Abstract
Objectives
The proton density–weighted, in-phase stack-of-stars (PDIP-SOS) MRI technique provides calcification visualization in peripheral artery disease (PAD). This study sought to investigate the diagnostic accuracy of a combined non-contrast quiescent-interval slice-selective (QISS) MRA and PDIP-SOS MRI protocol for the detection of PAD, in comparison with CTA and digital subtraction angiography (DSA).
Methods
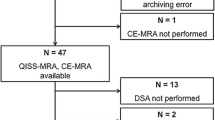
Twenty-six prospectively enrolled PAD patients (70 ± 8 years) underwent lower extremity CTA and 1.5-T or 3-T PDIP-SOS/QISS MRI prior to DSA. Two readers rated image quality and graded stenosis (≥ 50%) on QISS MRA without/with calcification visualization. Sensitivity, specificity, and area under the curve (AUC) were calculated against DSA. Calcification was quantified and compared between MRI and non-contrast CT (NCCT) using paired t test, Pearson’s correlation, and Bland-Altman analysis.
Results
Image quality ratings were significantly higher for CTA compared to those for MRA (4.0 [3.0–4.0] and 3.0 [3.0–4.0]; p = 0.0369). The sensitivity and specificity of QISS MRA, QISS MRA with PDIP-SOS, and CTA for ≥ 50% stenosis detection were 85.4%, 92.2%, and 90.2%, and 90.3%, 93.2%, and 94.2%, respectively, while AUCs were 0.879, 0.928, and 0.923, respectively. A significant increase in AUC was observed when PDIP-SOS was added to the MRA protocol (p = 0.0266). Quantification of calcification showed significant differences between PDIP-SOS and NCCT (80.6 ± 31.2 mm3 vs. 88.0 ± 29.8 mm3; p = 0.0002) with high correlation (r = 0.77, p < 0.0001) and moderate mean of differences (− 7.4 mm3).
Conclusion
QISS MRA combined with PDIP-SOS MRI provides improved, CTA equivalent, accuracy for the detection of PAD, although its image quality remains inferior to CTA.
Key Points
• Agreement in stenosis detection rate using non-contrast quiescent-interval slice-selective MRA compared to DSA improved when calcification visualization was provided to the readers.
• An increase was observed in both sensitivity and specificity for the detection of ≥ 50% stenosis when MRI-based calcification assessment was added to the protocol, resulting in a diagnostic accuracy more comparable to CTA.
• Quantification of calcification showed statistical difference between MRI and non-contrast CT; however, a high correlation was observed between the techniques.



Similar content being viewed by others
Abbreviations
- ABI:
-
Ankle brachial index
- CI:
-
Confidence interval
- ICC:
-
Intraclass correlation coefficient
- MIP:
-
Maximum intensity projection
- NCCT:
-
Non-contrast computed tomography
- PAD:
-
Peripheral artery disease
- PDIP-SOS:
-
Proton density–weighted, in-phase stack-of-stars
- PETRA:
-
Point-wise encoding time reduction with radial acquisition
- QISS:
-
Quiescent-interval slice-selective
- UTE:
-
Ultra-short echo time
- VNC:
-
Virtual non-contrast
References
Criqui MH, Aboyans V (2015) Epidemiology of peripheral artery disease. Circ Res 116:1509–1526
Hiatt WR, Hoag S, Hamman RF (1995) Effect of diagnostic criteria on the prevalence of peripheral arterial disease. The San Luis Valley Diabetes Study. Circulation 91:1472–1479
Pollak AW, Norton PT, Kramer CM (2012) Multimodality imaging of lower extremity peripheral arterial disease: current role and future directions. Circ Cardiovasc Imaging 5:797–807
Ouwendijk R, Kock MC, van Dijk LC, van Sambeek MR, Stijnen T, Hunink MG (2006) Vessel wall calcifications at multi-detector row CT angiography in patients with peripheral arterial disease: effect on clinical utility and clinical predictors. Radiology 241:603–608
Davenport MS, Khalatbari S, Cohan RH, Dillman JR, Myles JD, Ellis JH (2013) Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material: risk stratification by using estimated glomerular filtration rate. Radiology 268:719–728
Mathur M, Jones JR, Weinreb JC (2020) Gadolinium deposition and nephrogenic systemic fibrosis: a radiologist’s primer. Radiographics 40:153–162
American College of Rardiology Committee on Drugs and Contrast Media. ACR manual on contrast media. Available at: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf. Accessed 3 June 2020
Tranche-Iparraguirre S, Marin-Iranzo R, Fernandez-de Sanmamed R, Riesgo-Garcia A, Hevia-Rodriguez E, Garcia-Casas JB (2012) Peripheral arterial disease and kidney failure: a frequent association. Nefrologia 32:313–320
Edelman RR, Sheehan JJ, Dunkle E, Schindler N, Carr J, Koktzoglou I (2010) Quiescent-interval single-shot unenhanced magnetic resonance angiography of peripheral vascular disease: technical considerations and clinical feasibility. Magn Reson Med 63:951–958
Varga-Szemes A, Wichmann JL, Schoepf UJ et al (2017) Accuracy of noncontrast quiescent-interval single-shot lower extremity MR angiography versus CT angiography for diagnosis of peripheral artery disease: comparison with digital subtraction angiography. JACC Cardiovasc Imaging 10:1116–1124
