four pooled observational studies with iopromide showed that HSR incidence was significantly more frequent after IV administration (0.7% vs. 0.2% with IA administration) [6]. The median ADR incidence calculated from ioversol clinical development studies was 1.7% for IA procedures, comparable to that reported with IV procedures [11]. In pediatric patients, ADR incidence after IA administration of ioversol (0.09%) [28] was lower than reported with IV administration (0.38%) [64]. However, due to the limited number of studies, it is difficult to infer whether ADR and HSR incidences are different between IA and IV administration.
This study comes with some limitations. Only one study reported the incidence of HSRs after IA administration of ioversol. Nevertheless, the incidence of ADRs reported in several studies was low and comparable to that of other LOCM. Regarding PC-AKI, only three studies used other ICMs in addition to ioversol, of which only one was a RCT. Therefore, we were unable to compare the incidence of PC-AKI between ioversol and other ICM within selected studies. PC-AKI incidences were highly variable due, inter alia, to various definitions used in the selected studies and the analyzed patients’ populations. However, analysis of the literature did not highlight differences between ioversol and other LOCM. Data on pediatric populations are limited as only two studies were identified with relevant data.
In conclusion, PC-AKI incidence after IA administration of ioversol was highly variable between studies and reflects the heterogeneity of the included study populations. Nevertheless, PC-AKI incidence appears comparable to what has been reported in the literature with other ICM and PC-AKI requiring dialysis was mainly reported in patients with severe CKD. The rate of other outcomes appears to be low, therefore highlighting the good safety profile of ioversol. Well-designed studies are needed for a better comparison with other ICM, for evaluation of other safety endpoints, and in pediatric populations.
Abbreviations
- ADR:
-
Adverse drug reaction
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- HSR:
-
Hypersensitivity reaction
- IA:
-
Intra-arterial
- ICM:
-
Iodinated contrast medium
- IV:
-
Intravenous
- LOCM:
-
Low-osmolar contrast medium
- NOS:
-
Newcastle-Ottawa scale
- PC-AKI:
-
Post-contrast acute kidney injury
- PCI:
-
Percutaneous coronary intervention
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT:
-
Randomized controlled trial
- RIPostC:
-
Remote ischemic postconditioning
- ROB 2:
-
Revised Cochrane Risk of Bias assessment tool for randomized trials
- sCr:
-
Serum creatinine
- sCysC:
-
Serum cystatin C
References
Demoly P, Adkinson NF, Brockow K et al (2014) International consensus on drug allergy. Allergy 69:420–437
Kooiman J, Pasha SM, Zondag W et al (2012) Meta-analysis: serum creatinine changes following contrast enhanced CT imaging. Eur J Radiol 81:2554–2561
Rao QA, Newhouse JH (2006) Risk of nephropathy after intravenous administration of contrast material: a critical literature analysis. Radiology 239:392–397
From AM, Bartholmai BJ, Williams AW, Cha SS, McDonald FS (2008) Mortality associated with nephropathy after radiographic contrast exposure. Mayo Clin Proc 83:1095–1100
Azzalini L, Kalra S (2020) Contrast-induced acute kidney injury-definitions, epidemiology, and implications. Interv Cardiol Clin 9:299–309
Endrikat J, Michel A, Kölbach R, Lengsfeld P, Vogtländer K (2020) Risk of hypersensitivity reactions to iopromide after intra-arterial versus intravenous administration: a nested case-control analysis of 133,331 patients. Invest Radiol 55:38–44
Meurer K, Laniado M, Hosten N, Kelsch B, Hogstrom B (2015) Intra-arterial and intravenous applications of Iosimenol 340 injection, a new non-ionic, dimeric, iso-osmolar radiographic contrast medium: phase 2 experience. Acta Radiol 56:702–708
van der Molen AJ, Reimer P, Dekkers IA et al (2018) Post-contrast acute kidney injury - part 1: definition, clinical features, incidence, role of contrast medium and risk factors: recommendations for updated ESUR Contrast Medium Safety Committee guidelines. Eur Radiol 28:2845–2855
Everson M, Sukcharoen K, Milner Q (2020) Contrast-associated acute kidney injury. BJA Educ 20:417–423
American College of Radiology, Reston, VA. ACR Manual on Contrast Media, Version 2021. Available at: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf. Accessed: 8/11/2021.
