Abstract
Objectives
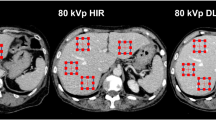
We evaluated lower dose (LD) hepatic dynamic ultra-high-resolution computed tomography (U-HRCT) images reconstructed with deep learning reconstruction (DLR), hybrid iterative reconstruction (hybrid-IR), or model-based IR (MBIR) in comparison with standard-dose (SD) U-HRCT images reconstructed with hybrid-IR as the reference standard to identify the method that allowed for the greatest radiation dose reduction while preserving the diagnostic value.
Methods
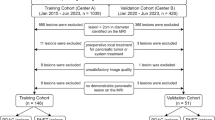
Evaluated were 72 patients who had undergone hepatic dynamic U-HRCT; 36 were scanned with the standard radiation dose (SD group) and 36 with 70% of the SD (lower dose [LD] group). Hepatic arterial and equilibrium phase (HAP, EP) images were reconstructed with hybrid-IR in the SD group, and with hybrid-IR, MBIR, and DLR in the LD group. One radiologist recorded the standard deviation of attenuation in the paraspinal muscle as the image noise. The overall image quality was assessed by 3 other radiologists; they used a 5-point confidence scale ranging from 1 (unacceptable) to 5 (excellent). Superiority and equivalence with prespecified margins were assessed.
Results
With respect to the image noise, in the HAP and EP, LD DLR and LD MBIR images were superior to SD hybrid-IR images; LD hybrid-IR images were neither superior nor equivalent to SD hybrid-IR images. With respect to the quality scores, only LD DLR images were superior to SD hybrid-IR images.
Conclusions
DLR preserved the quality of abdominal U-HRCT images even when scanned with a reduced radiation dose.
Key Points
• Lower dose DLR images were superior to the standard-dose hybrid-IR images quantitatively and qualitatively at abdominal U-HRCT.
• Neither hybrid-IR nor MBIR may allow for a radiation dose reduction at abdominal U-HRCT without compromising the image quality.
• Because DLR allows for a reduction in the radiation dose and maintains the image quality even at the thinnest slice section, DLR should be applied to abdominal U-HRCT scans.






Similar content being viewed by others
Abbreviations
- AiCE:
-
Advanced Intelligent Clear-IQ Engine
- AIDR3D:
-
Adaptive Iterative Dose Reduction 3-Dimensional
- BMI:
-
Body mass index
- CA:
-
Chromosomal aberrations
- CI:
-
Confidence interval
- CNR:
-
Contrast-to-noise ratio
- CTDIvol :
-
CT dose index
- DICOM:
-
Digital Imaging and Communications in Medicine
- DLP:
-
Dose-length product
- DLR:
-
Deep learning reconstruction
- EP:
-
Equilibrium phase
- FIRST:
-
Forward projected model based iterative reconstruction solution
- HAP:
-
Hepatic arterial phase
- Hybrid-IR:
-
Hybrid iterative reconstruction
- LD:
-
Lower dose
- MBIR:
-
Model-based iterative reconstruction
- ROI:
-
Region of interest
- SD:
-
Standard dose
- SSDE:
-
Size-specific dose estimate
- U-HRCT:
-
Ultra-high-resolution computed tomography
References
Kakinuma R, Moriyama N, Muramatsu Y et al (2015) Ultra-high-resolution computed tomography of the lung: image quality of a prototype scanner. PLoS One 10:e0137165
Motoyama S, Ito H, Sarai M et al (2018) Ultra-high-resolution computed tomography angiography for assessment of coronary artery stenosis. Circ J. https://doi.org/10.1253/circj.CJ-17-1281
Tanaka R, Yoshioka K, Takagi H, Schuijf JD, Arakita K (2018) Novel developments in non-invasive imaging of peripheral arterial disease with CT: experience with state-of-the-art, ultra-high-resolution CT and subtraction imaging. Clin Radiol. https://doi.org/10.1016/j.crad.2018.03.002
Yanagawa M, Hata A, Honda O et al (2018) Subjective and objective comparisons of image quality between ultra-high-resolution CT and conventional area detector CT in phantoms and cadaveric human lungs. Eur Radiol 28:5060–5068
Narita K, Nakamura Y, Higaki T, Akagi M, Honda Y, Awai K (2020) Deep learning reconstruction of drip-infusion cholangiography acquired with ultra-high-resolution computed tomography. Abdom Radiol (NY). https://doi.org/10.1007/s00261-020-02508-4
