Abstract
Objective
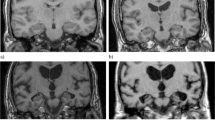
To evaluate the diagnostic performance and reliability of the medial temporal lobe atrophy (MTA) scale in patients with Alzheimer’s disease.
Methods
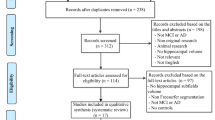
A systematic literature search of MEDLINE and EMBASE databases was performed to select studies that evaluated the diagnostic performance or reliability of MTA scale, published up to January 21, 2021. Pooled estimates of sensitivity and specificity were calculated using a bivariate random-effects model. Pooled correlation coefficients for intra- and interobserver agreements were calculated using the random-effects model based on Fisher’s Z transformation of correlations. Meta-regression was performed to explain the study heterogeneity. Subgroup analysis was performed to compare the diagnostic performance of the MTA scale and hippocampal volumetry.
Results
Twenty-one original articles were included. The pooled sensitivity and specificity of the MTA scale in differentiating Alzheimer’s disease from healthy control were 74% (95% CI, 68–79%) and 88% (95% CI, 83–91%), respectively. The area under the curve of the MTA scale was 0.88 (95% CI, 0.84–0.90). Meta-regression demonstrated that the difference in the method of rating the MTA scale was significantly associated with study heterogeneity (p = 0.04). No significant difference was observed in five studies regarding the diagnostic performance between MTA scale and hippocampal volumetry (p = 0.40). The pooled correlation coefficients for intra- and interobserver agreements were 0.85 (95% CI, 0.69–0.93) and 0.83 (95% CI, 0.66–0.92), respectively.
Conclusions
Our meta-analysis demonstrated a good diagnostic performance and reliability of the MTA scale in Alzheimer’s disease.
Key Points
• The pooled sensitivity and specificity of the MTA scale in differentiating Alzheimer’s disease from healthy control were 74% and 88%, respectively.
• There was no significant difference in the diagnostic performance between MTA scale and hippocampal volumetry.
• The reliability of MTA scale was excellent based on the pooled correlation coefficient for intra- and interobserver agreements.





Similar content being viewed by others
Abbreviations
- AD:
-
Alzheimer’s disease
- CI:
-
Confidence interval
- DLB:
-
Dementia with Lewy bodies
- ESNR:
-
European Society of Neuroradiology
- FTLD:
-
Frontotemporal lobar dementia
- HC:
-
Healthy controls
- HSROC:
-
Hierarchical summary receiver operating characteristics
- MCI:
-
Mild cognitive impairment
- MTA:
-
Medial temporal lobe atrophy
- NIA-AA :
-
National Institute on Aging and Alzheimer's Association
- SCD:
-
Subjective cognitive decline
References
Nichols E, Szoeke CE, Vollset SE et al (2019) Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18:88–106
Albert MS, DeKosky ST, Dickson D et al (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:270–279
Yiannopoulou KG, Papageorgiou SG (2020) Current and future treatments in Alzheimer disease: an update. J Cent Nerv Syst Dis 12:1179573520907397
Park M, Moon W-J (2016) Structural MR imaging in the diagnosis of Alzheimer’s disease and other neurodegenerative dementia: current imaging approach and future perspectives. Korean J Radiol 17:827
Herzog AG, Kemper TL (1980) Amygdaloid changes in aging and dementia. Arch Neurol 37:625–629
Jack CR Jr, Bennett DA, Blennow K et al (2018) NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement 14:535–562
McKhann GM, Knopman DS, Chertkow H et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269
Scheltens P, Leys D, Barkhof F et al (1992) Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. J Neurol Neurosurg Psychiatry 55:967–972
Vernooij M, Pizzini F, Schmidt R et al (2019) Dementia imaging in clinical practice: a European-wide survey of 193 centres and conclusions by the ESNR working group. Neuroradiology 61:633–642
Håkansson C, Torisson G, Londos E, Hansson O, Björkman-Burtscher IM, van Westen D (2021) Reporting frequency of radiology findings increases after introducing visual rating scales in the primary care diagnostic work up of subjective and mild cognitive impairment. Eur Radiol 31:666–673
Torisson G, van Westen D, Stavenow L, Minthon L, Londos E (2015) Medial temporal lobe atrophy is underreported and may have important clinical correlates in medical inpatients. BMC Geriatr 15:1–8
Caspers J, Heeger A, Turowski B, Rubbert C (2020) Automated age- and sex-specific volumetric estimation of regional brain atrophy: workflow and feasibility. Eur Radiol. https://doi.org/10.1007/s00330-020-07196-8
Suh C, Shim W, Kim S et al (2020) Development and validation of a deep learning–based automatic brain segmentation and classification algorithm for Alzheimer disease using 3d t1-weighted volumetric images. AJNR Am J Neuroradiol 41:2227–2234
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34:939–939
Petersen RC (2004) Mild cognitive impairment as a diagnostic entity. J Intern Med 256:183–194
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors) (2021) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from https://www.training.cochrane.org/handbook.
