Abstract
Purpose
To assess the added value of dynamic contrast-enhanced (DCE) in prostate MR in clinical practice.
Methods
Two hundred sixty-four patients underwent prostate MRI, with T2 and DWI sequences initially interpreted, prior to full multiparametric magnetic resonance imaging (mpMRI) interpretation using a Likert 1–5 scale. A prospective opinion was given on likely benefit of contrast prior to review of the DCE sequence, and retrospectively following full mpMRI review. The final histology result following targeted and/or systematic biopsy of the prostate was used for outcome purposes.
Results
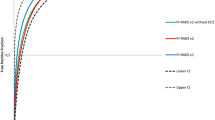
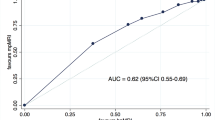
Biparametric magnetic resonance imaging (bpMRI) and mpMRI were assigned the same score in 86% of cases; when dichotomising to a negative or positive MRI (Likert score ≥ 3), concordance increased to 92.8%. At Likert score ≥ 3 bpMRI detected 89.9% of all cancers and 93.5% clinically significant prostate cancers (csPCa) and mpMRI 90.7% and 94.6%, respectively. mpMRI had fewer false positives than bpMRI (11.4% vs 18.9%) and a lower Likert 3 rate (8.3% vs 17%), conferring higher specificity (74% vs 67%), but similar sensitivity (95% versus 94%) and ROC-AUC (90% vs 89%). At a positive MRI threshold of Likert ≥ 4, mpMRI had a higher sensitivity than bpMRI (89% versus 80%) and detected more csPCa (89.2% versus 79.6%). DCE was prospectively considered of potential benefit in 27.3%, but readers would only recall 11% of patients for DCE sequences, mainly to assess score 3 peripheral zone lesions. Following full mpMRI review, DCE was considered helpful in 28.4% of cases; in 23/75 (30.6%) of these cases this only became apparent after reviewing the sequence, reasons included increased confidence, presence of “safety-net” lesions or inflammatory lesions.
Conclusion
BpMRI has equivalent cancer detection rates to mpMRI; however, mpMRI had fewer Likert 3 call rates and increased specificity and was subjectively considered of benefit by readers in 28.4% of cases.
Key Points
• bpMRI has similar cancer detection rates to the full mpMRI protocol at a positive MRI threshold of Likert 3.
• mpMRI had fewer intermediate category 3 calls (8.3%) than bpMRI (17%) and fewer false positives than bpMRI (11.4% vs 18.9%), conferring higher specificity (74% vs 67%).
• Readers considered DCE beneficial in 28.4% of cases, but in a relatively high number (30.6%) this only became apparent after reviewing the sequence.






Similar content being viewed by others
Abbreviations
- 3D-FSPGR:
-
Three-dimensional fast spoiled gradient-echo
- ADC:
-
Apparent diffusion coefficient
- AUC:
-
Area under the curve
- Bp:
-
Biparametric
- csPCa:
-
Clinically significant prostate cancer
- DCE:
-
Dynamic contrast-enhanced
- DWI:
-
Diffusion-weighted imaging
- ESUR:
-
European Society of Urogenital Radiology
- FOV:
-
Field-of-view
- iPCa:
-
Insignificant prostate cancer
- IQR:
-
Inter quartiles ranges
- ISUP:
-
International Society of Urological Pathology
- Mp:
-
Multiparametric
- MRI:
-
Magnetic resonance imaging
- PI-RADS:
-
Prostate Imaging Reporting and Data System
- PSA:
-
Prostate-specific antigen
- PZ:
-
Peripheral zone
- ROC:
-
Receiver operating characteristic
- SD:
-
standard deviation
- TE:
-
Time of echo
- TR:
-
Time of repetition
- TZ:
-
Transition zone
- US:
-
Ultrasound
References
Ahmed HU, El-Shater Bosaily A, Brown LC et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389:815–822
Kasivisvanathan V, Rannikko AS, Borghi M et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378:1767–1777
Rouvière O, Puech P, Renard-Penna R et al (2019) Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): a prospective, multicentre, paired diagnostic study. Lancet Oncol 20(1):100–109
