Abstract
Objectives
To assess whether initial or 12–18-month change in magnetic resonance imaging (MRI) subchondral bone texture is predictive of radiographic knee osteoarthritis (OA) progression over 36 months.
Methods
This was a nested case-control study including 122 knees/122 participants in the Osteoarthritis Initiative (OAI) Bone Ancillary Study, who underwent MRI optimised for subchondral bone assessment at either the 30- or 36-month and 48-month OAI visits. Case knees (n = 61) had radiographic OA progression between the 36- and 72-month OAI visits, defined as ≥ 0.7 mm minimum medial tibiofemoral radiographic joint space (minJSW) loss. Control knees (n = 61) without radiographic OA progression were matched (1:1) to cases for age, sex, body mass index and initial medial minJSW. Texture analysis was performed on the medial femoral and tibial subchondral bone. We assessed the association of texture features with radiographic progression by creating a composite texture score using penalised logistic regression and calculating odds ratios. We evaluated the predictive performance of texture features for predicting radiographic progression using c-statistics.
Results
Initial (odds ratio [95% confidence interval] = 2.13 [1.41–3.40]) and 12– 18-month change (3.76 [2.04–7.82]) texture scores were significantly associated with radiographic OA progression. Combinations of texture features were significant predictors of radiographic progression using initial (c-statistic [95% confidence interval] = 0.65 [0.64–0.65], p = 0.003) and 12–18-month change (0.68 [0.68-0.68], p < 0.001) data.
Conclusions
Initial and 12–18-month changes in MRI subchondral bone texture score were significantly associated with radiographic progression at 36 months, with better predictive performance for 12–18-month change in texture. These results suggest that texture analysis may be a useful biomarker of subchondral bone in OA.
Key Points
• Subchondral bone MRI texture analysis is a promising knee osteoarthritis imaging biomarker.
• In this study, subchondral bone texture was associated with knee osteoarthritis progression.
• This demonstrates predictive and concurrent validity of MRI subchondral bone texture analysis.
• This method may be useful in clinical trials with interventions targeting bone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is increasingly recognised that subchondral bone plays a critical role in osteoarthritis (OA) onset and progression. Subchondral bone is a dynamic tissue, absorbing the majority of forces transmitted through the joint and capable of remodelling in response to stress [1]. Therefore, there has been increasing interest in subchondral bone as a target for potential disease-modifying OA drugs (DMOADs) [2].
Sensitive markers of subchondral bone alterations that occur in OA are required for such treatments to be evaluated. Several imaging biomarkers of subchondral bone have been described using plain radiographs, dual x-ray absorptiometry (DXA), computed tomography (CT) and magnetic resonance imaging (MRI), including direct estimation of trabecular microarchitecture and fractal signature analysis (FSA) [3, 4]. While several established biomarkers have shown cross-sectional associations with OA severity, there remains room for improvement with regard to the ability to predict OA progression [5,6,7,8].
MRI texture analysis (MRI TA) has recently been described as a method of quantifying subchondral bone changes in OA which may offer superiority over existing biomarkers [9]. MRI TA involves the calculation of several statistical descriptors of image texture, aiming to characterise the heterogeneity and spatial-organisation of the subchondral bone. The technique has been shown to be reproducible and able to distinguish subjects at different stages of OA from healthy subjects [9]. Moreover, texture features have shown an improved ability to discriminate between knees with and without OA when compared to microarchitectural analysis and are significantly associated with histomorphometry [10, 11].
However, MRI TA has previously only been used to compare subjects with OA and healthy controls. To be useful as a prognostic or treatment evaluation imaging biomarker, it should also be able to identify which individuals with OA are likely to progress (predictive validity) and demonstrate sensitivity to change for OA progression (concurrent validity).
Therefore, the purpose of this study was to evaluate whether (1) initial (i.e. OAI visit at 30 or 36 months) or (2) 12–18-month change (i.e. between OAI visit at 30/36 months and 48 months) in MRI subchondral bone texture were predictive of radiographic OA progression over 36 months (i.e. between OAI visit at 36 months and 72 months).