van der Molen AJ, Dekkers IA, Bedioune I, Darmon-Kern E (2021) A systematic review of the incidence of hypersensitivity reactions and post-contrast acute kidney injury after ioversol in more than 57,000 patients: part 1 - intravenous administration. Eur Radiol EURA-D-21-02907
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
GA Wells BS, D O'Connell, J Peterson, V Welch, M Losos, P Tugwell (2020) The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available via http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 19/10/2020
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Abaci O, Arat Ozkan A, Kocas C et al (2015) Impact of rosuvastatin on contrast-induced acute kidney injury in patients at high risk for nephropathy undergoing elective angiography. Am J Cardiol 115:867–871
Azzalini L, Vilca LM, Lombardo F et al (2018) Incidence of contrast-induced acute kidney injury in a large cohort of all-comers undergoing percutaneous coronary intervention: comparison of five contrast media. Int J Cardiol 273:69–73
Azzalini L, Laricchia A, Regazzoli D et al (2019) Ultra-low contrast percutaneous coronary intervention to minimize the risk for contrast-induced acute kidney injury in patients with severe chronic kidney disease. J Invasive Cardiol 31:176–182
Baskurt M, Okcun B, Abaci O et al (2009) N-Acetylcysteine versus N-acetylcysteine + theophylline for the prevention of contrast nephropathy. Eur J Clin Invest 39:793–799
Call J, Sacrinty M, Applegate R et al (2006) Automated contrast injection in contemporary practice during cardiac catheterization and PCI: effects on contrast-induced nephropathy. J Invasive Cardiol 18:469–474
Cho R, Javed N, Traub D, Kodali S, Atem F, Srinivasan V (2010) Oral hydration and alkalinization is noninferior to intravenous therapy for prevention of contrast-induced nephropathy in patients with chronic kidney disease. J Interv Cardiol 23:460–466
Cury MVM, Matielo MF, Brochado Neto FC et al (2018) The incidence, risk factors, and outcomes of contrast-induced nephropathy in patients with critical limb ischemia following lower limb angiography. Angiology 69:700–708
El-saadani R, Ibrahim O, El-Haggar S, Khalel S (2017) Outcomes of different pre-procedural loading doses of atorvastatin in patients undergoing elective percutaneous coronary intervention. Int J Pharm Sci Rev Res 45:153–160
Hernández F, Mora L, García-Tejada J et al (2009) Comparison of iodixanol and ioversol for the prevention of contrast-induced nephropathy in diabetic patients after coronary angiography or angioplasty. Rev Esp Cardiol 62:1373–1380
Hirsch R, Dent C, Pfriem H et al (2007) NGAL is an early predictive biomarker of contrast-induced nephropathy in children. Pediatr Nephrol 22:2089–2095
Komenda P, Zalunardo N, Burnett S et al (2007) Conservative outpatient renoprotective protocol in patients with low GFR undergoing contrast angiography: a case series. Clin Exp Nephrol 11:209–213
Krol AL, Dzialowski I, Roy J et al (2007) Incidence of radiocontrast nephropathy in patients undergoing acute stroke computed tomography angiography. Stroke 38:2364–2366
Rudnick MR, Davidson C, Laskey W, Stafford JL, Sherwin PF, VALOR Trial Investigators (2008) Nephrotoxicity of iodixanol versus ioversol in patients with chronic kidney disease: the Visipaque Angiography/Interventions with Laboratory Outcomes in Renal Insufficiency (VALOR) Trial. Am Heart J 156:776–782
Senthilnathan S, Gauvreau K, Marshall AC, Lock JE, Bergersen L (2009) Contrast administration in pediatric cardiac catheterization: dose and adverse events. Catheter Cardiovasc Interv 73:814–820
Sharma J, Nanda A, Jung RS, Mehta S, Pooria J, Hsu DP (2013) Risk of contrast-induced nephropathy in patients undergoing endovascular treatment of acute ischemic stroke. J Neurointerv Surg 5:543–545
Sohn K-H, Kim G-W, Lee S-Y et al (2019) Immediate and delayed hypersensitivity after intra-arterial injection of iodinated contrast media: a prospective study in patients with coronary angiography. Eur Radiol 29:5314–5321
