Abstract
Objective
To review the diagnostic performance of CT and MRI for detecting extranodal extension (ENE) in head and neck squamous cell carcinoma (HNSCC) patients.
Methods
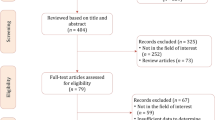
MEDLINE and EMBASE databases were searched up to October 7, 2019. Studies that evaluated the diagnostic performance of CT and/or MRI for detecting ENE in HNSCC patients were included. A 2 × 2 table was reconstructed for each study. Pooled sensitivity and specificity were calculated using the bivariate model and hierarchical summary receiver operating characteristic (HSROC) model. Subgroup analyses were performed according to HPV status and radiological features. Pooled correlation coefficient for interobserver agreement was calculated.
Results
Twenty-two studies including 2478 patients were included. The pooled sensitivity and specificity for detecting ENE were 73% (95% CI, 62–82%) and 83% (95% CI, 75–89%), respectively, for CT, and 60% (95% CI, 49–70%) and 96% (95% CI, 85–99%), respectively, for MRI. There was substantial heterogeneity for both CT and MRI. A threshold effect was present for MRI. On subgroup analysis, the pooled specificity of CT was significantly lower in patients with HPV+ OPSCC than in patients with HPV‑ oral cavity cancer or all HNSCC (74% vs. 87%; p = 0.01). Central node necrosis showed significantly higher pooled sensitivity (81% vs. 51%; p = 0.02), while infiltration of adjacent planes showed significantly higher pooled specificity (94% vs. 65%; p = 0.03). The pooled correlation coefficient was 0.72 (95% CI, 0.60–0.81).
Conclusion
Both CT and MRI show reasonable diagnostic performance for detecting ENE in HNSCC patients and interobserver agreement was substantial.
Key Points
• Pooled sensitivity and specificity were 73% and 83% for CT and 60% and 96% for MRI without significant difference.
• Pooled specificity was lower for HPV+ OPSCC than for HPV‑ oral cavity cancer or all HNSCC (74% vs. 87%, p = 0.01), likely due to central node necrosis.
• Central node necrosis showed higher sensitivity (81% vs. 51%; p = 0.02), while infiltration of adjacent planes showed higher specificity (94% vs. 65%; p = 0.03).






Similar content being viewed by others
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- ENE:
-
Extranodal extension
- HNSCC:
-
Head and neck squamous cell carcinoma
- HPV:
-
Human papillomavirus
- HSROC:
-
Hierarchical summary receiver operating characteristic
- OPSCC:
-
Oropharyngeal squamous cell carcinoma
- PRISMA-DTA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analysis of Diagnostic Test Accuracy Studies
- QUADAS-2:
-
Quality Assessment of Diagnostic Accuracy Studies-2
- RT:
-
Radiotherapy
- TLM:
-
Transoral laser microsurgery
- TORS:
-
Transoral robotic surgery
References
Almulla A, Noel CW, Lu L et al (2018) Radiologic-pathologic correlation of extranodal extension in patients with squamous cell carcinoma of the oral cavity: implications for future editions of the TNM classification. Int J Radiat Oncol Biol Phys 102:698–708
Bernier J, Cooper JS, Pajak T et al (2005) Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (# 22931) and RTOG (# 9501). Head Neck 27:843–850
Cooper JS, Zhang Q, Pajak TF et al (2012) Long-term follow-up of the RTOG 9501/intergroup phase III trial: postoperative concurrent radiation therapy and chemotherapy in high-risk squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 84:1198–1205
Amin MB, Edge S, Greene F et al (2017) AJCC cancer staging manual. Springer
An Y, Park HS, Kelly JR et al (2017) The prognostic value of extranodal extension in human papillomavirus-associated oropharyngeal squamous cell carcinoma. Cancer 123:2762–2772
Haughey BH, Sinha P, Kallogjeri D et al (2016) Pathology-based staging for HPV-positive squamous carcinoma of the oropharynx. Oral Oncol 62:11–19
Huang SH, Xu W, Waldron J et al (2015) Refining American Joint Committee on Cancer/Union for International Cancer Control TNM stage and prognostic groups for human papillomavirus-related oropharyngeal carcinomas. J Clin Oncol 33:836–845
O'Sullivan B, Huang SH, Su J et al (2016) Development and validation of a staging system for HPV-related oropharyngeal cancer by the International Collaboration on Oropharyngeal cancer Network for Staging (ICON-S): a multicentre cohort study. Lancet Oncol 17:440–451