Methods
The Osteoarthritis Initiative (OAI) has been approved by the Institutional Review Boards of the University of California, San Francisco and the four OAI clinical centers (University of Pittsburgh, Ohio State University, University of Maryland, Baltimore, and Memorial Hospital of Rhode Island). All participants have given informed consent to participate in the study. This was a retrospective nested case-control study. The OAI datasets are freely available for download at https://oai.epi-ucsf.org.
Subjects
Included participants were participants in the OAI Bone Ancillary Study (BAS). The BAS featured 629 participants who underwent MRI examination optimised for assessment of subchondral bone in addition to the standard OAI MRI. All BAS participants were members of the progression sub-cohort, participants with both frequent knee symptoms and radiographic OA in at least one knee at OAI inception. Initial trabecular bone MRIs were performed at either the 30- or 36-month OAI visit, with the majority of participants undergoing a repeat MRI at the 48-month OAI visit (“12–18-month follow-up”). The study design is summarised in Fig. 1.
We defined study cases (“progressors”) as individuals with radiographic progression over a 36-month period between the 36-month OAI visit and the 72-month OAI visit, according to the definition of the Foundation for the National Institutes of Health (FNIH) OA biomarkers consortium: a decrease in minimum medial tibiofemoral joint space width (minJSW) of ≥ 0.7 mm, which has a less than 10% chance of being due to measurement error [12]. The details of the radiographic acquisition and assessments have been discussed in detail previously. Briefly, knee radiographs were performed using a non-fluoroscopic fixed flexion technique [13]. Assessments included central readings for Kellgren-Lawrence (KL) grading, Osteoarthritis Research Society International (OARSI) grading of joint space narrowing (JSN), measurement of femorotibial alignment and automated measurement of joint space width [14,15,16].
Progressors were matched to participants who did not have radiographic progression between the 36-month OAI visit and 72-month OAI visit (controls) for age, sex, body mass index (BMI) and initial medial minJSW in a 1:1 ratio, using an optimal nearest-neighbour propensity score algorithm.
We excluded individuals who did not have measurements of minJSW available at the 36-month or 72-month OAI visits and individuals with KL grade-4 knees at the 36-month visit (due to ceiling effects on minJSW progression in this group). As this study focused on the medial tibiofemoral compartment, we excluded any individuals who had lateral compartment predominant disease at the 36-month OAI visit, as defined by greater OARSI JSN grade in the lateral than medial compartment.
MRI acquisition
Study participants were evaluated with a coronal-oblique three-dimensional fast imaging with steady-state precession (FISP) MRI sequence (field of view 12 x 12 cm, matrix 512 x 512 [interpolated to 1024 x 1024], slice thickness 1 mm, repetition time 20 ms, echo time 4.92 ms, flip angle 50o, number of signal averages 1, acquisition time 10.5 minutes) optimised for visualisation of subchondral trabecular bone [17]. This was performed on one of four identical Siemens Trio 3T MR platforms used for the OAI using a quadrature transmit-receive knee coil (USA Instruments).
MRI analysis
The five most central coronal-oblique images through the central medial tibiofemoral joint were identified with reference to axial and sagittal reformats and used for subsequent analysis.
The MRI images were imported into a dedicated texture analysis program (MazDA v3.3, freely available at http://www.eletel.p.lodz.pl/programy/mazda/) [18]. Regions of interest (ROIs) were created manually in the medial tibial and medial femoral subchondral bone on each coronal image by an analyst blinded to case or control status of participants (JM, a musculoskeletal radiologist with 5 years’ experience). ROIs were defined superiorly and inferiorly by the bone–cartilage interface, medially and laterally by the margins of the tibial plateau and femoral condyle and extended for a depth of approximately 1 cm into the subchondral bone. Illustrative ROI examples are provided in Fig. 2.
