Abstract
Objectives
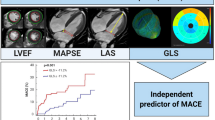
Global left ventricular (LV) function is routinely used to assess cardiac function; however, myocardial strain is able to identify more subtle dysfunction. We aimed to determine the recovery and prognostic value of featuring tracking (FT) cardiovascular magnetic resonance (CMR) strain in ST-segment elevation myocardial infarction (STEMI) patients with a concurrent chronic total occlusion (CTO).
Methods
In the randomized EXPLORE trial, there was no significant difference in global LV function after percutaneous coronary intervention (PCI) of the CTO, compared with no-CTO PCI, post-STEMI. In the current study, we included 200 of the 302 EXPLORE patients with a baseline CMR, of which 180 also had 4-month follow-up (serial) CMR. Global longitudinal strain (GLS) was calculated from 3 long-axis views. Global circumferential strain (GCS) and segmental strain were calculated from 3 short-axis views (basal, mid, and apical).
Results
Global strain significantly improved at 4 months (GLS ∆ − 1.8 ± 4.3%, p < 0.001; GCS ∆ − 1.7 ± 4.7%, p < 0.001); however, there was no treatment effect of CTO-PCI on strain recovery. GLS was a significant predictor for 4 months of LV ejection fraction (p = 0.006), incremental to other CMR parameters including infarct size. For mortality, infarct size remained the strongest predictor. On regional level, segmental strain independently predicted recovery in the dysfunctional segments (p < 0.001).
Conclusions
Global and segmental myocardial strains significantly improved over time, with no effect of CTO-PCI. Global strain was associated with outcome and segmental strain was an independent predictor for regional LV recovery in the dysfunctional CTO territory. Further research is needed to determine the additional prognostic value of strain beyond routine CMR parameters.
Key Points
• In STEMI patients with a concurrent CTO, strain significantly improves over time, regardless of CTO-PCI.
• Global strain is an independent predictor for functional recovery, incremental to infarct size, LVEF, and clinical parameters.
• Segmental strain was able to predict the recovery of wall thickening, incremental to transmural extent of infarction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular magnetic resonance (CMR) is frequently used for non-invasive assessment of global left ventricular (LV) function and infarct size, which can be used as surrogate endpoints to predict clinical outcome of ST-segment elevation myocardial infarction (STEMI) patients [1]. However, more subtle but important contractile changes might not be detected, as these do not always lead to a decline in global LV function. Currently, new techniques, such as myocardial strain parameters, are therefore gaining more interest as they are able to identify subtle myocardial deformation, are less subjective, and are less experience-dependent [2]. The reference method for the quantification of cardiac LV deformation is myocardial tissue tagging; however, this technique requires additional image acquisition and post-processing analysis and is therefore more time-consuming [3]. CMR-based feature tracking (FT) is novel and highly correlated with myocardial tissue tagging, but it is more clinically feasible as it uses the steady-state free-precision cine images acquired with standard CMR protocols [2, 4]. FT-CMR provides a fast and accurate assessment of myocardial strain by following the border tracking over time and defining the relative change in length of the myocardial segment [5]. FT-CMR is reproducible and comparable values are provided with different software methods [6, 7]. Global longitudinal strain (GLS) and global circumferential strain (GCS) are suggested to be more sensitive in detecting myocardial contractility changes before there is a change in global LV parameters and also to be less variable when compared with LV ejection fraction (LVEF) and wall motion analysis [8].
In STEMI patients with a concurrent chronic total occlusion (CTO), neither the recovery and prediction of outcome using global and segmental strains have thus far been examined nor the effect of additional percutaneous coronary intervention (PCI) of the CTO on the recovery of strain. Currently, the treatment of the (accidently) found concurrent CTO in STEMI patients during primary PCI remains controversial. Observational data have suggested beneficial effects of CTO-PCI [9]. However, the first randomized Evaluating Xience and left ventricular function in PCI on occlusiOns afteR STEMI (EXPLORE) trial, which included STEMI patients, after successful primary PCI, with a CTO and randomized patients to either CTO-PCI or no-CTO PCI, showed no beneficial effect on global LV function (LVEF and LVEDV) [10]. We used the patients included in the EXPLORE trial to (1) investigate the recovery in global and segmental strain parameters from baseline to follow-up, (2) study the effect of CTO-PCI on this recovery, and (3) determine the incremental prognostic value of global and segmental strains in predicting functional and clinical outcomes.