Suh CH, Park SH (2016) Successful publication of systematic review and meta-analysis of studies evaluating diagnostic test accuracy. Korean J Radiol 17:5–6
Devillé WL, Buntinx F, Bouter LM et al (2002) Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol 2:9
Hedges LV, Olkin I (2014) Statistical methods for meta-analysis. Academic Press
Min J, Moon W-J, Jeon JY, Choi JW, Moon Y-S, Han S-H (2017) Diagnostic efficacy of structural MRI in patients with mild-to-moderate Alzheimer disease: automated volumetric assessment versus visual assessment. AJR Am J Roentgenol 208:617–623
Bresciani L, Rossi R, Testa C et al (2005) Visual assessment of medial temporal atrophy on MR films in Alzheimer’s disease: comparison with volumetry. Aging Clin Exp Res 17:8–13
Burton EJ, Barber R, Mukaetova-Ladinska EB et al (2009) Medial temporal lobe atrophy on MRI differentiates Alzheimer’s disease from dementia with Lewy bodies and vascular cognitive impairment: a prospective study with pathological verification of diagnosis. Brain 132:195–203
Claus JJ, Staekenborg SS, Holl DC et al (2017) Practical use of visual medial temporal lobe atrophy cut-off scores in Alzheimer’s disease: Validation in a large memory clinic population. Eur Radiol 27:3147–3155
Dhikav V, Duraiswamy S, Anand KS (2017) Correlation between hippocampal volumes and medial temporal lobe atrophy in patients with Alzheimer’s disease. Ann Indian Acad Neurol 20:29–35
Duara R, Loewenstein DA, Potter E et al (2008) Medial temporal lobe atrophy on MRI scans and the diagnosis of Alzheimer disease. Neurology 71:1986–1992
Enkirch SJ, Traschütz A, Müller A et al (2018) The ERICA score: an MR imaging-based visual scoring system for the assessment of entorhinal cortex atrophy in Alzheimer disease. Radiology 288:226–333
Ferreira D, Cavallin L, Larsson EM et al (2015) Practical cut-offs for visual rating scales of medial temporal, frontal and posterior atrophy in Alzheimer’s disease and mild cognitive impairment. J Intern Med 278:277–290
Firbank MJ, Lloyd J, Williams D et al (2016) An evidence-based algorithm for the utility of FDG-PET for diagnosing Alzheimer’s disease according to presence of medial temporal lobe atrophy. Br J Psychiatry 208:491–496
Flak MM, Hol HR, Hernes SS et al (2018) Cognitive profiles and atrophy ratings on MRI in senior patients with mild cognitive impairment. Front Aging Neurosci 10:384
Galton CJ, Gomez-Anson B, Antoun N et al (2001) Temporal lobe rating scale: application to Alzheimer’s disease and frontotemporal dementia. J Neurol Neurosurg Psychiatry 70:165–173
Lehmann M, Koedam EL, Barnes J et al (2012) Posterior cerebral atrophy in the absence of medial temporal lobe atrophy in pathologically-confirmed Alzheimer’s disease. Neurobiol Aging 33:627.e621-627.e612
O’Donovan J, Watson R, Colloby SJ et al (2013) Does posterior cortical atrophy on MRI discriminate between Alzheimer’s disease, dementia with Lewy bodies, and normal aging? Int Psychogeriatr 25:111–119
Rhodius-Meester HFM, Benedictus MR, Wattjes MP et al (2017) MRI Visual ratings of brain atrophy and white matter hyperintensities across the spectrum of cognitive decline are differently affected by age and diagnosis. Front Aging Neurosci 9:117
Ridha BH, Barnes J, van de Pol LA et al (2007) Application of automated medial temporal lobe atrophy scale to Alzheimer disease. Arch Neurol 64:849–854
Traschütz A, Enkirch SJ, Polomac N et al (2020) The entorhinal cortex atrophy score is diagnostic and prognostic in mild cognitive impairment. J Alzheimers Dis 75:99–108
Wahlund LO, Julin P, Lindqvist J, Scheltens P (1999) Visual assessment of medical temporal lobe atrophy in demented and healthy control subjects: correlation with volumetry. Psychiatry Res 90:193–199
Wei M, Shi J, Ni J et al (2019) A new age-related cutoff of medial temporal atrophy scale on MRI improving the diagnostic accuracy of neurodegeneration due to Alzheimer’s disease in a Chinese population. BMC Geriatr 19:59
