Abstract
Objectives
2-Deoxy-2-[18F]fluoro-D-glucose ([18F]FDG) positron-emission tomography/computed tomography (PET/CT) is widely used to evaluate lung nodules, although respiratory motion artefacts may occur. We investigated the value of prone position PET/CT (pPET/CT) in lung nodule evaluation compared with standard supine position PET/CT (sPET/CT).
Methods
We retrospectively reviewed 28 consecutive patients (20 men; age, 65.6 ± 12.1 years) with a lung nodule (size, 16.8 ± 5.5 mm) located below the sub-carinal level who underwent [18F]FDG PET/CT in a standard supine position and additional prone position. The maximum standardised uptake value (SUVmax), metabolic tumour volume (MTV), difference of diaphragm position between PET and CT (DDP), Dice’s similarity coefficient (DSC) and occurrence of mis-registration were analysed. The [18F]FDG uptake of 20 biopsy-confirmed (15 malignant) nodules was evaluated visually.
Results
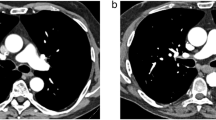
pPET/CT yielded a significantly higher SUVmax, lower MTV and shorter DDP than with sPET/CT (p = 0.043, 0.007 and 0.021, respectively). Mis-registration occurred in 53.6% of cases in sPET/CT and in 28.6% of cases in pPET/CT (p = 0.092). Among the 15 patients with mis-registration in sPET/CT, 10 patients (66.7%) did not show mis-registration in pPET/CT. DSC was higher in pPET/CT than in sPET/CT in 18 out of 28 patients (64.3%). In visual analysis, malignant nodules exhibited a higher [18F]FDG uptake positivity than benign nodules in pPET/CT (93.3% vs. 40.0%, p = 0.032) but not in sPET/CT (80.0% vs. 40.0%, p = 0.131).
Conclusions
pPET/CT reduces respiratory motion artefact and enables more-precise measurements of PET parameters.
Key Points
• In prone position PET/CT, the decrease in the blurring effect caused by reduced respiratory motion resulted in a higher SUV max and lower MTV in lung nodules than that with supine position PET/CT.
• Prone position PET/CT was useful to interpret correctly malignant lung nodules as being positive in individual cases that had a negative result in supine position PET/CT.




Similar content being viewed by others
Abbreviations
- [18F]FDG:
-
2-Deoxy-2-[18F]fluoro-D-glucose
- CT:
-
Computed tomography
- DDP:
-
Difference of diaphragm position between PET and CT
- IPF:
-
Idiopathic pulmonary fibrosis
- MTV:
-
Metabolic tumour volume
- PET/CT:
-
Positron-emission tomography/computed tomography
- PET:
-
Positron-emission tomography
- pPET/CT:
-
Prone position positron-emission tomography/computed tomography
- SD:
-
Standard deviation
- sPET/CT:
-
Supine position positron-emission tomography/computed tomography
- SUVmax :
-
Maximum standardised uptake value
References
Cronin P, Dwamena BA, Kelly AM, Bernstein SJ, Carlos RC (2008) Solitary pulmonary nodules and masses: A meta-analysis of the diagnostic utility of alternative imaging tests. Eur Radiol 18:1840–1856
Divisi D, Barone M, Bertolaccini L, Zaccagna G, Gabriele F, Crisci R (2018) Diagnostic performance of fluorine-18 fluorodeoxyglucose positron emission tomography in the management of solitary pulmonary nodule: A meta-analysis. J Thorac Dis 10:S779–s789
Jia Y, Gong W, Zhang Z et al (2019) Comparing the diagnostic value of (18)F-FDG-PET/CT versus CT for differentiating benign and malignant solitary pulmonary nodules: A meta-analysis. J Thorac Dis 11:2082–2098
Li ZZ, Huang YL, Song HJ, Wang YJ, Huang Y (2018) The value of 18F-FDG-PET/CT in the diagnosis of solitary pulmonary nodules: A meta-analysis. Medicine (Baltimore) 97:e0130
