Abstract
Objective
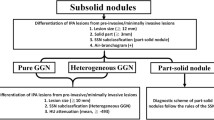
To validate three proposed definitions of the “solid” component of subsolid nodules, as compared to CT histograms and the use of different window settings, for discriminating the invasiveness of adenocarcinomas in a manner that facilitates routine clinical assessment.
Methods
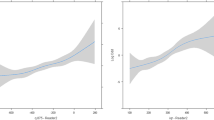
We retrospectively analyzed 328 pathologically confirmed lung adenocarcinomas, manifesting as subsolid nodules. Three-dimensional CT histograms were generated by setting 11 CT attenuation intervals from − 400 to 50 HU, at 50 HU intervals, and the voxel percentage within each CT attenuation interval was generated automatically. Three definitions of the “solid” component were proposed, and 10 medium window settings were set to evaluate the “solid” component. The diagnostic performance of the three definitions for identifying invasive adenocarcinoma was compared with that of CT histogram analysis and subjective evaluation with medium window settings.
Results
A parallel diagnosis using five intervals with the largest AUC (AUC ≥ 0.797) demonstrated good differential diagnostic performance, with 78% sensitivity and 73.7% specificity. Definition 2 (visibility in the mediastinum window) yielded higher accuracy (75.6%) than the other two definitions (p < 0.01). A medium window setting of − 50 WL/2 WW gave a larger AUC than the other nine medium window settings as well as definition 2, with 82.5% specificity and 88.5% PPV, which was higher than those of parallel diagnosis with CT histogram and definition 2.
Conclusion
Using − 50 WL/2 WW is the optimum approach for evaluating the “solid” component and discriminating invasiveness, superior to using 3D CT histograms and definition 2, and convenient in routine clinical assessment.
Key Points
• − 50 WL/2 WW gave a larger AUC than definition 2.
• The specificity of − 50 WL/2 WW was higher than CT histograms.
• − 50 WL/2 WW offers the best evaluation of the solid component.





Similar content being viewed by others
Abbreviations
- AAH:
-
Atypical adenomatous hyperplasia
- AIS:
-
Adenocarcinoma in situ
- AUC:
-
Area under the curve
- CT:
-
Computed tomography
- DFS:
-
Disease-free survival
- GGNs:
-
Ground-glass nodules
- IAC:
-
Invasive adenocarcinoma
- IASLC/ATS/ERS:
-
International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society
- LW:
-
Lung window
- MIA:
-
Minimally invasive adenocarcinoma
- MW:
-
Mediastinal window
- NPV:
-
Negative predictive value
- NSNs:
-
Nonsolid nodules
- NRI:
-
Net reclassification improvement
- OR:
-
Odds ratio
- PSNs:
-
Part-solid nodules
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
References
Goo JM, Park CM, Lee HJ (2011) Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol 196:533–543
Kim HY, Shim YM, Lee KS et al (2007) Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 245(1):267–275
Ding H, Shi J, Zhou X et al (2017) Value of CT characteristics in predicting invasiveness of adenocarcinoma presented as pulmonary ground-glass nodules. Thorac Cardiovasc Surg 65:136–141
Shikuma K, Menju T, Chen F et al (2016) Is volumetric 3-dimensional computed tomography useful to predict histological tumour invasiveness? Analysis of 211 lesions of cT1N0M0 lung adenocarcinoma. Interact Cardiovasc Thorac Surg 22:831–838
Yanagawa M, Johkoh T, Noguchi M et al (2017) Radiological prediction of tumor invasiveness of lung adenocarcinoma on thin-section CT. Medicine (Baltimore) 96:e6331
Travis WD, Brambilla E, Noguchi M et al (2011) International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6:244–285
Yanagawa N, Shiono S, Abiko M et al (2013) New IASLC/ATS/ERS classification and invasive tumor size are predictive of disease recurrence in stage I lung adenocarcinoma. J Thorac Oncol 8:612–618
Yoshiya T, Mimae T, Tsutani Y et al (2016) Prognostic role of subtype classification in small-sized pathologic N0 invasive lung adenocarcinoma. Ann Thorac Surg 102:1668–1673
Luo J, Huang Q, Wang R et al (2016) Prognostic and predictive value of the novel classification of lung adenocarcinoma in patients with stage IB. J Cancer Res Clin Oncol 142:2031–2040
Fan L, Fang M, Li Z et al (2018) Radiomics signature: a biomarker for the preoperative discrimination of lung invasive adenocarcinoma manifesting as a ground-glass nodule. Eur Radiol. https://doi.org/10.1007/s00330-018-5530-z