Methods
In the current sub-study from the EXPLORE trial, we included all patients who underwent a baseline CMR (200 of the 302 patients), of which 180 patients also had a 4-month CMR (serial CMR). This cohort of patients with serial CMR has been described before [11]. In these 200 patients, offline strain analysis was performed; the other patients (n = 102) were excluded because they lacked a baseline CMR (a baseline CMR was not mandatory in the study protocol). Details regarding the design and results of the EXPLORE trial were previously reported [10, 12]. In short, the randomized multi-center clinical EXPLORE trial included 302 STEMI patients with a concurrent CTO and randomized them in a 1:1 ratio to CTO-PCI within 7 days after primary PCI (n = 148) or to a conservative strategy (no-CTO PCI) for at least 4 months (n = 154). Important inclusion criteria were the following: a concurrent CTO in a non-infarct-related artery found during successful primary PCI for STEMI and the CTO had to be located in a coronary vessel with a reference diameter of at least 2.5 mm. Among the exclusion criteria were the following: > 48 hemodynamic instability and factors precluding reliable CMR imaging (atrial fibrillation, severe renal insufficiency, and pacemakers or implantable cardioverter-defibrillators). Full inclusion and exclusion criteria are summarized in the Supplemental File. CTO definition was a 100% luminal narrowing without antegrade flow. An independent angiography corelab assessed all coronary angiographies. There were no significant differences in the primary outcomes of LVEF and LV end-diastolic volume (LVEDV) at 4 months of follow-up in patients randomized to CTO-PCI compared with no-CTO PCI, nor on LV systolic volume, LV mass, and infarct size.
CMR protocol
All CMRs were performed on a 1.5-Tesla scanner using a dedicated phased array cardiac receiver coil. ECG-gated steady-state free-precession cine images for LV function imaging were obtained, during repeated breath holds, in long-axis orientation (2-, 3-, and 4-chamber views) and in short-axis orientation covering the left ventricle from base to apex. Late gadolinium-enhanced (LGE) images were acquired using an inversion recovery gradient-echo pulse sequence with slice locations identical to the cine images to identify the size and extent of infarction. Images were acquired at least 10 min after administration of a gadolinium-based contrast agent in a dosage of 0.2 mmol/kg of body weight. Transmurality of scar tissue of the myocardium was assessed in patients who underwent baseline CMR of sufficient quality. To assess viability, transmural extent of infarction (TEI) was used, TEI of 0–50% per segment was considered viable [13].
Wall thickening
The analysis of segmental wall thickening has been described before [11]. An independent core laboratory, blinded for randomization outcome, analyzed all CMR images (ClinFact Corelab using QMass MR analytical software version 7.6, Medis BV). A 16-segment model, excluding the apex, was used to analyze wall thickening. Endo- and epicardial borders on the end-diastolic and end-systolic images were manually outlined on all short-axis cine slices. Segmental wall thickening was defined as a percentage increase of LV wall thickness during systole compared with diastole. Myocardial segments were considered dysfunctional if wall thickening was less than 45% [14]. Individual segments for each patient were assigned to one of the major coronary arteries using the American Heart Association standardized myocardial segmentation and nomenclature statement [15]. Myocardial segments were assigned to the CTO, infarct, or remote territory using this standard model (in relation to the coronary anatomy scored by the angiographic corelab).
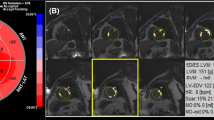
Strain analysis
Strain measurements were performed offline using the FT-CMR software method of Medis QStrain Software (Medis Medical Imaging Systems, version 2.0.12.2.) (example of the analysis is in the Supplementary File). All three longitudinal-axis views (2-, 3-, and 4-chamber) were used to determine peak GLS. Endocardial contours were manually drawn during end-diastole and end-systole with subsequent automatic tracking during the cardiac cycle. As an example, a cine CMR movie file of the endocardial tracking is available as additional files 1 and 2. For the assessment of GCS and segmental circumferential strain, the corelab contours for the short-axis images were used. Peak GCS was calculated from 3 short-axis views (basal, mid, and apical). For peak segmental strain, short-axis images were used to define the segments according to the 16-segment model after manual insertion of a reference point (delineated at the anterior insertion of the right ventricle). All studies were loaded into the software and analyzed in a random order by one investigator blinded for randomization outcome under supervision of a CMR cardiologist with > 15-year experience (JE, supervisor: AH). The reproducibility of GLS measurements was assessed in 30 CMR scans (15 patients with baseline and follow-up CMR). The intraclass correlation coefficient for interobserver agreement was 0.97 (95% CI 0.89 to 0.99; p < 0.001).