Wróbel W, Sinkiewicz W, Gordon M, Woźniak-Wiśniewska A (2010) Oral versus intravenous hydration and renal function in diabetic patients undergoing percutaneous coronary interventions. Kardiol Pol 68:1015–1020
Zaki T, Samir A, Mohammed Rashid T, Galal H, Samir W (2015) Assessment of estimated GFR and clinical predictors of contrast induced nephropathy among diabetic patients undergoing cardiac catheterization. Egypt Heart J 67:249–258
Cutcliff WB, Schwarten DE (1989) A double-blind comparative study of the safety, tolerability, and efficacy of ioversol and iohexol in peripheral and visceral arteriography. Invest Radiol 24(Suppl 1):S56–S59
Grassi CJ, Bettmann MA, Finkelstein J, Reagan K (1989) Ioversol. Double-blind study of a new low osmolar contrast agent for peripheral and visceral arteriography. Invest Radiol 24:133–137
Hirshfeld JW, Wieland J, Davis CA et al (1989) Hemodynamic and electrocardiographic effects of ioversol during cardiac angiography. Comparison with iopamidol and diatrizoate. Invest Radiol 24:138–144
McGaughey MD, Remetz MS, Sharf-Bornhofen E (1991) A double-blind study comparing the safety, tolerability, and efficacy of ioversol-350 and iohexol-350 in coronary arteriography with left ventriculography. J Invasive Cardiol 3:272–277
Miller FJ, Pollei SR, Osborn AG (1989) Efficacy, safety, and tolerability of ioversol in intra-arterial digital subtraction angiography. Invest Radiol 24(Suppl 1):S52–S54
Ringel K, Kuehn J (1989) A double-blind study comparing the safety, tolerability, and efficacy of ioversol 320 and iopamidol-300 in cerebral angiography. Invest Radiol 24(Suppl 1):S48–S51
Reagan K, Bettman MA, Finkelstein J, Ganz P, Grassi CJ (1988) Double-blind study of a new nonionic contrast agent for cardiac angiography. Radiology 167:409–413
Cao B, Zhang C, Wang H, Xia M, Yang X (2018) Renoprotective effect of remote ischemic postconditioning in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Ther Clin Risk Manag 14:369–375
Xu Q, Wang NN, Duan SB et al (2017) Serum cystatin c is not superior to serum creatinine for early diagnosis of contrast-induced nephropathy in patients who underwent angiography. J Clin Lab Anal:31
Fu N, Yang S, Zhang J et al (2018) The efficacy of probucol combined with hydration in preventing contrast-induced nephropathy in patients with coronary heart disease undergoing percutaneous coronary intervention: a multicenter, prospective, randomized controlled study. Int Urol Nephrol 50:105–112
LaBounty TM, Shah M, Raman SV, Lin FY, Berman DS, Min JK (2012) Within-hospital and 30-day outcomes in 107,994 patients undergoing invasive coronary angiography with different low-osmolar iodinated contrast media. Am J Cardiol 109:1594–1599
Schönenberger E, Martus P, Bosserdt M et al (2019) Kidney injury after intravenous versus intra-arterial contrast agent in patients suspected of having coronary artery disease: a randomized trial. Radiology 292:664–672
Kooiman J, Le Haen PA, Gezgin G et al (2013) Contrast-induced acute kidney injury and clinical outcomes after intra-arterial and intravenous contrast administration: risk comparison adjusted for patient characteristics by design. Am Heart J 165:793–799.e791
McDonald JS, Leake CB, McDonald RJ et al (2016) Acute kidney injury after intravenous versus intra-arterial contrast material administration in a paired cohort. Invest Radiol 51:804–809
Tong GE, Kumar S, Chong KC et al (2016) Risk of contrast-induced nephropathy for patients receiving intravenous vs. intra-arterial iodixanol administration. Abdom Radiol (NY) 41:91–99
Karlsberg RP, Dohad SY, Sheng R, Iodixanol peripheral computed tomographic angiography study investigator panel (2011) Contrast medium-induced acute kidney injury: comparison of intravenous and intraarterial administration of iodinated contrast medium. J Vasc Interv Radiol 22:1159–1165
Chaudhury P, Armanyous S, Harb SC et al (2019) Intra-arterial versus intravenous contrast and renal injury in chronic kidney disease: a propensity-matched analysis. Nephron 141:31–40
Davenport MS, Perazella MA, Yee J et al (2020) Use of intravenous iodinated contrast media in patients with kidney disease: consensus statements from the American College of Radiology and the National Kidney Foundation. Kidney Med 2:85–93
