Abstract
Purpose
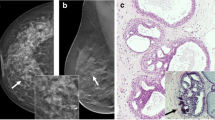
To evaluate the diagnostic performance of dynamic contrast-enhanced (DCE)–MRI in predicting malignancy after percutaneous biopsy diagnosis of atypical ductal hyperplasia (ADH).
Methods and materials
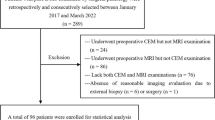
In this retrospective study, 68 lesions (66 women) with percutaneous biopsy diagnosis of ADH and pre-operative breast DCE-MRI performed between January 2016 and December 2017 were included. Two radiologists reviewed in consensus mammography, ultrasound, and MR images. The final diagnosis after surgical excision was used as standard of reference. Clinical and imaging features were compared in patients with and without upgrade to malignancy after surgery. The diagnostic performance of DCE-MRI in predicting malignant upgrade was evaluated.
Results
A 9-gauge vacuum-assisted biopsy was performed in 40 (58.8%) cases and a 14-gauge core needle biopsy in 28 (41.2%) cases. Upgrade to malignancy was observed in 17/68 (25%) lesions, including 4/17 (23.5%) cases of invasive cancer and 13/17 (76.5%) cases of ductal carcinoma in situ (DCIS). In 16/17 (94.1%) malignant and 20/51 (39.2%) benign lesions, a suspicious enhancement could be recognized in DCE-MRI. The malignant lesion without suspicious enhancement was a low-grade DCIS (4 mm size). Sensitivity, specificity, positive predictive value, and negative predictive value of DCE-MRI on predicting malignancy were respectively 94.1%, 60.7%, 44.4%, and 96.8%. No other clinical or imaging features were significantly different in patients with and without upgrade to malignancy.
Conclusion
After a percutaneous biopsy diagnosis of ADH, malignancy can be ruled out in most of the cases, if no suspicious enhancement is present in the biopsy area at DCE-MRI. Breast DCE-MRI may be used to avoid surgery in more than half of the patients with final benign diagnosis.
Key Points
• Breast DCE-MRI can safely rule out malignancy if no suspicious enhancement is present in the biopsy area after a percutaneous biopsy diagnosis of ADH.
• All cases of upgrade to high-grade DCIS and invasive cancers can be identified at breast DCE-MRI after a percutaneous biopsy diagnosis of ADH.
• Breast DCE-MRI may be used to avoid surgery in more than half of the patients with final benign diagnosis.






Similar content being viewed by others
Abbreviations
- ADH:
-
Atypical ductal hyperplasia
- BI-RADS:
-
Breast imaging reporting and data system
- CNB:
-
Core needle biopsy
- DCE-MRI:
-
Dynamic contrast-enhanced MRI
- DCIS:
-
Ductal carcinoma in situ
- DWI:
-
Diffusion-weighted imaging
- FOV:
-
Field of view
- HG:
-
High grade
- IDC:
-
Invasive ductal carcinoma
- IG:
-
Intermediate grade
- LG:
-
Low grade
- ME:
-
Mass enhancement
- NME:
-
Non-mass enhancement
- VAB:
-
Vacuum-assisted biopsy
References
Darling MLR, Smith DN, Lester SC et al (2000) Atypical ductal hyperplasia and ductal carcinoma in situ as revealed by large-core needle breast biopsy: results of surgical excision. AJR Am J Roentgenol 175:1341–1346
Jackman RJ, Burbank F, Parker SH et al (1997) Atypical ductal hyperplasia diagnosed at stereotactic breast biopsy: improved reliability with 14-gauge, directional, vacuum-assisted biopsy. Radiology 204:485–488
Jackman RJ, Nowels KW, Rodriguez-Soto J, Marzoni FA, Finkelstein SI, Shepard MJ (1999) Stereotactic, automated, large-core needle biopsy of nonpalpable breast lesions: false-negative and histologic underestimation rates after long-term follow-up. Radiology 210:799–805
Liberman L, Cohen MA, Dershaw DD, Abramson AF, Hann LE, Rosen PP (1995) Atypical ductal hyperplasia diagnosed at stereotaxic core biopsy of breast-lesions - an indication for surgical biopsy. AJR Am J Roentgenol 164:1111–1113
Pandelidis S, Heilman D, Jones D, Stough K, Trapeni J, Suliman Y (2003) Accuracy of 11-gauge vacuum-assisted core biopsy of mammographic breast lesions. Ann Surg Oncol 10:43–47
Sohn V, Arthurs Z, Herbert G et al (2007) Atypical ductal hyperplasia: improved accuracy with the 11-gauge vacuum-assisted versus the 14-gauge core biopsy needle. Ann Surg Oncol 14:2497–2501
Tavassoli FA, Norris HJ (1990) A comparison of the results of long-term follow-up for atypical intraductal hyperplasia and intraductal hyperplasia of the breast. Cancer 65:518–529
Jang M, Cho N, Moon WK, Park JS, Seong MH, Park IA (2008) Underestimation of atypical ductal hyperplasia at sonographically guided core biopsy of the breast. AJR Am J Roentgenol 191:1347–1351