Clinical outcomes
At 4 months and 1, 2, 3, 4, and 5 years, clinical follow-up was collected to assess survival status. Survival data were censored at 5 years or known date of last contact [16].
Statistical analysis
Data are presented as mean ± standard deviation for continuous variables. Discrete variables are presented as frequencies and percentages. Baseline characteristics were compared using the independent-samples t test, or Fisher’s exact probability test in case of binary endpoints. Analyses were performed on intention-to-treat analysis. Changes in GLS and GCS within each group were tested with paired Student’s t test. Pearson’s correlation coefficient analysis was used to assess the relationship between the global strain and LV function parameters. Multivariable linear regression was used for testing the contribution of baseline, angiographic, and CMR characteristics in relation to LVEF at follow-up. Stepwise forward selection of variables was used; all variables with a p value < 0.05 were included and variables with a p value > 0.10 were removed from the model. Cumulative event rates of long-term mortality were estimated using Kaplan-Meier curves, and the Log rank statistic was used for comparing the survival curves. Hazard ratios for long-term mortality were calculated, after verification of the proportional hazard assumption, using Cox proportional hazard regression analyses. We evaluated the recovery of segmental circumferential strain in dysfunctional segments at baseline. Because within 1 patient the regional strain in the different segments is strongly related and not an independent outcome, multilevel analysis was used (linear regression) [17]. The following fixed effects were included: randomization outcome and baseline segmental strain. Multilevel analysis was also used to look for predictors of regional wall thickening recovery, and the following fixed effects were included: baseline SWT, baseline transmural extent of infarction, presence of microvascular obstruction, randomization outcome, and baseline segmental strain. All tests were two-sided, and a p value < 0.05 was considered to indicate statistical significance. Statistical analysis was performed with the Statistical Package for Social Sciences software (SPSS version 23.0 for Windows).
Results
Baseline characteristics
The baseline characteristics of the 200 patients included in this study are shown in Supplement Table 1. Patients had a mean age of 60 ± 10 years and 88% was male. Mean baseline LVEF was 41 ± 12%, LVEDV 103 ± 25 ml/m2, and infarct size 12 ± 11 g. In the patients randomized to CTO-PCI, the PCI was performed on day 5 ± 2 after primary PCI. Baseline CMR was performed 4 ± 2 days after primary PCI. Baseline GLS was available in 184 patients and GCS in 176 patients. Serial GLS measurements were available in 166 and serial GCS in 160 patients (Fig. 1). GLS and GCS by FT-CMR were significantly correlated with LVEF, LVEDV, and infarct size (p < 0.0001 for all). Changes in strain parameters were also related to change in LVEF; however, change in LVEDV and infarct size showed poor correlation with change in global strain (Supplement Table 2).
Global myocardial strain at follow-up
GLS and GCS significantly improved from baseline to 4 months of follow-up (ΔGLS − 1.8 ± 4.3%, p < 0.001; ΔGCS − 1.7 ± 4.7%, p < 0.001) (Fig. 2). However, there was no treatment effect of CTO-PCI on the recovery of global strain parameters (∆GLS − 2.4 ± 4.2% versus − 1.4 ± 4.3%, p = 0.14; ∆GCS − 1.4 ± 4.5% versus − 1.9 ± 4.9%, p = 0.55) (Table 1).
Prognostic value of global strain
Both GLS and GCS were univariate predictors for LVEF at 4-month follow-up. In multivariate analysis, GLS remained a significant predictor for functional outcome (4-month LVEF) (ß − 0.40, 95% CI − 0.68 to − 0.12, p = 0.006), together with baseline LVEF, LVEDV, and presence of microvascular obstruction (MVO) (Table 2). By the Kaplan-Meier analysis, the patients in the lowest quartile GCS (GCS > − 14%) had a significantly worse survival compared with patients with GCS < − 14% (Fig. 3). During a median follow-up of 4.0 (2.2–5.0) years, 13 patients died (6.5%). Univariate predictors for long-term mortality were LVEF, LVEDV, and GCS. In stepwise forward multivariate analysis, GCS remained the strongest predictor for mortality (HR 1.17, 95% CI 1.04–1.31, p = 0.009) (Supplement Table 3). In 74% of the patients, infarct data was available; when including infarct size and MVO in the model, infarct size was the only significant CMR parameter predicting mortality (HR 1.07, 95% CI 1.03–1.11, p < 0.001).