Zhan KY, Eskander A, Kang SY et al (2017) Appraisal of the AJCC 8th edition pathologic staging modifications for HPV-positive oropharyngeal cancer, a study of the National Cancer Data Base. Oral Oncol 73:152–159
Genden EM, Desai S, Sung CK (2009) Transoral robotic surgery for the management of head and neck cancer: a preliminary experience. Head Neck 31:283–289
Moore EJ, Olsen KD, Kasperbauer JL (2009) Transoral robotic surgery for oropharyngeal squamous cell carcinoma: a prospective study of feasibility and functional outcomes. Laryngoscope 119:2156–2164
O'Malley BW Jr, Weinstein GS, Snyder W, Hockstein NG (2006) Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope 116:1465–1472
Quon H, O’Malley BW Jr, Weinstein GS (2011) Postoperative adjuvant therapy after transoral robotic resection for oropharyngeal carcinomas: rationale and current treatment approach. ORL J Otorhinolaryngol Relat Spec 73:121–130
Weinstein GS, O’Malley BW, Snyder W, Sherman E, Quon H (2007) Transoral robotic surgery: radical tonsillectomy. Arch Otolaryngol Head Neck Surg 133:1220–1226
Weinstein GS, Quon H, Newman HJ et al (2012) Transoral robotic surgery alone for oropharyngeal cancer: an analysis of local control. Arch Otolaryngol Head Neck Surg 138:628–634
Weinstein GS, Quon H, O'Malley BW Jr, Kim GG, Cohen MA (2010) Selective neck dissection and deintensified postoperative radiation and chemotherapy for oropharyngeal cancer: a subset analysis of the University of Pennsylvania transoral robotic surgery trial. Laryngoscope 120:1749–1755
Chai RL, Rath TJ, Johnson JT et al (2013) Accuracy of computed tomography in the prediction of extracapsular spread of lymph node metastases in squamous cell carcinoma of the head and neck. JAMA Otolaryngol Head Neck Surg 139:1187–1194
Referenced with permission from the NCCN Guidelines® for Head and Neck Cancers V.3.2019 © National Comprehensive Cancer Network, Inc. 2019. All rights reserved. Accessed 12/31/2019. Available online at www.NCCN.org
Mermod M, Tolstonog G, Simon C, Monnier Y (2016) Extracapsular spread in head and neck squamous cell carcinoma: a systematic review and meta-analysis. Oral Oncol 62:60–71
Su Z, Duan Z, Pan W et al (2016) Predicting extracapsular spread of head and neck cancers using different imaging techniques: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 45:413–421
McInnes MDF, Moher D, Thombs BD et al (2018) Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319:388–396
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 3:25
Kim KW, Lee J, Choi SH, Huh J, Park SH (2015) Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical researchers-part I. general guidance and tips. Korean J Radiol 16:1175–1187
Lee J, Kim KW, Choi SH, Huh J, Park SH (2015) Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical researchers-part II. Statistical methods of meta-analysis. Korean J Radiol 16:1188–1196
Suh CH, Park SH (2016) Successful publication of systematic review and meta-analysis of studies evaluating diagnostic test accuracy. Korean J Radiol 17:5–6
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
Hedges LV, Olkin I (2014) Statistical methods for meta-analysis. Academic press
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Deville WL, Buntinx F, Bouter LM et al (2002) Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol 2:9
Curtin HD, Som PM (2011) Head and neck imaging. Mosby
Sharma A, Jaiswal AA, Umredkar G et al (2017) Lymph node central necrosis on the computed tomography as the predictor of the extra capsular spread in metastatic head and neck squamous cell carcinoma. Indian J Otolaryngol Head Neck Surg 69:323–332
Carlton JA, Maxwell AW, Bauer LB et al (2017) Computed tomography detection of extracapsular spread of squamous cell carcinoma of the head and neck in metastatic cervical lymph nodes. Neuroradiol J 30:222–229
Faraji F, Aygun N, Coquia SF et al (2019) Computed tomography performance in predicting extranodal extension in HPV-positive oropharynx cancer. Laryngoscope. https://doi.org/10.1002/lary.28237
Frood R, Palkhi E, Barnfield M, Prestwich R, Vaidyanathan S, Scarsbrook A (2018) Can MR textural analysis improve the prediction of extracapsular nodal spread in patients with oral cavity cancer? Eur Radiol 28:5010–5018
Geltzeiler M, Clayburgh D, Gleysteen J et al (2017) Predictors of extracapsular extension in HPV-associated oropharyngeal cancer treated surgically. Oral Oncol 65:89–93