Liberman L, Holland AE, Marjan D et al (2007) Underestimation of atypical ductal hyperplasia at MRI-guided 9-gauge vacuum-assisted breast biopsy. AJR Am J Roentgenol 188:684–690
Londero V, Zuiani C, Linda A, Battigelli L, Brondani G, Bazzocchi M (2011) Borderline breast lesions: comparison of malignancy underestimation rates with 14-gauge core needle biopsy versus 11-gauge vacuum-assisted device. Eur Radiol 21:1200–1206
Villa A, Tagliafico A, Chiesa F, Chiaramondia M, Friedman D, Calabrese M (2011) Atypical ductal hyperplasia diagnosed at 11-gauge vacuum-assisted breast biopsy performed on suspicious clustered microcalcifications: could patients without residual microcalcifications be managed conservatively? AJR Am J Roentgenol 197:1012–1018
Youk JH, Kim EK, Kim MJ (2009) Atypical ductal hyperplasia diagnosed at sonographically guided 14-gauge core needle biopsy of breast mass. AJR Am J Roentgenol 192:1135–1141
Eby PR, Ochsner JE, DeMartini WB, Allison KH, Peacock S, Lehman CD (2009) Frequency and upgrade rates of atypical ductal hyperplasia diagnosed at stereotactic vacuum-assisted breast biopsy: 9-versus 11-gauge. AJR Am J Roentgenol 192:229–234
Rageth CJ, O’Flynn EAM, Comstock C et al (2016) First International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 159:203–213
Rageth CJ, O’Flynn EAM, Pinker K et al (2018) Second International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 174:279–296
Deshaies I, Provencher L, Jacob S et al (2011) Factors associated with upgrading to malignancy at surgery of atypical ductal hyperplasia diagnosed on core biopsy. Breast 20:50–55
Liberman L, Smolkin JH, Dershaw DD, Morris EA, Abramson AF, Rosen PP (1998) Calcification retrieval at stereotactic, 11-gauge, directional, vacuum-assisted breast biopsy. Radiology 208:251–260
Philpotts LE, Lee CH, Horvath LJ, Lange RC, Carter D, Tocino I (2000) Underestimation of breast cancer with II-gauge vacuum suction biopsy. AJR Am J Roentgenol 175:1047–1050
Sneige N, Lim SC, Whitman GJ et al (2003) Atypical ductal hyperplasia diagnosis by directional vacuum-assisted stereotactic biopsy of breast microcalcifications. Considerations for surgical excision. Am J Clin Pathol 119:248–253
Forgeard C, Benchaib M, Guerin N et al (2008) Is surgical biopsy mandatory in case of atypical ductal hyperplasia on 11-gauge core needle biopsy? A retrospective study of 300 patients. Am J Surg 196:339–345
Hong ZJ, Chu CH, Fan HL et al (2011) Factors predictive of breast cancer in open biopsy in cases with atypical ductal hyperplasia diagnosed by ultrasound-guided core needle biopsy. Eur J Surg Oncol 37:758–764
Tsuchiya K, Mori N, Schacht DV et al (2017) Value of breast MRI for patients with a biopsy showing atypical ductal hyperplasia (ADH). J Magn Reson Imaging 46:1738–1747
Linda A, Zuiani C, Bazzocchi M, Furlan A, Londero V (2008) Borderline breast lesions diagnosed at core needle biopsy: can magnetic resonance mammography rule out associated malignancy? Preliminary results based on 79 surgically excised lesions. Breast 17:125–131
Linda A, Zuiani C, Furlan A et al (2012) Nonsurgical management of high-risk lesions diagnosed at core needle biopsy: can malignancy be ruled out safely with breast MRI? AJR Am J Roentgenol 198:272–280
Pediconi F, Padula S, Dominelli V et al (2010) Role of breast MR imaging for predicting malignancy of histologically borderline lesions diagnosed at core needle biopsy: prospective evaluation. Radiology 257:653–661
D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA et al (2013) ACR BI-RADS Atlas, breast imaging reporting and data system. American College of Radiology, Reston, VA
Morris EA, Comstock CE, Lee CH et al (2013) ACR BI-RADS magnetic resonance imaging. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System, Reston, VA
de Beca FF, Rasteiro C, Correia A, Costa S, Amendoeira I (2013) Improved malignancy prediction by B3 breast lesions subclassification. Ann Diagn Pathol 17:434–436
Sagara Y, Mallory MA, Wong S et al (2015) Survival benefit of breast surgery for low-grade ductal carcinoma in situ a population-based cohort study. JAMA Surg 150:739–745
Strigel RM, Eby PR, DeMartini WB et al (2010) Frequency, upgrade rates, and characteristics of high-risk lesions initially identified with breast MRI. AJR Am J Roentgenol 195:792–798
Crystal P, Sadaf A, Bukhanov K, McCready D, O’Malley F, Helbich TH (2011) High-risk lesions diagnosed at MRI-guided vacuum-assisted breast biopsy: can underestimation be predicted? Eur Radiol 21:582–589