Nakayama Y, Awai K, Funama Y et al (2005) Abdominal CT with low tube voltage: preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology 237:945–951
Volders D, Bols A, Haspeslagh M, Coenegrachts K (2013) Model-based iterative reconstruction and adaptive statistical iterative reconstruction techniques in abdominal CT: comparison of image quality in the detection of colorectal liver metastases. Radiology 269:469–474
Chang W, Lee JM, Lee K et al (2013) Assessment of a model-based, iterative reconstruction algorithm (MBIR) regarding image quality and dose reduction in liver computed tomography. Invest Radiol 48:598–606
Fontarensky M, Alfidja A, Perignon R et al (2015) Reduced radiation dose with model-based iterative reconstruction versus standard dose with adaptive statistical iterative reconstruction in abdominal CT for diagnosis of acute renal colic. Radiology 276:156–166
Euler A, Stieltjes B, Szucs-Farkas Z et al (2017) Impact of model-based iterative reconstruction on low-contrast lesion detection and image quality in abdominal CT: a 12-reader-based comparative phantom study with filtered back projection at different tube voltages. Eur Radiol 27:5252–5259
Mileto A, Guimaraes LS, McCollough CH, Fletcher JG, Yu L (2019) State of the art in abdominal CT: the limits of iterative reconstruction algorithms. Radiology. https://doi.org/10.1148/radiol.2019191422:191422
Laurent G, Villani N, Hossu G et al (2019) Full model-based iterative reconstruction (MBIR) in abdominal CT increases objective image quality, but decreases subjective acceptance. Eur Radiol 29:4016–4025
Yasaka K, Furuta T, Kubo T et al (2017) Full and hybrid iterative reconstruction to reduce artifacts in abdominal CT for patients scanned without arm elevation. Acta Radiol 58:1085–1093
Nakamoto A, Kim T, Hori M et al (2015) Clinical evaluation of image quality and radiation dose reduction in upper abdominal computed tomography using model-based iterative reconstruction; comparison with filtered back projection and adaptive statistical iterative reconstruction. Eur J Radiol 84:1715–1723
Deak Z, Grimm JM, Treitl M et al (2013) Filtered back projection, adaptive statistical iterative reconstruction, and a model-based iterative reconstruction in abdominal CT: an experimental clinical study. Radiology 266:197–206
Akagi M, Nakamura Y, Higaki T et al (2019) Deep learning reconstruction improves image quality of abdominal ultra-high-resolution CT. Eur Radiol 29:6163–6171
Tatsugami F, Higaki T, Nakamura Y et al (2019) Deep learning-based image restoration algorithm for coronary CT angiography. Eur Radiol 29:5322–5329
Nakamura Y, Higaki T, Tatsugami F et al (2019) Deep learning-based CT image reconstruction: initial evaluation targeting hypovascular hepatic metastases. Radiol Artif Intell 1:e180011
Nakamura Y, Higaki T, Tatsugami F et al (2020) Possibility of deep learning in medical imaging focusing improvement of computed tomography image quality. J Comput Assist Tomogr 44:161–167
Higaki T, Nakamura Y, Zhou J et al (2020) Deep learning reconstruction at CT: phantom study of the image characteristics. Acad Radiol 27:82–87
Singh R, Digumarthy SR, Muse VV et al (2020) Image quality and lesion detection on deep learning reconstruction and iterative reconstruction of submillisievert chest and abdominal CT. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.19.21809:1-8
Higaki T, Nishimaru E, Nakamura Y et al (2018) Radiation dose reduction in CT using deep learning based reconstruction (DLR): a phantom study. ECR2018. https://doi.org/10.1594/ecr2018/C-1656, https://posterng.netkey.at/esr/viewing/index.php?module=viewing_poster&task=&pi=143052
Brady SL, Kaufman RA (2012) Investigation of American Association of Physicists in Medicine Report 204 size-specific dose estimates for pediatric CT implementation. Radiology 265:832–840
