Abstract
Objectives
To determine the accuracies of the American College of Radiology (ACR)–thyroid imaging reporting and data systems (TIRADS), Korean (K)-TIRADS, and European (EU)-TIRADS for diagnosing malignancy in thyroid nodules.
Methods
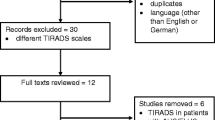
Original studies reporting the diagnostic accuracy of TIRADS for determining malignancy on ultrasound were identified in MEDLINE and EMBASE up to June 23, 2019. The meta-analytic summary sensitivity and specificity were obtained for TIRADS category 5 (TR-5) and category 4 or 5 (TR-4/5), using a bivariate random effects model. To explore study heterogeneity, meta-regression analyses were performed.
Results
Of the 34 eligible articles (37,585 nodules), 25 used ACR-TIRADS, 12 used K-TIRADS, and seven used EU-TIRADS. For TR-5, the meta-analytic sensitivity was highest for EU-TIRADS (78% [95% confidence interval, 64–88%]), followed by ACR-TIRADS (70% [61–79%]) and K-TIRADS (64% [58–70%]), although the differences were not significant. K-TIRADS showed the highest meta-analytic specificity (93% [91–95%]), which was similar to ACR-TIRADS (89% [85–92%]) and EU-TIRADS (89% [77–95%]). For TR-4/5, all three TIRADS systems had sensitivities higher than 90%. K-TIRADS had the highest specificity (61% [50–72%]), followed by ACR-TIRADS (49% [43–56%]) and EU-TIRADS (48% [35–62%]), although the differences were not significant. Considerable threshold effects were noted with ACR- and K-TIRADS (p ≤ 0.01), with subject enrollment, country of origin, experience level of reviewer, number of patients, and clarity of blinding in review being the main causes of heterogeneity (p ≤ 0.05).
Conclusions
There was no significant difference among these three international TIRADS, but the trend toward higher sensitivity with EU-TIRADS and higher specificity with K-TIRADS.
Key Points
• For TIRADS category 5, the meta-analytic sensitivity was highest for the EU-TIRADS, followed by the ACR-TIRADS and the K-TIRADS, although the differences were not significant.
• For TIRADS category 5, K-TIRADS showed the highest meta-analytic specificity, which was similar to ACR-TIRADS and EU-TIRADS.
• Considerable threshold effects were noted with ACR- and K-TIRADS, with subject enrollment, country of origin, experience level of reviewer, number of patients, and clarity of blinding in review being the main causes of heterogeneity.



Similar content being viewed by others
Abbreviations
- ACR:
-
American College of Radiology
- CI:
-
Confidence interval
- ETA:
-
European Thyroid Association
- EU:
-
European
- FNA:
-
Fine-needle aspiration
- HSROC:
-
Hierarchical summary receiver operating characteristic
- K:
-
Korean
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QUADAS:
-
Quality Assessment of Diagnostic Accuracy Studies
- TIRADS:
-
Thyroid imaging reporting and data system
- US:
-
Ultrasound
References
Guth S, Theune U, Aberle J, Galach A, Bamberger CM (2009) Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest 39:699–706
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133
Gharib H, Papini E, Garber JR et al (2016) American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules--2016 update. Endocr Pract 22:622–639
Brito JP, Gionfriddo MR, Al Nofal A et al (2014) The accuracy of thyroid nodule ultrasound to predict thyroid cancer: systematic review and meta-analysis. J Clin Endocrinol Metab 99:1253–1263
Moon WJ, Jung SL, Lee JH et al (2008) Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology 247:762–770
Choi SH, Kim EK, Kwak JY, Kim MJ, Son EJ (2010) Interobserver and intraobserver variations in ultrasound assessment of thyroid nodules. Thyroid 20:167–172
Lee HJ, Yoon DY, Seo YL et al (2018) Intraobserver and interobserver variability in ultrasound measurements of thyroid nodules. J Ultrasound Med 37:173–178
Horvath E, Majlis S, Rossi R et al (2009) An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab 94:1748–1751
Shin JH, Baek JH, Chung J et al (2016) Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol 17:370–395
Tessler FN, Middleton WD, Grant EG et al (2017) ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS committee. J Am Coll Radiol 14:587–595
Russ G, Bonnema SJ, Erdogan MF, Durante C, Ngu R, Leenhardt L (2017) European thyroid association guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: the EU-TIRADS. Eur Thyroid J 6:225–237