Hao SP, Ng SH (2000) Magnetic resonance imaging versus clinical palpation in evaluating cervical metastasis from head and neck cancer. Otolaryngol Head Neck Surg 123:324–327
Kann BH, Aneja S, Loganadane GV et al (2018) Pretreatment identification of head and neck cancer nodal metastasis and extranodal extension using deep learning neural networks. Sci Rep 8:14036
Kimura Y, Sumi M, Sakihama N, Tanaka F, Takahashi H, Nakamura T (2008) MR imaging criteria for the prediction of extranodal spread of metastatic cancer in the neck. AJNR Am J Neuroradiol 29:1355–1359
King AD, Tse GM, Yuen EH et al (2004) Comparison of CT and MR imaging for the detection of extranodal neoplastic spread in metastatic neck nodes. Eur J Radiol 52:264–270
Lee B, Choi YJ, Kim SO et al (2019) Prognostic value of radiologic extranodal extension in human papillomavirus-related oropharyngeal squamous cell carcinoma. Korean J Radiol 20:1266–1274
Lodder WL, Lange CA, van Velthuysen ML et al (2013) Can extranodal spread in head and neck cancer be detected on MR imaging. Oral Oncol 49:626–633
Moreno KF, Cornelius RS, Lucas FV, Meinzen-Derr J, Patil YJ (2017) Using 3 Tesla magnetic resonance imaging in the pre-operative evaluation of tongue carcinoma. J Laryngol Otol 131:793–800
Noor A, Mintz J, Patel S et al (2019) Predictive value of computed tomography in identifying extracapsular spread of cervical lymph node metastases in p16 positive oropharyngeal squamous cell carcinoma. J Med Imaging Radiat Oncol 63:500–509
Patel MR, Hudgins PA, Beitler JJ et al (2018) Radiographic imaging does not reliably predict macroscopic extranodal extension in human papilloma virus-associated oropharyngeal cancer. ORL J Oto-Rhino-Laryngol Relat Spec 80:85–95
Prabhu RS, Magliocca KR, Hanasoge S et al (2014) Accuracy of computed tomography for predicting pathologic nodal extracapsular extension in patients with head-and-neck cancer undergoing initial surgical resection. Int J Radiat Oncol Biol Phys 88:122–129
Randall DR, Lysack JT, Hudon ME et al (2015) Diagnostic utility of central node necrosis in predicting extracapsular spread among oral cavity squamous cell carcinoma. Head Neck 37:92–96
Shaw RJ, Lowe D, Woolgar JA et al (2010) Extracapsular spread in oral squamous cell carcinoma. Head Neck 32:714–722
Souter MA, Allison RS, Clarkson JH, Cowan IA, Coates MH, Wells JE (2009) Sensitivity and specificity of computed tomography for detection of extranodal spread from metastatic head and neck squamous cell carcinoma. J Laryngol Otol 123:778–782
Url C, Schartinger VH, Riechelmann H et al (2013) Radiological detection of extracapsular spread in head and neck squamous cell carcinoma (HNSCC) cervical metastases. Eur J Radiol 82:1783–1787
Zoumalan RA, Kleinberger AJ, Morris LG et al (2010) Lymph node central necrosis on computed tomography as predictor of extracapsular spread in metastatic head and neck squamous cell carcinoma: pilot study. J Laryngol Otol 124:1284–1288
Huang YH, Yeh CH, Cheng NM et al (2017) Cystic nodal metastasis in patients with oropharyngeal squamous cell carcinoma receiving chemoradiotherapy: relationship with human papillomavirus status and failure patterns. PLoS One 12:e0180779
McGrath TA, McInnes MD, Korevaar DA, Bossuyt PM (2016) Meta-analyses of diagnostic accuracy in imaging journals: analysis of pooling techniques and their effect on summary estimates of diagnostic accuracy. Radiology 281:78–85
Sumi M, Nakamura T (2011) Extranodal spread in the neck: MRI detection on the basis of pixel-based time-signal intensity curve analysis. J Magn Reson Imaging 33:830–838
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Young Jun Choi.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because this study was a systematic review and meta-analysis using data from published studies.
Ethical approval
Institutional Review Board approval was not required because this study was a systematic review and meta-analysis using data from published studies.
Methodology
• systematic review
• meta-analysis
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 252 kb)
Rights and permissions
About this article
Cite this article
Park, S.I., Guenette, J.P., Suh, C.H. et al. The diagnostic performance of CT and MRI for detecting extranodal extension in patients with head and neck squamous cell carcinoma: a systematic review and diagnostic meta-analysis. Eur Radiol 31, 2048–2061 (2021). https://doi.org/10.1007/s00330-020-07281-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07281-y