Abstract
Objectives
To compare the diagnostic accuracy of 2-[18F]fluoro-2-deoxy-d-glucose-enhanced positron emission tomography (2-[18F]FDG-PET) and diffusion-weighted magnetic resonance imaging (DW-MRI) for the detection of bone marrow metastases in children and young adults with solid malignancies.
Methods
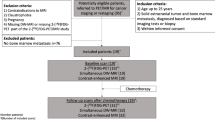
In this cross-sectional single-center institutional review board-approved study, we investigated twenty-three children and young adults (mean age, 16.8 years ± 5.1 [standard deviation]; age range, 7–25 years; 16 males, 7 females) with 925 bone marrow metastases who underwent 66 simultaneous 2-[18F]FDG-PET and DW-MRI scans including 23 baseline scans and 43 follow-up scans after chemotherapy between May 2015 and July 2020. Four reviewers evaluated all foci of bone marrow metastasis on 2-[18F]FDG-PET and DW-MRI to assess concordance and measured the tumor-to-bone marrow contrast. Results were assessed with a one-sample Wilcoxon test and generalized estimation equation. Bone marrow biopsies and follow-up imaging served as the standard of reference.
Results
The reviewers detected 884 (884/925, 95.5%) bone marrow metastases on 2-[18F]FDG-PET and 893 (893/925, 96.5%) bone marrow metastases on DW-MRI. We found different “blind spots” for 2-[18F]FDG-PET and MRI: 2-[18F]FDG-PET missed subcentimeter lesions while DW-MRI missed lesions in small bones. Sensitivity and specificity were 91.0% and 100% for 18F-FDG-PET, 89.1% and 100.0% for DW-MRI, and 100.0% and 100.0% for combined modalities, respectively. The diagnostic accuracy of combined 2-[18F]FDG-PET/MRI (100.0%) was significantly higher compared to either 2-[18F]FDG-PET (96.9%, p < 0.001) or DW-MRI (96.3%, p < 0.001).
Conclusions
Both 2-[18F]FDG-PET and DW-MRI can miss bone marrow metastases. The combination of both imaging techniques detected significantly more lesions than either technique alone.
Key Points
• DW-MRI and 2-[18F]FDG-PET have different strengths and limitations for the detection of bone marrow metastases in children and young adults with solid tumors.
• Both modalities can miss bone marrow metastases, although the “blind spot” of each modality is different.
• A combined PET/MR imaging approach will achieve maximum sensitivity and specificity for the detection of bone marrow metastases in children with solid tumors.





Similar content being viewed by others
Abbreviations
- 2-[18F]FDG-PET:
-
2-[18F]fluoro-2-deoxy-d-glucose-enhanced positron emission tomography
- ADC:
-
Apparent diffusion coefficient
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DNA:
-
Deoxyribonucleic acid
- DWI:
-
Diffusion-weighted imaging
- EANM:
-
European Association of Nuclear Medicine
- FOV:
-
Field of view
- GEE:
-
Generalized estimation equation
- GLMM:
-
Generalized linear mixed model
- IRB:
-
Institutional review board
- LAVA:
-
Liver acquisition with volume acquisition
- MIBG:
-
Metaiodobenzylguanidine
- MRI:
-
Magnetic resonance imaging
- NCCN:
-
National Comprehensive Cancer Network
- NHL:
-
Non-Hodgkin lymphomas
- OSEM:
-
Ordered subset expectation maximization
- ROI:
-
Regions of interest
- SD:
-
Standard deviation
- SNMMI:
-
Society of Nuclear Medicine and Molecular Imaging
- SNR:
-
Signal to noise ratio
- SUV:
-
Standardized uptake value
- TE:
-
Echo time
- TR:
-
Repetition time
References
Weiss AR, Lyden ER, Anderson JR et al (2013) Histologic and clinical characteristics can guide staging evaluations for children and adolescents with rhabdomyosarcoma: a report from the Children’s Oncology Group Soft Tissue Sarcoma Committee. J Clin Oncol 31:3226–3232
Cotterill SJ, Ahrens S, Paulussen M et al (2000) Prognostic factors in Ewing’s tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing’s Sarcoma Study Group. J Clin Oncol 18:3108–3114