Fischer U, Klopka L, Grabbe E (1999) Breast carcinoma: effect of preoperative contrast-enhanced MR imaging on the therapeutic approach. Radiology 213(3):881–888
Dietzel M, Baltzer PAT (2018) How to use the Kaiser score as a clinical decision rule for diagnosis in multiparametric breast MRI: a pictorial essay. Insights Imaging 9:325–335
Caplain A, Drouet Y, Peyron M et al (2014) Management of patients diagnosed with atypical ductal hyperplasia by vacuum-assisted core biopsy: a prospective assessment of the guidelines used at our institution. Am J Surg 208:260–267
Mesurolle B, Perez JCH, Azzumea F et al (2014) Atypical ductal hyperplasia diagnosed at sonographically guided core needle biopsy: frequency, final surgical outcome, and factors associated with underestimation. AJR Am J Roentgenol 202:1389–1394
Grady I, Gorsuch H, Wilburn-Bailey S (2005) Ultrasound-guided, vacuum-assisted, percutaneous excision of breast lesions: an accurate technique in the diagnosis of atypical ductal hyperplasia. J Am Coll Surg 201:14–17
Liberman L, Hann LE, Dershaw DD, Morris EA, Abramson AF, Rosen PP (1997) Mammographic findings after stereotactic 14-gauge vacuum biopsy. Radiology 203:343–347
Salem C, Sakr R, Chopier J, Antoine M, Uzan S, Darai E (2009) Pain and complications of directional vacuum-assisted stereotactic biopsy: comparison of the Mammotome and Vacora techniques. Eur J Radiol 72:295–299
Hartmann LC, Radisky DC, Frost MH et al (2014) Understanding the premalignant potential of atypical hyperplasia through its natural history: a longitudinal cohort study. Cancer Prev Res (Phila) 7:211–217
Hartmann LC, Sellers TA, Frost MH et al (2005) Benign breast disease and the risk of breast cancer. N Engl J Med 353:229–237
Page DL, Dupont WD, Rogers LW, Rados MS (1985) Atypical hyperplastic lesions of the female breast - a long-term follow-up-study. Cancer 55:2698–2708
Sanders ME, Schuyler PA, Dupont WD, Page DL (2005) The natural history of low-grade ductal carcinoma in situ of the breast in women treated by biopsy only revealed over 30 years of long-term follow-up. Cancer 103:2481–2484
Collins LC, Baer HJ, Tamimi RM, Connolly JL, Colditz GA, Schnitt SJ (2006) The influence of family history on breast cancer risk in women with biopsy-confirmed benign breast disease - results from the nurses’ health study. Cancer 107:1240–1247
Degnim AC, Visscher DW, Berman HK et al (2007) Stratification of breast cancer risk in women with atypia: a Mayo cohort study. J Clin Oncol 25:2671–2677
Baer HJ, Collins LC, Connolly JL, Colditz GA, Schnitt SJ, Tamimi RM (2009) Lobule type and subsequent breast cancer risk: results from the nurses’ health studies. Cancer 115:1404–1411
Milanese TR, Hartmann LC, Sellers TA et al (2006) Age-related lobular involution and risk of breast cancer. J Natl Cancer Inst 98:1600–1607
Dietzl M, Wenkel E, Hammon M et al (2019) Does higher filed strength translate into better diagnostic accuracy? A prospective comparison of breast MRI at 3 and 1.5 tesla. Eur J Radiol 114:51–56
Kuhl CK, Strobel K, Bieling H et al (2017) Impact of preoperative breast MR imaging and MR-guided surgery on diagnosis and surgical outcome of women with invasive breast cancer with and without DCIS component. Radiology 284:645–655
Hata T, Takahashi H, Watanabe K et al (2004) Magnetic resonance imaging for preoperative evaluation of breast cancer: a comparative study with mammography and ultrasonography. J Am Coll Surg 198:190–197
Proulx F, Correa JA, Ferre R et al (2016) Value of pre-operative breast MRI for the size assessment of ductal carcinoma in situ. Br J Radiol 89:20150543
Baltzer A, Dietzel M, Kaiser CG, Baltzer PA (2016) Combined reading of contrast enhanced and diffusion weighted magnetic resonance imaging by using a simple sum score. Eur Rad 26(3):884–891
Acknowledgments
The authors thank Suzanne Potter for reading and correcting the manuscript.
Funding
This work was supported by a grant of “Promedica-Stiftung” to M. Marcon. The funding source was not involved in study design, in collection, analysis, and interpretation of data, in manuscript writing, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Magda Marcon.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Cross-sectional study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bertani, V., Urbani, M., La Grassa, M. et al. Atypical ductal hyperplasia: breast DCE-MRI can be used to reduce unnecessary open surgical excision. Eur Radiol 30, 4069–4081 (2020). https://doi.org/10.1007/s00330-020-06701-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06701-3