Hodnett PA, Ward EV, Davarpanah AH et al (2011) Peripheral arterial disease in a symptomatic diabetic population: prospective comparison of rapid unenhanced MR angiography (MRA) with contrast-enhanced MRA. AJR Am J Roentgenol 197:1466–1473
Amin P, Collins JD, Koktzoglou I et al (2014) Evaluating peripheral arterial disease with unenhanced quiescent-interval single-shot MR angiography at 3 T. AJR Am J Roentgenol 202:886–893
Altaha MA, Jaskolka JD, Tan K et al (2017) Non-contrast-enhanced MR angiography in critical limb ischemia: performance of quiescent-interval single-shot (QISS) and TSE-based subtraction techniques. Eur Radiol 27:1218–1226
Ferreira Botelho MP, Koktzoglou I, Collins JD et al (2017) MR imaging of iliofemoral peripheral vascular calcifications using proton density-weighted, in-phase three-dimensional stack-of-stars gradient echo. Magn Reson Med 77:2146–2152
Serhal A, Koktzoglou I, Aouad P et al (2018) Cardiovascular magnetic resonance imaging of aorto-iliac and ilio-femoral vascular calcifications using proton density-weighted in-phase stack of stars. J Cardiovasc Magn Reson 20:51
Fleischmann D, Kamaya A (2009) Optimal vascular and parenchymal contrast enhancement: the current state of the art. Radiol Clin North Am 47:13–26
Fraioli F, Catalano C, Napoli A et al (2006) Low-dose multidetector-row CT angiography of the infra-renal aorta and lower extremity vessels: image quality and diagnostic accuracy in comparison with standard DSA. Eur Radiol 16:137–146
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH image to ImageJ: 25 years of image analysis. Nat Methods 9:671–675
Bischoff B, Kantert C, Meyer T et al (2012) Cardiovascular risk assessment based on the quantification of coronary calcium in contrast-enhanced coronary computed tomography angiography. Eur Heart J Cardiovasc Imaging 13:468–475
Wagner M, Knobloch G, Gielen M et al (2015) Nonenhanced peripheral MR-angiography (MRA) at 3 tesla: evaluation of quiescent-interval single-shot MRA in patients undergoing digital subtraction angiography. Int J Cardiovasc Imaging 31:841–850
Hodnett PA, Koktzoglou I, Davarpanah AH et al (2011) Evaluation of peripheral arterial disease with nonenhanced quiescent-interval single-shot MR angiography. Radiology 260:282–293
Klasen J, Blondin D, Schmitt P et al (2012) Nonenhanced ECG-gated quiescent-interval single-shot MRA (QISS-MRA) of the lower extremities: comparison with contrast-enhanced MRA. Clin Radiol 67:441–446
Ward EV, Galizia MS, Usman A, Popescu AR, Dunkle E, Edelman RR (2013) Comparison of quiescent inflow single-shot and native space for nonenhanced peripheral MR angiography. J Magn Reson Imaging 38:1531–1538
Sharma S, Boujraf S, Bornstedt A et al (2010) Quantification of calcifications in endarterectomy samples by means of high-resolution ultra-short echo time imaging. Invest Radiol 45:109–113
Du J, Corbeil J, Znamirowski R et al (2011) Direct imaging and quantification of carotid plaque calcification. Magn Reson Med 65:1013–1020
Edelman RR, Flanagan O, Grodzki D, Giri S, Gupta N, Koktzoglou I (2015) Projection MR imaging of peripheral arterial calcifications. Magn Reson Med 73:1939–1945
Serhal A, Koktzoglou I, Edelman RR (2019) Feasibility of image fusion for concurrent MRI evaluation of vessel lumen and vascular calcifications in peripheral arterial disease. AJR Am J Roentgenol 212:914–918
Dietrich O, Raya JG, Reeder SB, Reiser MF, Schoenberg SO (2007) Measurement of signal-to-noise ratios in MR images: influence of multichannel coils, parallel imaging, and reconstruction filters. J Magn Reson Imaging 26:375–385
Norgren L, Hiatt WR, Dormandy JA et al (2007) Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 45(Suppl S):S5–S67
Lin JH, Brunson A, Romano PS, Mell MW, Humphries MD (2019) Endovascular-first treatment is associated with improved amputation-free survival in patients with critical limb ischemia. Circ Cardiovasc Qual Outcomes 12:e005273
Funding
This study was supported by a research grant from Siemens and by NIH NHLBI R01 HL130093 (RRE).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is U. Joseph Schoepf.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: U. Joseph Schoepf is a consultant for and/or receives research support from Astellas, Bayer, Elucid Bioimaging, Guerbet, HeartFlow Inc., and Siemens Healthcare. Akos Varga-Szemes receives institutional research and travel support from Siemens Healthcare and is a consultant for Elucid Bioimaging. Robert R. Edelman receives grant support and royalties from Siemens Healthcare. Ioannis Koktzoglou receives research support from Siemens Healthcare.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Varga-Szemes, A., Penmetsa, M., Emrich, T. et al. Diagnostic accuracy of non-contrast quiescent-interval slice-selective (QISS) MRA combined with MRI-based vascular calcification visualization for the assessment of arterial stenosis in patients with lower extremity peripheral artery disease. Eur Radiol 31, 2778–2787 (2021). https://doi.org/10.1007/s00330-020-07386-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07386-4