Abstract
Objectives
To identify the radiomics signature allowing preoperative discrimination of lung invasive adenocarcinomas from non-invasive lesions manifesting as ground-glass nodules.
Methods
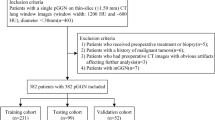
This retrospective primary cohort study included 160 pathologically confirmed lung adenocarcinomas. Radiomics features were extracted from preoperative non-contrast CT images to build a radiomics signature. The predictive performance and calibration of the radiomics signature were evaluated using intra-cross (n=76), external non-contrast-enhanced CT (n=75) and contrast-enhanced CT (n=84) validation cohorts. The performance of radiomics signature and CT morphological and quantitative indices were compared.
Results
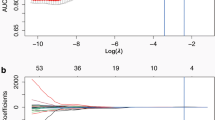
355 three-dimensional radiomics features were extracted, and two features were identified as the best discriminators to build a radiomics signature. The radiomics signature showed a good ability to discriminate between invasive adenocarcinomas and non-invasive lesions with an accuracy of 86.3%, 90.8%, 84.0% and 88.1%, respectively, in the primary and validation cohorts. It remained an independent predictor after adjusting for traditional preoperative factors (odds ratio 1.87, p < 0.001) and demonstrated good calibration in all cohorts. It was a better independent predictor than CT morphology or mean CT value.
Conclusions
The radiomics signature showed good predictive performance in discriminating between invasive adenocarcinomas and non-invasive lesions. Being a non-invasive biomarker, it could assist in determining therapeutic strategies for lung adenocarcinoma.
Key Points
• The radiomics signature was a non-invasive biomarker of lung invasive adenocarcinoma.
• The radiomics signature outweighed CT morphological and quantitative indices.
• A three-centre study showed that radiomics signature had good predictive performance.



Similar content being viewed by others
Abbreviations
- ANNs:
-
Artificial neural networks
- AUC:
-
Area under the curve
- CT:
-
Computed tomography
- DFS:
-
Disease-free survival
- GGN:
-
Ground-glass nodule
- GLCM:
-
Grey-level co-occurrence matrix
- GLRLM:
-
Grey-level run-length matrix
- IAC:
-
Invasive adenocarcinoma
- IASLC/ATS/ERS:
-
International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society
- LASSO:
-
The least absolute shrinkage and selection operator
- MIA:
-
Minimally invasive adenocarcinoma
- ROC:
-
Receiver-operating characteristic
References
Goo JM, Park CM, Lee HJ (2011) Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol 196:533–543
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics. CA Cancer J Clin 63:11–30
de Groot P, Munden RF (2012) Lung cancer epidemiology, risk factors, and prevention. Radiol Clin North Am 50:863–876
Travis WD, Brambilla E, Noguchi M et al (2011) International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6:244–285
Russell PA, Wainer Z, Wright GM et al (2011) Does lung adenocarcinoma subtype predict patient survival? A clinicopathologic study based on the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary lung adenocarcinoma classification. J Thorac Oncol 6:1496–1504
Luo J, Huang Q, Wang R et al (2016) Prognostic and predictive value of the novel classification of lung adenocarcinoma in patients with stage IB. J Cancer Res Clin Oncol 142:2031–2040
Yanagawa N, Shiono S, Abiko M et al (2013) New IASLC/ATS/ERS classification and invasive tumor size are predictive of disease recurrence in stage I lung adenocarcinoma. J Thorac Oncol 8:612–618
Yoshiya T, Mimae T, Tsutani Y et al (2016) Prognostic role of subtype classification in small-sized pathologic N0 invasive lung adenocarcinoma. Ann Thorac Surg 102:1668–1673
Yoshizawa A, Motoi N, Riely GJ et al (2011) Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 24:653–664
Lee HY, Choi YL, Lee KS et al (2014) Pure ground-glass opacity neoplastic lung nodules: histopathology, imaging, and management. AJR Am J Roentgenol 202:W224–W233
Ding H, Shi J, Zhou X et al (2017) Value of CT characteristics in predicting invasiveness of adenocarcinoma presented as pulmonary ground-glass nodules. Thorac Cardiovasc Surg 65:136–141