Nineteen texture features were calculated for each ROI aiming to quantify the heterogeneity and spatial organisation of the subchondral bone, according to the method described previously [9]. These texture features belonged to one of four classes: grey-level histogram, absolute gradient, run-length matrix (RLM) and grey-level co-occurrence matrix (GLCM). Briefly, grey-level histogram features are simple descriptors of the distribution of grey levels (i.e. pixel intensity values) in the ROI. Gradient, RLM and GLCM features are higher-order descriptors of the spatial organisation of pixels in the ROI. We used image compression settings of four bits/pixel for calculation of gradient features, and six bits/pixel for calculation of GLCM and RLM parameters. RLM parameters were calculated four times for each pixel (in the horizontal, vertical, 45o and 135o directions) and GLCM parameters were calculated 20 times for each pixel at a variety of pixel offsets ranging from 1 to 5 pixels. The mean value of each RLM and GLCM parameter for each pixel in all possible directions and pixel offsets was calculated for each coronal image. The values of each texture parameter on each of the five coronal images analysed were then averaged to give summary values in each participant for medial tibial and medial femoral ROIs.
Texture analysis reproducibility
Twenty-three randomly selected participants were analysed in duplicate by two independent analysts (JM & GK: both musculoskeletal radiologists with 5 years’ experience) to assess reproducibility. Analysts created ROIs independently and were blinded to case or control status. The sample size was based on previous data, suggesting a mean intraclass correlation coefficient (ICC) value of 0.9 across texture features [10, 19]. Texture features with suboptimal reproducibility metrics (ICCs of < 0.8 or root-mean-square average coefficient of variation [RMSCV] of > 10% for either ROI) were excluded from subsequent analyses.
Statistical analysis
Descriptive statistics for each texture feature were generated. We compared the distribution of texture values in progressors and controls visually using boxplots. We created composite texture scores using linear combinations of texture features with least absolute shrinkage and selection operator (LASSO) penalised logistic regression. This helps to avoid problems associated with overfitting when many predictor variables are available by imposing a penalty for including additional variables in a model. The LASSO model was chosen based on minimisation of 10-fold cross-validation classification error. Because the folds for cross-validation are chosen at random, the procedure was repeated with 100 iterations. We used the logistic regression equation from the model iteration giving the mean classification error to calculate a composite texture score. This was performed separately for tibial, femoral and combined (tibial and femoral) texture datasets using initial MRI texture features and 12–18-month change in MRI texture features.
Odds ratios were calculated for the increase or decrease in odds of radiographic progression per one standard deviation (SD) increase in texture score. The mean classification accuracy (c-statistic, equivalent to area under the receiver operating curve [AUC]) was recorded.
Inter-observer reproducibility was assessed using ICC values (single measures, absolute agreement) and the RMSCV for each texture feature.
All statistical analyses were performed using RStudio version 1.0.136 for Mac, using the MatchIt package for matching cases to controls, and the glmnet package for performing LASSO regression [20, 21]. Statistical significance of the logistic regression analyses was assessed using the chi-squared test, with an adjusted p value threshold of < 0.008 to maintain an overall type 1 error rate of 0.05.
Results
Participants
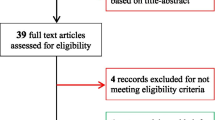
Of 629 participants in the BAS, 359 were eligible for this study following exclusions. Sixty-four participants met the criterion for radiographic progression and were selected as cases, with 64 controls matched for age, sex, BMI and initial minJSW.
For initial timepoint analyses, 12 participants (3 cases) were excluded due to excessive motion artefacts, defined as preventing the identification of the bone–cartilage interface (n = 5), unavailable initial MRI (n = 3) or large subchondral cysts preventing ROI placement in trabecular bone (n = 4). The matched controls for excluded cases were also removed from the analysis. For each excluded control, a new matched control was selected as the next best match for the corresponding case according to the matching algorithm.
For 12–18-month follow-up analyses, a further 17 participants were excluded due to excessive motion artefacts on follow-up images (n = 8), unavailable follow-up MRI (n = 8), and surgical intervention during the interval between initial and follow-up MRI (n = 1).