Takahashi EA, Kallmes DF, Fleming CJ et al (2017) Predictors and outcomes of postcontrast acute kidney injury after endovascular renal artery intervention. J Vasc Interv Radiol 28:1687–1692
Shoukat S, Gowani SA, Jafferani A, Dhakam SH (2010) Contrast-induced nephropathy in patients undergoing percutaneous coronary intervention. Cardiol Res Pract 2010
Liu L, Liang Y, Li H et al (2021) Association between diabetes mellitus and contrast-associated acute kidney injury: a systematic review and meta-analysis of 1.1 million contrast exposure patients. Nephron 145: 451-461
European Society of Urogenital Radiology (2018) ESUR guidelines on contrast agents v10.0. Available via https://www.esur.org/fileadmin/content/2019/ESUR_Guidelines_10.0_Final_Version.pdf. Accessed 08/11/2021
Kim J, Male S, Jagadeesan BD, Streib C, Tummala RP (2018) Safety of cerebral angiography and neuroendovascular therapy in patients with chronic kidney disease. Neuroradiology 60:529–533
Myung JW, Kim JH, Cho J, Park I, Kim HY, Beom JH (2020) Contrast-induced acute kidney injury in radiologic management of acute ischemic stroke in the emergency setting. AJNR Am J Neuroradiol 41:632–636
Weber R, van Hal R, Stracke P, Hadisurya J, Nordmeyer H, Chapot R (2020) Incidence of acute kidney injury after computed tomography angiography±computed tomography perfusion followed by thrombectomy in patients with stroke using a postprocedural hydration protocol. J Am Heart Assoc 9:e014418
Prasad A, Ortiz-Lopez C, Khan A, Levin D, Kaye DM (2016) Acute kidney injury following peripheral angiography and endovascular therapy: a systematic review of the literature. Catheter Cardiovasc Interv 88:264–273
Gruberg L, Mehran R, Dangas G et al (2001) Acute renal failure requiring dialysis after percutaneous coronary interventions. Catheter Cardiovasc Interv 52:409–416
Tsai T-M, Chiang X-H, Liao H-C et al (2019) Computed tomography-guided dye localization for deeply situated pulmonary nodules in thoracoscopic surgery. Ann Transl Med 7: 31
Inohara T, Kohsaka S, Miyata H et al (2016) Performance and validation of the U.S. NCDR acute kidney injury prediction model in Japan. J Am Coll Cardiol 67:1715–1722
Heinrich MC, Häberle L, Müller V, Bautz W, Uder M (2009) Nephrotoxicity of iso-osmolar iodixanol compared with nonionic low-osmolar contrast media: meta-analysis of randomized controlled trials. Radiology 250:68–86
McCullough PA, Brown JR (2011) Effects of intra-arterial and intravenous iso-osmolar contrast medium (iodixanol) on the risk of contrast-induced acute kidney injury: a meta-analysis. Cardiorenal Med 1:220–234
Callahan MJ, Poznauskis L, Zurakowski D, Taylor GA (2009) Nonionic iodinated intravenous contrast material-related reactions: incidence in large urban children's hospital--retrospective analysis of data in 12,494 patients. Radiology 250:674–681
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Aart J. van der Molen.
Conflict of Interest
Ibrahim Bedioune and Elisabeth Darmon-Kern are medical writers employed by Guerbet.
Statistics and Biometry
No complex statistical methods were necessary for this paper.
Informed Consent
Written informed consent was not required for this study because only published data were used.
Ethical Approval
Institutional Review Board approval was not required because only published data were used.
Study subjects or cohorts overlap
Studies with duplicate data was excluded from this systematic review.
Methodology
• Multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Part 1 of this article can be found under https://doi.org/10.1007/s00330-022-08636-3.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Molen, A.J., Dekkers, I.A., Bedioune, I. et al. A systematic review of the incidence of hypersensitivity reactions and post-contrast acute kidney injury after ioversol: part 2—intra-arterial administration. Eur Radiol 32, 5546–5558 (2022). https://doi.org/10.1007/s00330-022-08637-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08637-2