Van der Leest M, Cornel E, Israel B et al (2019) Head-to-head comparison of transrectal ultrasound-guided prostate biopsy versus multiparametric prostate resonance imaging with subsequent magnetic resonance-guided biopsy in biopsy-naïve men with elevated prostate-specific antigen: a large prospective multicenter clinical study. Eur Urol 75(4):570–578
Weinreb JC, Barentsz JO, Choyke PL et al (2016) PI-RADS prostate imaging – reporting and data system: 2015, version 2. Eur Urol 69:16–40
Turkbey B, Rosenkrantz AB, Haider MA et al (2019) Prostate Imaging Reporting and Data System Version 2.1: 2019 update of prostate imaging reporting and data system version 2. Eur Urol 76(3):340–351
Richenberg JL (2016) PI-RADS: past, present and future. Clin Radiol 71(1):23–24
Mowatt G, Scotland G, Boachie C et al (2013) The diagnostic accuracy and cost-effectiveness of magnetic resonance spectroscopy and enhanced magnetic resonance imaging techniques in aiding the localisation of prostate abnormalities for biopsy: a systematic review and economic evaluation. Health Technol Assess 17:1–281
Beomonte Zobel B, Quattrocchi CC, Errante Y, Grasso RF (2016) Gadolinium-based contrast agents: did we miss something in the last 25 years? Radiol Med 121:478–481
Di Campli E, Delli Pizzi A, Seccia B et al (2018) Diagnostic accuracy of biparametric vs multiparametric MRI in clinically significant prostate cancer: comparison between readers with different experience. Eur J Radiol 101:17–23
Kuhl CK, Bruhn R, Krämer N, Nebelung S, Heidenreich A, Schrading S (2017) Abbreviated biparametric prostate MR imaging in men with elevated prostate-specific antigen. Radiology 285:493–505
Thestrup KC, Logager V, Baslev, Møller JM, Hansen RH, Thomsen HS (2016) Biparametric versus multiparametric MRI in the diagnosis of prostate cancer. Acta Radiol Open 5:2058460116663046
De Visschere P, Lumen N, Ost P, Decaestecker K, Pattyn E, Villeirs G (2017) Dynamic contrast-enhanced imaging has limited added value over T2-weighted imaging and diffusion-weighted imaging when using PI-RADSv2 for diagnosis of clinically significant prostate cancer in patients with elevated PSA. Clin Radiol 72:23–32
Vargas HA, Hötker AM, Goldman DA et al (2016) Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur Radiol 26(6):1606–1612
Boesen L, Nørgaard N, Løgager V et al (2018) Assessment of the diagnostic accuracy of biparametric magnetic resonance imaging for prostate cancer in biopsy-naive men: the Biparametric MRI for Detection of Prostate Cancer (BIDOC) Study. JAMA Netw Open 1(2):e180219
Jambor I, Bostrom PJ, Taimen P et al (2017) Novel biparametric MRI and targeted biopsy improves risk stratification in men with a clinical suspicion of prostate cancer (IMPROD trial). J Magn Reson Imaging 46(4):1089–1095
Wassberg C, Akin O, Vargas HA, Shukla-Dave A, Zhang J, Hricak H (2012) The incremental value of contrast-enhanced MRI in the detection of biopsy-proven local recurrence of prostate cancer after radical prostatectomy: effect of reader experience. AJR Am J Roentgenol 199(2):360–366
Latifoltojar A, Appayya MB, Barrett T, Punwani S (2019) Similarities and differences between Likert and PIRADS v2.1 scores of prostate multiparametric MRI: a pictorial review of histology-validated cases. Clin Radiol 74(11):895. e1–895.e15
Barentsz JO, Richenberg J, Clements R et al (2012) ESUR prostate MR guidelines 2012. Eur Radiol 22(4):746–757
Barrett T, Turkbey B, Choyke PL (2015) PI-RADS version 2: what you need to know. Clin Radiol 70(11):1165–1176
Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL; ISUP Grading Committee (2005) ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol 29(9):1228–1242