Yalciner BZ, Kandemir M, Taskale S, Tepe SM, Unay D (2019) Modified visual magnetic resonance rating scale for evaluation of patients with forgetfulness. Can J Neurol Sci 46:71–78
Yuan Z, Pan C, Xiao T et al (2019) Multiple visual rating scales based on structural mri and a novel prediction model combining visual rating scales and age stratification in the diagnosis of Alzheimer’s disease in the Chinese population. Front Neurol 10:93
Van de Pol L, Scheltens P (2014) Medial temporal lobe atrophy scores translated to clinical practice: editorial comment on ‘Influence of age, disease onset and ApoE4 on visual medial temporal lobe atrophy cut-offs’’.’ J Intern Med 275:331–333
Frisoni GB, Jack CR (2011) Harmonization of magnetic resonance‐based manual hippocampal segmentation: a mandatory step for wide clinical use. Alzehimers Dement 7:171–174
Cavedo E, Pievani M, Boccardi M et al (2014) Medial temporal atrophy in early and late-onset Alzheimer’s disease. Neurobiol Aging 35:2004–2012
Jack CR Jr, Petersen RC, Xu Y et al (1998) Rate of medial temporal lobe atrophy in typical aging and Alzheimer’s disease. Neurology 51:993–999
Persson K, Barca ML, Cavallin L et al (2018) Comparison of automated volumetry of the hippocampus using NeuroQuant® and visual assessment of the medial temporal lobe in Alzheimer’s disease. Acta Radiol 59:997–1001
Hsu YY, Schuff N, Du AT et al (2002) Comparison of automated and manual MRI volumetry of hippocampus in normal aging and dementia. J Magn Reson Imaging 16:305–310
Koedam EL, Lehmann M, van der Flier WM et al (2011) Visual assessment of posterior atrophy development of a MRI rating scale. Eur Radiol 21:2618–2625
Egger K, Rau A, Yang S et al (2020) Automated voxel-and region-based analysis of gray matter and cerebrospinal fluid space in primary dementia disorders. Brain Res 1739:146800
Cajanus A, Hall A, Koikkalainen J et al (2018) Automatic MRI quantifying methods in behavioral-variant frontotemporal dementia diagnosis. Dement Geriatr Cogn Disord Extra 8:51–59
Thiagarajan S, Shaik MA, Venketasubramanian N, Ting E, Hilal S, Chen C (2018) Coronal CT is comparable to MR imaging in aiding diagnosis of dementia in a memory clinic in Singapore. Alzheimer Dis Assoc Disord 32:94–100
Buckley RF, Maruff P, Ames D et al (2016) Subjective memory decline predicts greater rates of clinical progression in preclinical Alzheimer’s disease. Alzheimers Dement 12:796–804
Peixoto-Santos JE, Carvalho LEDd, Kandratavicius L et al (2018) Manual hippocampal subfield segmentation using high-field MRI: Impact of different subfields in hippocampal volume loss of temporal lobe epilepsy patients. Front Neurol 9:927
Frankó E, Joly O, AsDN Initiative (2013) Evaluating Alzheimer’s disease progression using rate of regional hippocampal atrophy. PLoS One 8:e71354
Funding
This work was supported by the National Research Foundation of Korea (NRF-2021R1C1C1014413 to Chong Hyun Suh).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Chong Hyun Suh, M.D.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required because the article type of this study is a systematic review and meta-analysis.
Ethical approval
Institutional Review Board approval was not required because the article type of this study is a systematic review and meta-analysis.
Study subjects or cohort overlap
Some study subjects or cohorts have been previously reported in previously published articles which were included in this study.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed in one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, H.Y., Park, C.R., Suh, C.H. et al. Diagnostic performance of the medial temporal lobe atrophy scale in patients with Alzheimer’s disease: a systematic review and meta-analysis. Eur Radiol 31, 9060–9072 (2021). https://doi.org/10.1007/s00330-021-08227-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08227-8