Fan L, Liu SY, Li QC et al (2012) Multidetector CT features of pulmonary focal ground-glass opacity: differences between benign and malignant. Br J Radiol 85:897–904
Zhang Y, Qiang JW, Shen Y et al (2016) Using air bronchograms on multi-detector CT to predict the invasiveness of small lung adenocarcinoma. Eur J Radiol 85:571–577
Shikuma K, Menju T, Chen F et al (2016) Is volumetric 3-dimensional computed tomography useful to predict histological tumour invasiveness? Analysis of 211 lesions of cT1N0M0 lung adenocarcinoma. Interact Cardiovasc Thorac Surg 22:831–838
Ikeda K, Awai K, Mori T et al (2007) Differential diagnosis of ground-glass opacity nodules: CT number analysis by three-dimensional computerized quantification. Chest 132:984–990
Yu WS, Hong SR, Lee JG et al (2016) Three-dimensional ground glass opacity ratio in C T images can predict tumor invasiveness of stage Ia lung cancer. Yonsei Med J 57:1131–1138
Aerts HJ, Velazquez ER, Leijenaar RT et al (2014) Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 5:4006
Parmar C, Leijenaar RT, Grossmann P et al (2015) Radiomic feature clusters and prognostic signatures specific for lung and head and neck cancer. Sci Rep 5:11044
Huang YQ, Liang CH, He L et al (2016) Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol 34:2157–2164
Sakakura N, Inaba Y, Yatabe Y et al (2016) Estimation of the pathological invasive size of pulmonary adenocarcinoma using high-resolution computed tomography of the chest: a consideration based on lung and mediastinal window settings. Lung Cancer 95:51–56
Son JY, Lee HY, Kim JH et al (2016) Quantitative CT analysis of pulmonary ground-glass opacity nodules for distinguishing invasive adenocarcinoma from non–invasive or minimally invasive adenocarcinoma: the added value of using iodine mapping. Eur Radiol 26:43–54
Kitami A, Sano F, Hayashi S et al (2016) Correlation between histological invasiveness and the computed tomography value in pure ground-glass nodules. Surg Today 46:593–598
Lim HJ, Ahn S, Lee KS et al (2013) Persistent pure ground glass opacity lung nodules ≥10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 144:1291–1299
Nomori H, Ohtsuka T, Naruke T et al (2003) Differentiating between atypical adenomatous hyperplasia and bronchioloalveolar carcinoma using the computed tomography number histogram. Ann Thorac Surg 76:867–871
Kumar V, Gu Y, Basu S et al (2012) Radiomics: the process and the challenges. Magn Reson Imaging 30:1234–1248
Zhao B, Tan Y, Tsai WY et al (2016) Reproducibility of radiomics for deciphering tumor phenotype with imaging. Sci Rep 6:23428
Coroller TP, Grossmann P, Hou Y et al (2015) CT-based radiomic signature predicts distant metastasis in lung adenocarcinoma. Radiother Oncol 114:345–350
Chae HD, Park CM, Park SJ et al (2014) Computerized texture analysis of persistent part-solid ground-glass nodules: differentiation of preinvasive lesions from invasive pulmonary adenocarcinomas. Radiology 273:285–293
Song J, Yang C, Fan L et al (2016) Lung lesion extraction using a toboggan based growing automatic segmentation approach. IEEE Trans Med Imaging 35:337–353
Wang S, Zhou M, Liu Z et al (2017) Central focused convolutional neural networks: Developing a data-driven model for lung nodule segmentation. Med Image Anal 40:172–183
Funding
This study has received funding by the National Natural Science Foundation of China (grant numbers 81370035, 81230030, and 81771924), The National Key R&D Program of China (grant number 2016YFE0103000, 2017YFC1308703, 2017YFA0205200, 2017YFC1309100 and 2017YFC1308700), Shanghai Pujiang Talent Program (grant number 15PJD002).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Shiyuan Liu.
Conflict of interest
The authors of this article declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• multicentre study
Electronic supplementary material
ESM 1
(DOCX 356 kb)
Rights and permissions
About this article
Cite this article
Fan, L., Fang, M., Li, Z. et al. Radiomics signature: a biomarker for the preoperative discrimination of lung invasive adenocarcinoma manifesting as a ground-glass nodule. Eur Radiol 29, 889–897 (2019). https://doi.org/10.1007/s00330-018-5530-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5530-z