Naidich DP, Bankier AA, MacMahon H et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 266:304–317
Kakinuma R, Muramatsu Y, Kusumoto M et al (2015) Solitary pure ground-glass nodules 5 mm or smaller: frequency of growth. Radiology 276:873–882
Godoy MC, Naidich DP (2009) Subsolid pulmonary nodules and the spectrum of peripheral adenocarcinomas of the lung: recommended interim guidelines for assessment and management. Radiology 253:606–622
Kim H, Park CM, Woo S et al (2013) Pure and part-solid pulmonary ground-glass nodules: measurement variability of volume and mass in nodules with a solid portion less than or equal to 5 mm. Radiology 269:585–593
Bak SH, Lee HY, Kim JH et al (2016) Quantitative CT scanning analysis of pure ground-glass opacity nodules predict further CT scanning change. Chest 149:180–191
Fan L, Li Q, Xiao Y et al (2016) How to define and display solid components within ground-glass nodules and differentiate pure ground-glass nodules from mixed ground-glass nodules? Radiology 281:325–326
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Maeshima AM, Niki T, Maeshima A et al (2002) Modified scar grade: a prognostic indicator in small peripheral lung adenocarcinoma. Cancer 95:2546–2554
Peng M, Li Z, Hu H et al (2016) Pulmonary ground-glass nodules diagnosis: mean change rate of peak CT number as a discriminative factor of pathology during a follow-up. Br J Radiol 89:20150556
Li Q, Fan L, Cao ET et al (2017) Quantitative CT analysis of pulmonary pure ground-glass nodule predicts histological invasiveness. Eur J Radiol 89:67–71
Alpert JB, Rusinek H, Ko JP et al (2017) Lepidic predominant pulmonary lesions (LPL): CT-based distinction from more invasive adenocarcinomas using 3D volumetric density and first-order CT texture analysis. Acad Radiol 24:1604–1611
Yoshida Y, Sakamoto M, Maeda E et al (2015) Can image analysis on high-resolution computed tomography predict non-invasive growth in adenocarcinoma of the lung? Ann Thorac Cardiovasc Surg 21:8–13
Okada T, Iwano S, Ishigaki T et al (2009) Computer-aided diagnosis of lung cancer: definition and detection of ground-glass opacity type of nodules by high-resolution computed tomography. Jpn J Radiol 27:91–99
Cohen JG, Goo JM, Yoo RE et al (2016) Software performance in segmenting ground-glass and solid components of subsolid nodules in pulmonary adenocarcinomas. Eur Radiol 26:4465–4474
Kamiya S, Iwano S, Umakoshi H et al (2018) Computer-aided volumetry of part-solid lung cancers by using CT: solid component size predicts prognosis. Radiology 14:172319
Matsuguma H, Nakahara R, Anraku M et al (2004) Objective definition and measurement method of ground-glass opacity for planning limited resection in patients with clinical stage IA adenocarcinoma of the lung. Eur J Cardiothorac Surg 25:1102–1106
Matsunaga T, Suzuki K, Takamochi K et al (2017) What is the radiological definition of part-solid tumour in lung cancer? Eur J Cardiothorac Surg 51:242–247
Asamura H, Hishida T, Suzuki K et al (2013) Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg 146:24–30
Suzuki K, Koike T, Asakawa T et al (2011) A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol 6:751–756
Acknowledgements
We would like to thank the assistance of the United Imaging Healthcare Co. Ltd. for the pulmonary nodule advanced analysis tool software development and technical support.
Funding
This study has received funding from the National Key R&D Program of China (grant number 2016YFE0103000, 2017YFC1308703), the National Natural Science Foundation of China (grant number 81871321, 81370035), and the Youth Fund of the National Natural Science Foundation of China (grant number 81501618, 81501470).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Li FAN.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Prof. Jian Lu (Department of Statistics, Second Military Medical University) kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
An Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Electronic supplementary material
ESM 1
(DOCX 112 kb)
Rights and permissions
About this article
Cite this article
Tu, W., Li, Z., Wang, Y. et al. The “solid” component within subsolid nodules: imaging definition, display, and correlation with invasiveness of lung adenocarcinoma, a comparison of CT histograms and subjective evaluation. Eur Radiol 29, 1703–1713 (2019). https://doi.org/10.1007/s00330-018-5778-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5778-3