Levis A, Pietrasanta D, Godio L et al (2004) A large-scale study of bone marrow involvement in patients with Hodgkin’s lymphoma. Clin Lymphoma 5:50–55
Oberlin O, Rey A, Lyden E et al (2008) Prognostic factors in metastatic rhabdomyosarcomas: results of a pooled analysis from United States and European cooperative groups. J Clin Oncol 26:2384–2389
Paulussen M, Ahrens S, Burdach S et al (1998) Primary metastatic (stage IV) Ewing tumor: survival analysis of 171 patients from the EICESS studies. European Intergroup Cooperative Ewing Sarcoma Studies. Ann Oncol 9:275–281
Balamuth NJ, Womer RB (2010) Ewing’s sarcoma. Lancet Oncol 11:184–192
Cesari M, Righi A, Colangeli M et al (2019) Bone marrow biopsy in the initial staging of Ewing sarcoma: experience from a single institution. Pediatr Blood Cancer 66:e27653
Cheng G, Alavi A (2013) Value of 18F-FDG PET versus iliac biopsy in the initial evaluation of bone marrow infiltration in the case of Hodgkin’s disease: a meta-analysis. Nucl Med Commun 34:25–31
Wang Y, Xie L, Tian R et al (2019) PET/CT-based bone-marrow assessment shows potential in replacing routine bone-marrow biopsy in part of patients newly diagnosed with extranodal natural killer/T-cell lymphoma. J Cancer Res Clin Oncol 145:2529–2539
Yağci-Küpeli B, Koçyiğit-Deveci E, Adamhasan F, Küpeli S (2019) The value of 18F-FDG PET/CT in detecting bone marrow involvement in childhood cancers. J Pediatr Hematol Oncol 41:438–441
Kaushik A, Jaimini A, Tripathi M et al (2015) Estimation of radiation dose to patients from (18) FDG whole body PET/CT investigations using dynamic PET scan protocol. Indian J Med Res 142:721–731
Chawla SC, Federman N, Zhang D et al (2010) Estimated cumulative radiation dose from PET/CT in children with malignancies: a 5-year retrospective review. Pediatr Radiol 40:681–686
Kharuzhyk S, Zhavrid E, Dziuban A, Sukolinskaja E, Kalenik O (2020) Comparison of whole-body MRI with diffusion-weighted imaging and PET/CT in lymphoma staging. Eur Radiol 30:3915–3923
Soydan L, Demir AA, Torun M, Cikrikcioglu MA (2020) Use of diffusion-weighted magnetic resonance imaging and apparent diffusion coefficient in gastric cancer staging. Curr Med Imaging 16:1278–1289
Klenk C, Gawande R, Uslu L et al (2014) Ionising radiation-free whole-body MRI versus (18)F-fluorodeoxyglucose PET/CT scans for children and young adults with cancer: a prospective, non-randomised, single-centre study. Lancet Oncol 15:275–285
Regacini R, Puchnick A, Luisi FAV, Lederman HM (2018) Can diffusion-weighted whole-body MRI replace contrast-enhanced CT for initial staging of Hodgkin lymphoma in children and adolescents? Pediatr Radiol 48:638–647
Asenbaum U, Nolz R, Karanikas G et al (2018) Bone marrow involvement in malignant lymphoma: evaluation of quantitative PET and MRI biomarkers. Acad Radiol 25:453–460
Sakurai Y, Kawai H, Iwano S, Ito S, Ogawa H, Naganawa S (2013) Supplemental value of diffusion-weighted whole-body imaging with background body signal suppression (DWIBS) technique to whole-body magnetic resonance imaging in detection of bone metastases from thyroid cancer. J Med Imaging Radiat Oncol 57:297–305
Takenaka D, Ohno Y, Matsumoto K et al (2009) Detection of bone metastases in non-small cell lung cancer patients: comparison of whole-body diffusion-weighted imaging (DWI), whole-body MR imaging without and with DWI, whole-body FDG-PET/CT, and bone scintigraphy. J Magn Reson Imaging 30:298–308
Ishiguchi H, Ito S, Kato K et al (2018) Diagnostic performance of (18)F-FDG PET/CT and whole-body diffusion-weighted imaging with background body suppression (DWIBS) in detection of lymph node and bone metastases from pediatric neuroblastoma. Ann Nucl Med 32:348–362