Segmental circumferential strain at follow-up
There were 2560 segments available for serial segmental circumferential strain analysis (from n = 160 patients). Segmental strain was significantly recovered from baseline to 4-month follow-up in the dysfunctional segments (wall thickening < 45% at baseline; ∆ segmental strain − 2.4 (8.9), p < 0.001; Table 3). However, no significant difference was found between CTO-PCI and no-CTO PCI. Table 3 shows the recovery of segmental strain in the dysfunctional segments in the CTO. In the CTO territory, no significant difference was found on segmental strain between CTO-PCI and no-CTO PCI (∆ segmental strain − 2.5 ± 9.5% versus − 2.5% ± 8.5%, p = 0.50).
Prediction of wall thickening recovery with segmental strain
At baseline, 59% of the myocardial segments were dysfunctional (wall thickening < 45%). Of the dysfunctional segments, 74% was viable (TEI < 50%) and MVO was present in 13%. In a multivariate analysis, baseline wall thickening, segmental strain, and infarct (TEI) were all statistically significantly related; however, based on the t statistic, wall thickening and segmental strain were stronger predictors for wall thickening recovery compared with infarct or MVO. In the CTO territory, 59% of the segments were dysfunctional and 96% of the dysfunctional segments were viable (TEI < 50%). In multivariate analysis, segmental strain was an independent predictor for regional wall thickening recovery, incremental to baseline wall thickening and infarct (coefficient − 0.44, SE 0.14, t − 3.10, p = 0.002; Table 4).
Discussion
This is the first study evaluating the recovery and value of global and segmental myocardial strains in STEMI patients with a concurrent CTO, and the first to determine the effect of CTO-PCI on strain recovery. The main findings are the following: (1) Global and segmental strains improved over time, with no significant treatment effect of CTO-PCI; (2) GLS was a significant predictor for functional outcome incremental to infarct size, LV function, and clinical parameters; however, for mortality, infarct size remained the strongest predictor; and (3) segmental strain is incremental to TEI in predicting regional wall thickening recovery, especially in the CTO territory.
Global strain
Although strain significantly recovered at follow-up, we did not find a beneficial effect of CTO-PCI compared with no-CTO PCI on this recovery, which is consistent with the main EXPLORE trial results. FT-CMR strain has substantial clinical potential to be of diagnostic and prognostic value. Global strain measurements are highly reproducible with good to excellent intra- and inter-reproducibility and analysis appears not to be influenced by the level of training [7, 18]. However, only limited data is available on reference values of strain in healthy subjects. LVEF and LVEDV are frequently used in predicting patient prognosis; nonetheless, they are limited as contractility is not measured and they are affected by patient heart rate, loading conditions, and heart valve function [19]. We found that GLS is an independent predictor for global LV function, incremental to LVEF and LVEDV. In a beating heart, there are two longitudinal movements, shortening and lengthening (mainly reflecting GLS), and two transversal movements, narrowing and widening (mainly reflecting GCS). The cardiac cycle consists of different phases as described in more detail by Torrent-Guasp et al [20]. In short, (1) a decrease in the transversal diameter of the base caused by basal loop contraction (narrowing movement), (2) a decrease in the longitudinal axis (shortening movement), (3) an increase in the longitudinal axis (lengthening movement), and (4) an increase in the transversal diameter of the base are conditioned by the relaxation of the ventricular walls and widening movement [20]. GLS is mainly determined by subendocardial myofibers (the basal loop), which are more prone to early myocardial damage before global LV parameters are affected. Therefore, diminished GLS is an early marker of LV dysfunction. This could explain why GLS was the best predictor of LV preservation at follow-up. GCS is largely based on contraction of circumferential myofibers, which stay mostly preserved during early LV deterioration and serve as a restriction to prevent expansion of the LV [21].