Stanzione A, Imbriaco M, Cocozza S et al (2016) Biparametric 3T magnetic resonance imaging for prostatic cancer detection in a biopsy-naive patient population: a further improvement of PI-RADS v2? Eur J Radiol 85(12):2269–2274
Scialpi M, Prosperi E, D’Andrea A et al (2017) Biparametric versus multiparametric MRI with non-endorectal coil at 3T in the detection and localization of prostate cancer. Anticancer Res 37(3):1263–1271
Junker D, Steinkohl F, Fritz V et al (2019) Comparison of multiparametric and biparametric MRI of the prostate: are gadolinium-based contrast agents needed for routine examinations? World J Urol 37(4):691–699
Gatti M, Faletti R, Calleris G et al (2019) Prostate cancer detection with biparametric magnetic resonance imaging (bpMRI) by readers with different experience: performance and comparison with multiparametric (mpMRI). Abdom Radiol (NY) 44(5):1883–1893
Burn PR, Freeman SJ, Andreou S, Burns-Cox N, Persad R, Barrett T (2019) A multi-centre assessment of prostate MRI quality and compliance with UK and international standards. Clin Radiol 74:894.e19–894.e25
Hötker AM, Mazaheri Y, Zheng J et al (2015) Prostate Cancer: assessing the effects of androgen-deprivation therapy using quantitative diffusion-weighted and dynamic contrast-enhanced MRI. Eur Radiol 25(9):2665–2672
Barrett T, Davidson SR, Wilson BC, Weersink RA, Trachtenberg J, Haider MA (2014) Dynamic contrast enhanced MRI as a predictor of vascular-targeted photodynamic focal ablation therapy outcome in prostate cancer post-failed external beam radiation therapy. Can Urol Assoc J 8(9–10):E708–E714
Barrett T, Gill AB, Kataoka MY et al (2012) DCE and DW MRI in monitoring response to androgen deprivation therapy in patients with prostate cancer: a feasibility study. Magn Reson Med 67(3):778–785
Caglic I, Hansen NL, Slough RA, Patterson AJ, Barrett T (2017) Evaluating the effect of rectal distension on prostate multiparametric MRI image quality. Eur J Radiol 90:174–180
Padhani AR, Weinreb J, Rosenkrantz AB, Villeirs G, Turkbey B, Barentsz J (2019) Prostate Imaging-Reporting and Data System Steering Committee: PI-RADS v2 status update and future directions. Eur Urol 75(3):385–396
Scialpi M, Martorana E, Aisa MC, Rondoni V, D'Andrea A, Bianchi G (2017) Score 3 prostate lesions: a gray zone for PI-RADS v2. Turk J Urol 3:43
Hansen NL, Koo BC, Warren AY, Kastner C, Barrett T (2017) Sub-differentiating equivocal PI-RADS-3 lesions in multiparametric magnetic resonance imaging of the prostate to improve cancer detection. Eur J Radiol 95:307–313
Barrett T, Slough RA, Sushentsev N et al (2019) Three-year experience of a dedicated prostate mpMRI pre-biopsy programme and effect on timed cancer diagnostic pathways. Clin Radiol 74(11):894.e1–894.e9
Greer MD, Shih JH, Lay N, Barrett T et al (2017) Validation of the dominant sequence paradigm and role of dynamic contrast-enhanced imaging in PI-RADS version 2. Radiology 285(3):859–869
Barrett T, Rajesh A, Rosenkrantz AB et al (2019) PI-RADS version 2.1 - one small step for prostate MRI. Clin Radiol 74(11):841–852
Gaziev G, Wadhwa K, Barrett T et al (2016) Defining the learning curve for multiparametric magnetic resonance imaging (MRI) of the prostate using MRI-transrectal ultrasonography (TRUS) fusion-guided transperineal prostate biopsies as a validation tool. BJU Int 117(1):80–86
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Tristan Barrett.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zawaideh, J.P., Sala, E., Shaida, N. et al. Diagnostic accuracy of biparametric versus multiparametric prostate MRI: assessment of contrast benefit in clinical practice. Eur Radiol 30, 4039–4049 (2020). https://doi.org/10.1007/s00330-020-06782-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06782-0