Wei X, Li Y, Zhang S, Gao M (2016) Meta-analysis of thyroid imaging reporting and data system in the ultrasonographic diagnosis of 10,437 thyroid nodules. Head Neck 38:309–315
Ha EJ, Moon WJ, Na DG et al (2016) A multicenter prospective validation study for the Korean thyroid imaging reporting and data system in patients with thyroid nodules. Korean J Radiol 17:811–821
Middleton WD, Teefey SA, Reading CC et al (2017) Multiinstitutional analysis of thyroid nodule risk stratification using the American College of Radiology thyroid imaging reporting and data system. AJR Am J Roentgenol 208:1331–1341
Grani G, Lamartina L, Ascoli V et al (2019) Reducing the number of unnecessary thyroid biopsies while improving diagnostic accuracy: toward the “right” TIRADS. J Clin Endocrinol Metab 104:95–102
Jin ZQ, Yu HZ, Mo CJ, Su RQ (2019) Clinical study of the prediction of malignancy in thyroid nodules: modified score versus 2017 American College of Radiology’s thyroid imaging reporting and data system ultrasound lexicon. Ultrasound Med Biol 45:1627–1637
Bae JM, Hahn SY, Shin JH, Ko EY (2018) Inter-exam agreement and diagnostic performance of the Korean thyroid imaging reporting and data system for thyroid nodule assessment: real-time versus static ultrasonography. Eur J Radiol 98:14–19
Koseoglu Atilla FD, Ozgen Saydam B, Erarslan NA et al (2018) Does the ACR TI-RADS scoring allow us to safely avoid unnecessary thyroid biopsy? single center analysis in a large cohort. Endocrine 61:398–402
Wu XL, Du JR, Wang H et al (2019) Comparison and preliminary discussion of the reasons for the differences in diagnostic performance and unnecessary FNA biopsies between the ACR TIRADS and 2015 ATA guidelines. Endocrine 65:121–131
Zhu J, Li X, Wei X et al (2019) The application value of modified thyroid imaging report and data system in diagnosing medullary thyroid carcinoma. Cancer Med 8:3389–3400
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Ha SM, Kim JK, Baek JH (2017) Detection of malignancy among suspicious thyroid nodules <1 cm on ultrasound with various thyroid image reporting and data systems. Thyroid 27:1307–1315
Ha SM, Ahn HS, Baek JH et al (2017) Validation of three scoring risk-stratification models for thyroid nodules. Thyroid 27:1550–1557
Hong MJ, Na DG, Baek JH, Sung JY, Kim JH (2017) Cytology-ultrasonography risk-stratification scoring system based on fine-needle aspiration cytology and the Korean-thyroid imaging reporting and data system. Thyroid 27:953–959
Chung SR, Choi YJ, Suh CH et al (2018) Thyroid incidentalomas detected on (18)F-fluorodeoxyglucose positron emission tomography with computed tomography: malignant risk stratification and management plan. Thyroid 28:762–768
Gao L, Liu R, Jiang Y et al (2018) Computer-aided system for diagnosing thyroid nodules on ultrasound: a comparison with radiologist-based clinical assessments. Head Neck 40:778–783
Ha EJ, Na DG, Moon WJ, Lee YH, Choi N (2018) Diagnostic performance of ultrasound-based risk-stratification systems for thyroid nodules: comparison of the 2015 American Thyroid Association guidelines with the 2016 Korean thyroid association/Korean society of thyroid radiology and 2017 American congress of radiology guidelines. Thyroid 28:1532–1537
Hang J, Li F, Qiao XH, Ye XH, Li A, Du LF (2018) Combination of maximum shear wave elasticity modulus and TIRADS improves the diagnostic specificity in characterizing thyroid nodules: a retrospective study. Int J Endocrinol 2018:4923050
Hoang JK, Middleton WD, Farjat AE et al (2018) Reduction in thyroid nodule biopsies and improved accuracy with American College of Radiology thyroid imaging reporting and data system. Radiology 287:185–193
Hong MJ, Na DG, Baek JH, Sung JY, Kim JH (2018) Impact of nodule size on malignancy risk differs according to the ultrasonography pattern of thyroid nodules. Korean J Radiol 19:534–541
Lauria Pantano A, Maddaloni E, Briganti SI et al (2018) Differences between ATA, AACE/ACE/AME and ACR TI-RADS ultrasound classifications performance in identifying cytological high-risk thyroid nodules. Eur J Endocrinol 178:595–603
Rosario PW, da Silva AL, Nunes MB, Borges MAR (2018) Risk of malignancy in thyroid nodules using the American College of Radiology thyroid imaging reporting and data system in the NIFTP era. Horm Metab Res 50:735–737
Skowronska A, Milczarek-Banach J, Wiechno W et al (2018) Accuracy of the European thyroid imaging reporting and data system (EU-TIRADS) in the valuation of thyroid nodule malignancy in reference to the post-surgery histological results. Pol J Radiol 83:e579–e586