For mortality, infarct size remained the strongest predictor. Previous reports regarding the prognostic value of global strain have been conflicting. In a study with 470 ischemic and non-ischemic cardiomyopathy patients, GLS was a strong predictor for mortality incremental to LVEF and infarct size [22]. In 74 STEMI patients, GCS was able to predict preservation of global function (LVEF > 50%) at follow-up similar to infarct size [23]. However, in a study of 65 STEMI patients, GLS was not able to predict adverse LV remodeling [5]. In another study, GLS did not improve risk stratification compared with baseline characteristics and CMR indices in 323 STEMI patients [24]. In the largest strain study thus far (1,235 MI patients), GLS did have incremental prognostic value over LVEF and infarct size to predict mortality [25]. Nonetheless, most studies performed are of small sample sizes and with relative short follow-up.
Segmental strain
Segmental strain significantly recovered at follow-up. Yet, there was no effect of CTO-PCI, compared with no-CTO PCI, on global nor on segmental strain recovery. However, we have previously shown that wall thickening significantly improves after CTO-PCI compared with no-CTO PCI in the dysfunctional CTO territory [11]. Although strain has the potential to detect more subtle regional differences, we could not reproduce this finding with segmental strain, although the number of segments was relatively low. Furthermore, it is important to mention that previous studies reported high degrees of measurement variability and relatively poor segmental strain reproducibility [26, 27]. Therefore, segmental strain data may be less reliable and its use in clinical practice should be done with caution.
We did find that segmental strain was a strong predictor for wall thickening recovery, incremental to infarct, especially in the dysfunctional CTO territory. This finding is consistent with previous data: in 45 STEMI patients, segmental strain was incremental to infarct and MVO in predicting recovery of wall thickening [28]. However, another study in STEMI patients showed that segmental strain was only a mild predictor of wall thickening recovery and inferior compared with infarct [29]. Furthermore, segmental strain and infarct transmurality are also related, as segmental strain is a predictor for infarcted segments [30]. Therefore, the incremental predictive value and exact relation of segmental strain and infarct needs further examination as, different from infarct (TEI), segmental strain can be measured without the use of a contrast agent, making it a possible alternative in patients with contrast allergy or renal failure.
Clinical use of myocardial strain assessment
In our high-risk patient population, new risk stratification parameters may be relevant to adequately select patients for CTO revascularization. None of the randomized CTO trails conducted showed a beneficial effect of CTO-PCI on clinical outcome nor on LVF, although ischemia and viability testing prior to inclusion were not mandated. It remains to be determined what the optimal patient selection threshold for CTO revascularization is and whether optimal selection will indeed lead to improved outcomes. Further studies are needed to investigate the true value of (stress) FT-CMR strain in clinical evaluation and whether it can be used as a diagnostic and prognostic tool to select patients that might benefit from PCI.
Limitations
There are several limitations applicable to this study. Unfortunately, not all CMRs were suitable for strain analysis and not all patients underwent baseline CMR. Furthermore, infarct data was not available in all patients and only 4% of the dysfunctional segments in the CTO territory were non-viable (TEI > 50%), making sample size relatively small and underpowered. Infarct size was probably decreased by the presence of collaterals, which were present in > 90% of the patients. As with all randomized trials, patient selection has occurred. The mortality rate was relatively low in our study cohort with the risk of overfitting the model and EXPLORE was not powered for clinical outcomes.
Conclusion
Global and segmental myocardial strains, measured by FT-CMR, improved significantly over time in STEMI patients with a concurrent CTO, with no beneficial effect of CTO-PCI. GLS was an independent predictor for functional recovery, incremental to infarct size, LVEF, and clinical parameters. Although GCS predicted mortality, infarct size remained the strongest predictor. Segmental circumferential strain was an independent predictor for regional LV recovery in the dysfunctional CTO territory.