Ruilong Z, Daohai X, Li G, Xiaohong W, Chunjie W, Lei T (2017) Diagnostic value of 18F-FDG-PET/CT for the evaluation of solitary pulmonary nodules: A systematic review and meta-analysis. Nucl Med Commun 38:67–75
Bueno J, Landeras L, Chung JH (2018) Updated Fleischner Society guidelines for managing incidental pulmonary nodules: Common questions and challenging scenarios. Radiographics 38:1337–1350
Osman MM, Cohade C, Nakamoto Y, Wahl RL (2003) Respiratory motion artifacts on PET emission images obtained using CT attenuation correction on PET-CT. Eur J Nucl Med Mol Imaging 30:603–606
Allen-Auerbach M, Yeom K, Park J, Phelps M, Czernin J (2006) Standard PET/CT of the chest during shallow breathing is inadequate for comprehensive staging of lung cancer. J Nucl Med 47:298–301
Erdi YE, Nehmeh SA, Pan T et al (2004) The CT motion quantitation of lung lesions and its impact on PET-measured SUVs. J Nucl Med 45:1287–1292
Farid K, Poullias X, Alifano M et al (2015) Respiratory-gated imaging in metabolic evaluation of small solitary pulmonary nodules: 18F-FDG PET/CT and correlation with histology. Nucl Med Commun 36:722–727
Guerra L, De Ponti E, Elisei F et al (2012) Respiratory gated PET/CT in a European multicentre retrospective study: Added diagnostic value in detection and characterization of lung lesions. Eur J Nucl Med Mol Imaging 39:1381–1390
Van Der Gucht A, Serrano B, Hugonnet F, Paulmier B, Garnier N, Faraggi M (2014) Impact of a new respiratory amplitude-based gating technique in evaluation of upper abdominal PET lesions. Eur J Radiol 83:509–515
Pepin A, Daouk J, Bailly P, Hapdey S, Meyer ME (2014) Management of respiratory motion in PET/computed tomography: The state of the art. Nucl Med Commun 35:113–122
Walker MD, Morgan AJ, Bradley KM, McGowan DR (2020) Data driven respiratory gating outperforms device-based gating for clinical FDG PET/CT. J Nucl Med. https://doi.org/10.2967/jnumed.120.242248
Büther F, Jones J, Seifert R, Stegger L, Schleyer P, Schäfers M (2020) Clinical evaluation of a data-driven respiratory gating algorithm for whole-body PET with continuous bed motion. J Nucl Med 61:1520–1527
Manna EM, Ibraheim OA, Samarkandi AH, Alotaibi WM, Elwatidy SM (2005) The effect of prone position on respiratory mechanics during spinal surgery. Middle East J Anaesthesiol 18:623–630
Nam Y, Yoon AM, Kim YH, Yoon SH (2010) The effect on respiratory mechanics when using a Jackson surgical table in the prone position during spinal surgery. Korean J Anesthesiol 59:323–328
Senay H, Sivaci R, Kokulu S, Koca B, Baki ED, Ela Y (2016) The effect of pressure-controlled ventilation and volume-controlled ventilation in prone position on pulmonary mechanics and inflammatory markers. Inflammation 39:1469–1474
Cohade C, Osman M, Marshall LN, Wahl RN (2003) PET-CT: Accuracy of PET and CT spatial registration of lung lesions. Eur J Nucl Med Mol Imaging 30:721–726
Boellaard R, Delgado-Bolton R, Oyen WJ et al (2015) FDG PET/CT: EANM procedure guidelines for tumour imaging: Version 2.0. Eur J Nucl Med Mol Imaging 42:328–354
van der Vos CS, Grootjans W, Osborne DR et al (2015) Improving the spatial alignment in PET/CT using amplitude-based respiration-gated PET and respiration-triggered CT. J Nucl Med 56:1817–1822
Hanna GG, Hounsell AR, O’Sullivan JM (2010) Geometrical analysis of radiotherapy target volume delineation: A systematic review of reported comparison methods. Clin Oncol (R Coll Radiol) 22:515–525