Zheng Y, Xu S, Kang H, Zhan W (2018) A single-center retrospective validation study of the American College of Radiology thyroid imaging reporting and data system. Ultrasound Q 34:77–83
Ahmadi S, Oyekunle T, Jiang X et al (2019) A direct comparison of the ATA and TI-RADS ultrasound scoring systems. Endocr Pract 25:413–422
Ahn HS, Na DG, Baek JH, Sung JY, Kim JH (2019) False negative rate of fine-needle aspiration in thyroid nodules: impact of nodule size and ultrasound pattern. Head Neck 41:967–973
Chen L, Zhan J, Diao XH et al (2019) Additional value of superb microvascular imaging for thyroid nodule classification with the thyroid imaging reporting and data system. Ultrasound Med Biol 45:2040–2048
Gao L, Xi X, Jiang Y et al (2019) Comparison among TIRADS (ACR TI-RADS and KWAK- TI-RADS) and 2015 ATA guidelines in the diagnostic efficiency of thyroid nodules. Endocrine 64:90–96
Hong HS, Lee JY (2019) Diagnostic performance of ultrasound patterns by K-TIRADS and 2015 ATA guidelines in risk stratification of thyroid nodules and follicular lesions of undetermined significance. AJR Am J Roentgenol 213:444–450
Li X, Hou XJ, Du LY et al (2019) Virtual touch tissue imaging and quantification (VTIQ) combined with the American College of Radiology thyroid imaging reporting and data system (ACR TI-RADS) for malignancy risk stratification of thyroid nodules. Clin Hemorheol Microcirc 72:279–291
Phuttharak W, Boonrod A, Klungboonkrong V, Witsawapaisan T (2019) Interrater reliability of various thyroid imaging reporting and data system (TIRADS) classifications for differentiating benign from malignant thyroid nodules. Asian Pac J Cancer Prev 20:1283–1288
Ruan JL, Yang HY, Liu RB et al (2019) Fine needle aspiration biopsy indications for thyroid nodules: compare a point-based risk stratification system with a pattern-based risk stratification system. Eur Radiol 29:4871–4878
Sahli ZT, Karipineni F, Hang JF et al (2019) The association between the ultrasonography TIRADS classification system and surgical pathology among indeterminate thyroid nodules. Surgery 165:69–74
Shen Y, Liu M, He J et al (2019) Comparison of different risk-stratification systems for the diagnosis of benign and malignant thyroid nodules. Front Oncol 9:378
Trimboli P, Ngu R, Royer B et al (2019) A multicentre validation study for the EU-TIRADS using histological diagnosis as a gold standard. Clin Endocrinol (Oxf) 91:340–347
Wildman-Tobriner B, Buda M, Hoang JK et al (2019) Using artificial intelligence to revise ACR TI-RADS risk stratification of thyroid nodules: diagnostic accuracy and utility. Radiology 292:112–119
Xu T, Wu Y, Wu RX et al (2019) Validation and comparison of three newly-released thyroid imaging reporting and data systems for cancer risk determination. Endocrine 64:299–307
Yoon SJ, Na DG, Gwon HY et al (2019) Similarities and differences between thyroid imaging reporting and data systems. AJR Am J Roentgenol 213:W76–W84
Russ G (2016) Risk stratification of thyroid nodules on ultrasonography with the French TI-RADS: description and reflections. Ultrasonography 35:25–38
Perros P, Boelaert K, Colley S et al (2014) Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 81(Suppl 1):1–122
Davies L, Welch HG (2014) Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg 140:317–322
Ahn HS, Kim HJ, Welch HG (2014) Korea’s thyroid-cancer “epidemic”--screening and overdiagnosis. N Engl J Med 371:1765–1767
Borenstein M, Hedges LV, Higgins JPT, Rothstein H (2009) Introduction to meta-analysis, 1st edn. Wiley, West Sussex
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (grant number NRF-2019R1G1A1099743).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Sang Hyun Choi.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors (Sang Hyun Choi) has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because this study was meta-analysis.
Ethical approval
Institutional Review Board approval was not required because this study was meta-analysis.
Methodology
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 519 kb)
Rights and permissions
About this article
Cite this article
Kim, D.H., Chung, S.R., Choi, S.H. et al. Accuracy of thyroid imaging reporting and data system category 4 or 5 for diagnosing malignancy: a systematic review and meta-analysis. Eur Radiol 30, 5611–5624 (2020). https://doi.org/10.1007/s00330-020-06875-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06875-w