Park C, Lee E, Yeo Y et al (2018) Spine MR images in patients with pedicle screw fixation: comparison of conventional and SEMAC-VAT sequences at 1.5 T. Magn Reson Imaging 54:63–70
Guo H, Lan S, He Y, Tiheiran M, Liu W (2021) Differentiating brucella spondylitis from tuberculous spondylitis by the conventional MRI and MR T2 mapping: a prospective study. Eur J Med Res 26:125
Cohen J (1968) Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 70:213–220
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Cheng G, Chen W, Chamroonrat W, Torigian DA, Zhuang H, Alavi A (2011) Biopsy versus FDG PET/CT in the initial evaluation of bone marrow involvement in pediatric lymphoma patients. Eur J Nucl Med Mol Imaging 38:1469–1476
Purz S, Mauz-Körholz C, Körholz D et al (2011) [18F]Fluorodeoxyglucose positron emission tomography for detection of bone marrow involvement in children and adolescents with Hodgkin’s lymphoma. J Clin Oncol 29:3523–3528
Biermann JS, Chow W, Reed DR et al (2017) NCCN guidelines insights: bone cancer, version 2.2017. J Natl Compr Canc Netw 15:155–167
Kasalak Ö, Glaudemans A, Overbosch J, Jutte PC, Kwee TC (2018) Can FDG-PET/CT replace blind bone marrow biopsy of the posterior iliac crest in Ewing sarcoma? Skeletal Radiol 47:363–367
Chen S, Wang S, He K, Ma C, Fu H, Wang H (2018) PET/CT predicts bone marrow involvement in paediatric non-Hodgkin lymphoma and may preclude the need for bone marrow biopsy in selected patients. Eur Radiol 28:2942–2950
McCarten KM, Nadel HR, Shulkin BL, Cho SY (2019) Imaging for diagnosis, staging and response assessment of Hodgkin lymphoma and non-Hodgkin lymphoma. Pediatr Radiol 49:1545–1564
Albano D, Patti C, Lagalla R, Midiri M, Galia M (2017) Whole-body MRI, FDG-PET/CT, and bone marrow biopsy, for the assessment of bone marrow involvement in patients with newly diagnosed lymphoma. J Magn Reson Imaging 45:1082–1089
Balbo-Mussetto A, Saviolo C, Fornari A et al (2017) Whole body MRI with qualitative and quantitative analysis of DWI for assessment of bone marrow involvement in lymphoma. Radiol Med 122:623–632
Sun W, Li M, Gu Y, Sun Z, Qiu Z, Zhou Y (2020) Diagnostic value of whole-body DWI with background body suppression plus calculation of apparent diffusion coefficient at 3 T versus (18)F-FDG PET/CT for detection of bone metastases. AJR Am J Roentgenol 214:446–454
Lin C, Luciani A, Itti E et al (2010) Whole-body diffusion-weighted magnetic resonance imaging with apparent diffusion coefficient mapping for staging patients with diffuse large B-cell lymphoma. Eur Radiol 20:2027–2038
Badr S, Kotb M, Elahmadawy MA, Moustafa H (2018) Predictive value of FDG PET/CT versus bone marrow biopsy in pediatric lymphoma. Clin Nucl Med 43:e428–e438
Kernstine KH, Grannis FW Jr, Rotter AJ (2005) Is there a role for PET in the evaluation of subcentimeter pulmonary nodules? Semin Thorac Cardiovasc Surg 17:110–114
Muehe AM, Siedek F, Theruvath AJ et al (2020) Differentiation of benign and malignant lymph nodes in pediatric patients on ferumoxytol-enhanced PET/MRI. Theranostics 10:3612–3621
Hirsch FW, Sattler B, Sorge I et al (2013) PET/MR in children. Initial clinical experience in paediatric oncology using an integrated PET/MR scanner. Pediatr Radiol 43:860–875
Sher AC, Seghers V, Paldino MJ et al (2016) Assessment of sequential PET/MRI in comparison with PET/CT of pediatric lymphoma: a prospective study. AJR Am J Roentgenol 206:623–631
Danylesko I, Shouval R, Shem-Tov N et al (2020) Immune imitation of tumor progression after anti-CD19 chimeric antigen receptor T cells treatment in aggressive B-cell lymphoma. Bone Marrow Transplant. https://doi.org/10.1038/s41409-020-01156-y