Abbreviations
- CMR:
-
Cardiovascular magnetic resonance
- CTO:
-
Chronic total occlusion
- EXPLORE:
-
Evaluating Xience and left ventricular function in PCI on occlusiOns afteR STEMI
- FT:
-
Feature tracking
- GCS:
-
Global circumferential strain
- GLS:
-
Global longitudinal strain
- IRA:
-
Infarct-related artery
- LGE:
-
Late gadolinium-enhanced
- LVEDV:
-
Left ventricular end-diastolic volume
- LVEF:
-
Left ventricular ejection fraction
- MVO:
-
Microvascular obstruction
- PCI:
-
Percutaneous coronary intervention
- SSFP:
-
Steady-state free-precision
- STEMI:
-
ST-segment elevation myocardial infarction
- SWT:
-
Segmental wall thickening
- TEI:
-
Transmural extent of infarction
References
Bodi V, Sanchis J, Nunez J et al (2009) Prognostic value of a comprehensive cardiac magnetic resonance assessment soon after a first ST-segment elevation myocardial infarction. JACC Cardiovasc Imaging 2(7):835–842
Schuster A, Hor KN, Kowallick JT, Beerbaum P, Kutty S (2016) Cardiovascular magnetic resonance myocardial feature tracking: concepts and clinical applications. Circ Cardiovasc Imaging 9(4):e004077
Khan JN, Singh A, Nazir SA, Kanagala P, Gershlick AH, McCann GP (2015) Comparison of cardiovascular magnetic resonance feature tracking and tagging for the assessment of left ventricular systolic strain in acute myocardial infarction. Eur J Radiol 84(5):840–848
Hor KN, Gottliebson WM, Carson C et al (2010) Comparison of magnetic resonance feature tracking for strain calculation with harmonic phase imaging analysis. JACC Cardiovasc Imaging 3(2):144–151
Shetye AM, Nazir SA, Razvi NA et al (2017) Comparison of global myocardial strain assessed by cardiovascular magnetic resonance tagging and feature tracking to infarct size at predicting remodelling following STEMI. BMC Cardiovasc Disord 17(1):7
Gertz RJ, Lange T, Kowallick JT et al (2018) Inter-vendor reproducibility of left and right ventricular cardiovascular magnetic resonance myocardial feature-tracking. PLoS One 13(3):e0193746
Schmidt B, Dick A, Treutlein M et al (2017) Intra- and inter-observer reproducibility of global and regional magnetic resonance feature tracking derived strain parameters of the left and right ventricle. Eur J Radiol 89:97–105
Negishi T, Negishi K, Thavendiranathan P et al (2017) Effect of experience and training on the concordance and precision of strain measurements. JACC Cardiovasc Imaging 10(5):518–522
Yang ZK, Zhang RY, Hu J, Zhang Q, Ding FH, Shen WF (2013) Impact of successful staged revascularization of a chronic total occlusion in the non-infarct-related artery on long-term outcome in patients with acute ST-segment elevation myocardial infarction. Int J Cardiol 165(1):76–79
Henriques JP, Hoebers LP, Råmunddal T et al (2016) Percutaneous intervention for concurrent chronic total occlusions in patients with STEMI: the EXPLORE trial. J Am Coll Cardiol 68(15):1622–1632
Elias J, van Dongen IM, Hoebers LP et al (2017) Improved recovery of regional left ventricular function after PCI of chronic total occlusion in STEMI patients: a cardiovascular magnetic resonance study of the randomized controlled EXPLORE trial. J Cardiovasc Magn Reson 19(1):53
van der Schaaf RJ, Claessen BE, Hoebers LP et al (2010) Rationale and design of EXPLORE: a randomized, prospective, multicenter trial investigating the impact of recanalization of a chronic total occlusion on left ventricular function in patients after primary percutaneous coronary intervention for acute ST-elevation myocardial infarction. Trials 11:89
Bondarenko O, Beek AM, Hofman MB et al (2005) Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J Cardiovasc Magn Reson 7(2):481–485
Holman ER, Buller VG, de Roos A et al (1997) Detection and quantification of dysfunctional myocardium by magnetic resonance imaging. A new three-dimensional method for quantitative wall-thickening analysis. Circulation 95(4):924–931
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4):539–542
Elias J, van Dongen IM, Råmunddal T et al (2018) Long-term impact of chronic total occlusion recanalisation in patients with ST-elevation myocardial infarction. Heart 104(17):1432–1438
Nijveldt R, Beek AM, Hirsch A et al (2008) Functional recovery after acute myocardial infarction: comparison between angiography, electrocardiography, and cardiovascular magnetic resonance measures of microvascular injury. J Am Coll Cardiol 52(3):181–189
Morais P, Marchi A, Bogaert JA et al (2017) Cardiovascular magnetic resonance myocardial feature tracking using a non-rigid, elastic image registration algorithm: assessment of variability in a real-life clinical setting. J Cardiovasc Magn Reson 19(1):24