Meirelles GS, Erdi YE, Nehmeh SA et al (2007) Deep-inspiration breath-hold PET/CT: Clinical findings with a new technique for detection and characterization of thoracic lesions. J Nucl Med 48:712–719
Kawano T, Ohtake E, Inoue T (2008) Deep-inspiration breath-hold PET/CT of lung cancer: Maximum standardized uptake value analysis of 108 patients. J Nucl Med 49:1223–1231
Frood R, McDermott G, Scarsbrook A (2018) Respiratory-gated PET/CT for pulmonary lesion characterisation-Promises and problems. Br J Radiol 91:20170640
Balamoutoff N, Serrano B, Hugonnet F, Garnier N, Paulmier B, Faraggi M (2018) Added value of a single fast 20-second deep-inspiration breath-hold acquisition in FDG PET/CT in the assessment of lung nodules. Radiology 286:260–270
Torizuka T, Tanizaki Y, Kanno T et al (2009) Single 20-second acquisition of deep-inspiration breath-hold PET/CT: Clinical feasibility for lung cancer. J Nucl Med 50:1579–1584
García Vicente AM, Castrejón AS, León Martín AA, García BG, Pilkington Woll JP, Muñoz AP (2011) Value of 4-dimensional 18F-FDG PET/CT in the classification of pulmonary lesions. J Nucl Med Technol 39:91–99
García Vicente AM, Soriano Castrejón AM, Talavera Rubio MP et al (2010) (18)F-FDG PET-CT respiratory gating in characterization of pulmonary lesions: Approximation towards clinical indications. Ann Nucl Med 24:207–214
Werner MK, Parker JA, Kolodny GM, English JR, Palmer MR (2009) Respiratory gating enhances imaging of pulmonary nodules and measurement of tracer uptake in FDG PET/CT. AJR Am J Roentgenol 193:1640–1645
Aristophanous M, Yong Y, Yap JT et al (2012) Evaluating FDG uptake changes between pre and post therapy respiratory gated PET scans. Radiother Oncol 102:377–382
Grootjans W, de Geus-Oei LF, Meeuwis AP et al (2014) Amplitude-based optimal respiratory gating in positron emission tomography in patients with primary lung cancer. Eur Radiol 24:3242–3250
Huang T-C, Chou K-T, Wang Y-C, Zhang G (2014) Motion freeze for respiration motion correction in PET/CT: A preliminary investigation with lung cancer patient data. Biomed Res Int 2014:167491
van Elmpt W, Hamill J, Jones J, De Ruysscher D, Lambin P, Ollers M (2011) Optimal gating compared to 3D and 4D PET reconstruction for characterization of lung tumours. Eur J Nucl Med Mol Imaging 38:843–855
Chang G, Chang T, Pan T, Clark JW Jr, Mawlawi OR (2010) Implementation of an automated respiratory amplitude gating technique for PET/CT: Clinical evaluation. J Nucl Med 51:16–24
Nehmeh SA, Erdi YE, Ling CC et al (2002) Effect of respiratory gating on quantifying PET images of lung cancer. J Nucl Med 43:876–881
Suzawa N, Ichikawa Y, Ishida M, Tomita Y, Nakayama R, Sakuma H (2016) Respiratory-gated time-of-flight PET/CT during whole-body scan for lung lesions: Feasibility in a routine clinical setting and quantitative analysis. Ann Nucl Med 30:722–730
Chen HH, Chiu NT, Su WC, Guo HR, Lee BF (2012) Prognostic value of whole-body total lesion glycolysis at pretreatment FDG PET/CT in non-small cell lung cancer. Radiology 264:559–566
Huang YE, Lu HI, Liu FY et al (2012) Solitary pulmonary nodules differentiated by dynamic F-18 FDG PET in a region with high prevalence of granulomatous disease. J Radiat Res 53:306–312
Lee P, Bazan JG, Lavori PW et al (2012) Metabolic tumor volume is an independent prognostic factor in patients treated definitively for non-small-cell lung cancer. Clin Lung Cancer 13:52–58