Christner JA, Braun NN, Jacobsen MC, Carter RE, Kofler JM, McCollough CH (2012) Size-specific dose estimates for adult patients at CT of the torso. Radiology 265:841–847
American Association of Physicists in Medicine (2011) Size-specific dose estimates (SSDE) in Pediatric and adult body CT examinations (Task Group 204). American Association of Physicists in Medicine, College Park, MD https://www.aapm.org/pubs/reports/RPT_204.pdf
Phelps AS, Naeger DM, Courtier JL et al (2015) Pairwise comparison versus Likert scale for biomedical image assessment. AJR Am J Roentgenol 204:8–14
Likert R (1932) A technique for the measurement of attitudes. Arch Psychol 140:55
Hur BY, Lee JM, Joo I et al (2014) Liver computed tomography with low tube voltage and model-based iterative reconstruction algorithm for hepatic vessel evaluation in living liver donor candidates. J Comput Assist Tomogr 38:367–375
Svanholm H, Starklint H, Gundersen HJ, Fabricius J, Barlebo H, Olsen S (1989) Reproducibility of histomorphologic diagnoses with special reference to the kappa statistic. APMIS 97:689–698
Japan Association on Radiological Protection in Medicine (2015) Diagnostic reference levels based on latest surveys in Japan: Japan DRLs 2015. http://www.radher.jp/J-RIME/report/DRLhoukokusyoEng.pdf
Yoshioka K, Tanaka R, Takagi H et al (2018) Ultra-high-resolution CT angiography of the artery of Adamkiewicz: a feasibility study. Neuroradiology 60:109–115
Tamm EP, Rong XJ, Cody DD, Ernst RD, Fitzgerald NE, Kundra V (2011) Quality initiatives: CT radiation dose reduction: how to implement change without sacrificing diagnostic quality. Radiographics 31:1823–1832
Bonassi S, Norppa H, Ceppi M et al (2008) Chromosomal aberration frequency in lymphocytes predicts the risk of cancer: results from a pooled cohort study of 22 358 subjects in 11 countries. Carcinogenesis 29:1178–1183
Fucic A, Bonassi S, Gundy S et al (2016) Frequency of acentric fragments are associated with cancer risk in subjects exposed to ionizing radiation. Anticancer Res 36:2451–2457
Abe Y, Noji H, Miura T et al (2019) Investigation of the cumulative number of chromosome aberrations induced by three consecutive CT examinations in eight patients. J Radiat Res 60:729–739
Sakane H, Ishida M, Shi L et al (2020) Biological effects of low-dose chest CT on chromosomal DNA. Radiology 295:439–445
Valentin J (2005) Low-dose extrapolation of radiation-related cancer risk. Ann ICRP 35:1–140
Marrero JA, Kulik LM, Sirlin CB et al (2018) Diagnosis, staging, and management of hepatocellular carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 68:723–750
Heimbach JK, Kulik LM, Finn RS et al (2018) AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67:358–380
Qurashi AA, Rainford LA, Alshamrani KM, Foley SJ (2018) The impact of obesity on abdominal CT radiation dose and image quality. Radiat Prot Dosimetry. https://doi.org/10.1093/rpd/ncy212
Funding
Dr. Kazuo Awai received a research funding from Canon Medical Systems Co. Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Kazuo Awai.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Canon Medical Systems Co. Ltd for Kazuo Awai.
The other authors declare that they have no conflict of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Our institutional review board approved our study in which we applied 70% of the standard radiation dose plus deep learning reconstruction (DLR) to obtain hepatic dynamic CT scans as an observational study. Hybrid iterative reconstruction (hybrid-IR) and model-based IR (MBIR) images were reconstructed from the existing raw data. Thus, prior informed patient consent was waived.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 42 kb)
Rights and permissions
About this article
Cite this article
Nakamura, Y., Narita, K., Higaki, T. et al. Diagnostic value of deep learning reconstruction for radiation dose reduction at abdominal ultra-high-resolution CT. Eur Radiol 31, 4700–4709 (2021). https://doi.org/10.1007/s00330-020-07566-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07566-2