Gustafsson F, Torp-Pedersen C, Brendorp B et al (2003) Long-term survival in patients hospitalized with congestive heart failure: relation to preserved and reduced left ventricular systolic function. Eur Heart J 24(9):863–870
Torrent-Guasp F, Buckberg GD, Clemente C, Cox JL, Coghlan HC, Gharib M (2001) The structure and function of the helical heart and its buttress wrapping. I. The normal macroscopic structure of the heart. Semin Thorac Cardiovasc Surg 13(4):301–319
Hung CL, Verma A, Uno H et al (2010) Longitudinal and circumferential strain rate, left ventricular remodeling, and prognosis after myocardial infarction. J Am Coll Cardiol 56(22):1812–1822
Romano S, Judd RM, Kim RJ et al (2017) Association of feature-tracking cardiac magnetic resonance imaging left ventricular global longitudinal strain with all-cause mortality in patients with reduced left ventricular ejection fraction. Circulation 135(23):2313–2315
Buss SJ, Krautz B, Hofmann N et al (2015) Prediction of functional recovery by cardiac magnetic resonance feature tracking imaging in first time ST-elevation myocardial infarction. Comparison to infarct size and transmurality by late gadolinium enhancement. Int J Cardiol 183:162–170
Gavara J, Rodriguez-Palomares JF, Valente F et al (2017) Prognostic value of strain by tissue tracking cardiac magnetic resonance after ST-segment elevation myocardial infarction. JACC Cardiovasc Imaging 11:1448–1457
Eitel I, Stiermaier T, Lange T et al (2018) Cardiac magnetic resonance myocardial feature tracking for optimized prediction of cardiovascular events following myocardial infarction. JACC Cardiovasc Imaging 11:1433–1444
Wu L, Germans T, Güçlü A, Heymans MW, Allaart CP, van Rossum AC (2014) Feature tracking compared with tissue tagging measurements of segmental strain by cardiovascular magnetic resonance. J Cardiovasc Magn Reson 16:10
Morton G, Schuster A, Jogiya R, Kutty S, Beerbaum P, Nagel E (2012) Inter-study reproducibility of cardiovascular magnetic resonance myocardial feature tracking. J Cardiovasc Magn Reson 14:43
Wong DT, Leong DP, Weightman MJ et al (2014) Magnetic resonance-derived circumferential strain provides a superior and incremental assessment of improvement in contractile function in patients early after ST-segment elevation myocardial infarction. Eur Radiol 24(6):1219–1228
Khan JN, Nazir SA, Singh A et al (2016) Relationship of myocardial strain and markers of myocardial injury to predict segmental recovery after acute ST-segment-elevation myocardial infarction. Circ Cardiovasc Imaging 9(6)
Ogawa R, Kido T, Nakamura M et al (2017) Diagnostic capability of feature-tracking cardiovascular magnetic resonance to detect infarcted segments: a comparison with tagged magnetic resonance and wall thickening analysis. Clin Radiol 72(10):828–834
Acknowledgments
We acknowledge all the investigators and research coordinators who participated in the EXPLORE trial and thank all patients who participated in the trial. Trial Registration: trialregister.nl NTR1108, Date registered NTR: 30-okt-2007.
Funding
This study has received funding from the Academic Medical Centre in combination with a research grant from Abbott Vascular.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. J.P.S. Henriques.
Conflict of interest
JPSH has received grants from Abbott Vascular during the conduct of the study and has received grants from B. Braun, Abiomed, and Biotronik outside the submitted work. RJvdS has received grants from Abbott Vascular, Biotronik, and Biosensors, has received personal fees from Biotronik and Boston Scientific, has been a consultant for Biotronik, and has received speaker fees from OrbusNeich, Boston Scientific, and Asahi Intecc outside the submitted work. TR has been a proctor for Boston Scientific.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained. The EXPLORE trial was approved by the central Medical Ethics Review Committee (METC) of the Academic Medical Center of Amsterdam (The Netherlands) and by all local ethics committees involved.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in JACC (2016, main paper) and Heart (2018, long-term follow-up).
Methodology
• prospective
• randomized controlled trial
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Elias, J., van Dongen, I.M., Hoebers, L.P. et al. Recovery and prognostic value of myocardial strain in ST-segment elevation myocardial infarction patients with a concurrent chronic total occlusion. Eur Radiol 30, 600–608 (2020). https://doi.org/10.1007/s00330-019-06338-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06338-x