Lee P, Weerasuriya DK, Lavori PW et al (2007) Metabolic tumor burden predicts for disease progression and death in lung cancer. Int J Radiat Oncol Biol Phys 69:328–333
Liu J, Dong M, Sun X, Li W, Xing L, Yu J (2016) Prognostic value of 18F-FDG PET/CT in surgical non-small cell lung cancer: A meta-analysis. PLoS One 11:e0146195
Kim DH, Son SH, Kim CY et al (2014) Prediction for recurrence using F-18 FDG PET/CT in pathologic N0 lung adenocarcinoma after curative surgery. Ann Surg Oncol 21:589–596
Lin Y, Lin WY, Kao CH, Yen KY, Chen SW, Yeh JJ (2012) Prognostic value of preoperative metabolic tumor volumes on PET-CT in predicting disease-free survival of patients with stage I non-small cell lung cancer. Anticancer Res 32:5087–5091
Melloni G, Gajate AM, Sestini S et al (2013) New positron emission tomography derived parameters as predictive factors for recurrence in resected stage I non-small cell lung cancer. Eur J Surg Oncol 39:1254–1261
Zhang H, Wroblewski K, Liao S et al (2013) Prognostic value of metabolic tumor burden from (18)F-FDG PET in surgical patients with non-small-cell lung cancer. Acad Radiol 20:32–40
Gerbaudo VH, Julius B (2007) Anatomo-metabolic characteristics of atelectasis in F-18 FDG-PET/CT imaging. Eur J Radiol 64:401–405
Hovinga M, Sprengers R, Kauczor H-U, Schaefer-Prokop C (2016) CT imaging of interstitial lung diseases. Multidetector-row CT of the thorax. https://doi.org/10.1007/978-3-319-30355-0_7:105-130
Bondue B, Castiaux A, Van Simaeys G et al (2019) Absence of early metabolic response assessed by 18F-FDG PET/CT after initiation of antifibrotic drugs in IPF patients. Respir Res 20:10
Fraioli F, Lyasheva M, Porter JC et al (2019) Synergistic application of pulmonary (18)F-FDG PET/HRCT and computer-based CT analysis with conventional severity measures to refine current risk stratification in idiopathic pulmonary fibrosis (IPF). Eur J Nucl Med Mol Imaging 46:2023–2031
Jacquelin V, Mekinian A, Brillet PY et al (2016) FDG-PET/CT in the prediction of pulmonary function improvement in nonspecific interstitial pneumonia. A pilot study. Eur J Radiol 85:2200–2205
Justet A, Laurent-Bellue A, Thabut G et al (2017) [(18)F]FDG PET/CT predicts progression-free survival in patients with idiopathic pulmonary fibrosis. Respir Res 18:74
Win T, Screaton NJ, Porter JC et al (2018) Pulmonary (18)F-FDG uptake helps refine current risk stratification in idiopathic pulmonary fibrosis (IPF). Eur J Nucl Med Mol Imaging 45:806–815
Mueller-Mang C, Grosse C, Schmid K, Stiebellehner L, Bankier AA (2007) What every radiologist should know about idiopathic interstitial pneumonias. Radiographics 27:595–615
Hansell DM, Kerr IH (1991) The role of high resolution computed tomography in the diagnosis of interstitial lung disease. Thorax 46:77–84
Funding
This work has not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Suk Hyun Lee.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
The requirement for written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observation study
• Performed at a single institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 4600 kb)
Rights and permissions
About this article
Cite this article
Lee, H.J., Son, H.J., Yun, M. et al. Prone position [18F]FDG PET/CT to reduce respiratory motion artefacts in the evaluation of lung nodules. Eur Radiol 31, 4606–4614 (2021). https://doi.org/10.1007/s00330-021-07894-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07894-x