Huang J, Rong L, Wang E, Fang Y (2021) Pseudoprogression of extramedullary disease in relapsed acute lymphoblastic leukemia after CAR T-cell therapy. Immunotherapy 13:5–10
Høilund-Carlsen PF, Hess S, Werner TJ, Alavi A (2018) Cancer metastasizes to the bone marrow and not to the bone: time for a paradigm shift! Eur J Nucl Med Mol Imaging 45:893–897
Van der Woude HJ, Hazelbag HM, Bloem JL, Taminiau AH, Hogendoorn PC (2004) MRI of adamantinoma of long bones in correlation with histopathology. AJR Am J Roentgenol 183:1737–1744
Greenspan A, Norman A (1988) Osteolytic cortical destruction: an unusual pattern of skeletal metastases. Skeletal Radiol 17:402–406
Padhani AR, van Ree K, Collins DJ, D’Sa S, Makris A (2013) Assessing the relation between bone marrow signal intensity and apparent diffusion coefficient in diffusion-weighted MRI. AJR Am J Roentgenol 200:163–170
Koh DM, Collins DJ (2007) Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol 188:1622–1635
Rezaeian A, Tahmasebi Birgani MJ, Chegeni N, Sarkarian M, Hanafi MGh, Akbarizadeh Gh (2019) Signal intensity of high B-value diffusion-weighted imaging for the detection of prostate cancer. J Biomed Phys Eng 9:453–458
Truong MT, Erasmus JJ, Munden RF et al (2004) Focal FDG uptake in mediastinal brown fat mimicking malignancy: a potential pitfall resolved on PET/CT. AJR Am J Roentgenol 183:1127–1132
Yeung HW, Grewal RK, Gonen M, Schöder H, Larson SM (2003) Patterns of (18)F-FDG uptake in adipose tissue and muscle: a potential source of false-positives for PET. J Nucl Med 44:1789–1796
Daldrup-Link HE, Franzius C, Link TM et al (2001) Whole-body MR imaging for detection of bone metastases in children and young adults: comparison with skeletal scintigraphy and FDG PET. AJR Am J Roentgenol 177:229–236
Vali R, Alessio A, Balza R et al (2021) SNMMI procedure standard/EANM practice guideline on pediatric (18)F-FDG PET/CT for oncology 1.0. J Nucl Med 62:99–110
Ohnona J, Michaud L, Balogova S et al (2013) Can we achieve a radionuclide radiation dose equal to or less than that of 99mTc-hydroxymethane diphosphonate bone scintigraphy with a low-dose 18F-sodium fluoride time-of-flight PET of diagnostic quality? Nucl Med Commun 34:417–425
Klega K, Imamovic-Tuco A, Ha G et al (2018) Detection of somatic structural variants enables quantification and characterization of circulating tumor DNA in children with solid tumors. JCO Precis Oncol 2018
Acknowledgements
We thank Dawn Holley, Kim Halbert, and Mehdi Khalighi from the PET/MRI Metabolic Service Center for their assistance with the acquisition of PET/MRI scans at the Lucas Research Center at Stanford. We thank Hasti Gholami for her help in the preparation of Figure 2. We thank the members of the Daldrup-Link lab for valuable input and discussions regarding this project.
Funding
This work was in part supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, grant number R01 HD081123.
Statistical analysis for this work was also partially supported by the Biostatistics Shared Resources, which is funded by the Cancer Center Support Grant, P30CA124435.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Heike E. Daldrup-Link.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Dr. Rong Lu (Stanford University School of Medicine) has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained (IRB20221 and IRB44706).
Methodology
• prospective
• cross-sectional study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rashidi, A., Baratto, L., Theruvath, A.J. et al. Diagnostic Accuracy of 2-[18F]FDG-PET and whole-body DW-MRI for the detection of bone marrow metastases in children and young adults. Eur Radiol 32, 4967–4979 (2022). https://doi.org/10.1007/s00330-021-08529-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08529-x