Initial and follow-up characteristics of included cases and controls are presented in Table 1. A flow diagram for selection of study participants is presented in Fig. 3.
Texture analysis reproducibility
Data for inter-observer reproducibility are presented in the supplementary material. The majority of texture features demonstrated excellent inter-observer reproducibility. Seven texture features were excluded from subsequent analyses at this stage (per criteria in Methods), leaving a total of 12 texture features for analysis.
Association of subchondral bone texture and radiographic progression
Subchondral bone composite texture score was significantly associated with 36-month radiographic progression using the initial timepoint combined data (odds ratio [95% confidence interval] = 1.84 [1.25 – 2.80], p = 0.002) and the 12–18-month change tibial (2.31 [1.42 – 4.12], p < 0.001), femoral (1.80 [1.17 – 2.92], p = 0.006) and combined (3.76 [2.04 – 7.82], p < 0.001) data. Associations between subchondral bone texture score and radiographic progression using initial timepoint tibial (1.43 [0.99 – 2.09], p = 0.06) and femoral (1.63 [1.12 – 2.44], p = 0.009) data were not statistically significant. Results are summarised in Table 2. Data for each individual texture feature are provided in the supplementary material. Example images are shown in Fig. 4.
Example coronal 3D FISP MR images through the medial tibiofemoral compartment of radiographic progressors and non-progressors at the initial timepoint. A, non-progressor, texture score (TS) –1.22, B, non-progressor, TS –1.44, C, progressor, TS +1.01, and D, progressor, TS +0.93. Higher texture scores correspond to less spatially organised subchondral bone
Texture analysis classification
Combinations of both initial texture features and 12–18-month change in texture features were able to predict radiographic progression with statistical significance reached for femoral and combined initial data, and tibial, femoral and combined 12–18-month change data. The best classification accuracy was demonstrated for combined 12–18-month follow-up data with a c-statistic of 0.68 (95% confidence interval 0.68 – 0.68, p < 0.001).
Classification performance is summarised in Table 2.
Discussion
This study demonstrates that combinations of initial and 12–18-month change in subchondral bone MR texture features are significantly associated with radiographic OA progression over 36 months, with better predictive ability for 12–18-month change data.
These results suggest that subchondral bone texture may be a useful quantitative imaging biomarker for use in clinical trials, particularly those with interventions targeting subchondral bone. Although direct interpretation of the texture scores used in this study is difficult, results are consistent with progressors having less spatially organised, more homogeneous subchondral bone at the initial timepoint, and 12–18-month changes in the same direction. This is supported by visual assessment of example images. Combinations of texture features were able to predict case and control status using both initial and 12–18-month change in texture features. Classification accuracy improved when tibial and femoral data were combined. However, the best-performing model had only modest predictive ability (AUC 0.68), despite the strong associations between texture score and radiographic progression.
Possible explanations for the limited performance of MR subchondral bone texture in this study include a bias towards advanced OA in our cohort, and the MRI sequence used. First, as members of the progression sub-cohort of the OAI, most participants had established OA. Our study sample was further biased towards more advanced disease by the fact that only individuals with established OA at the 48-month OAI visit had quantitative JSW measurements performed at the 72-month OAI visit. MR subchondral bone texture has previously demonstrated the ability to detect relatively early OA-related changes in the subchondral bone; therefore, it may be that it is of less use in more established disease. Second, the MRI sequence used as part of the OAI BAS was optimised for analysing trabecular microarchitecture (i.e. direct estimation of histomorphometry parameters). While texture analysis has previously been described using a similar MRI sequence, it has also been demonstrated that alternative MRI sequences may provide improved texture discrimination between groups [22].
Nevertheless, the strength of association between texture scores and radiographic progression and the AUC values presented here are competitive when compared to several alternative OA imaging biomarkers, especially considering the relatively short follow-up time and matching of the control cohort in this study for important predictive covariates of age, sex and BMI [5, 23,24,25,26]. For example, in the FNIH OA biomarkers consortium studies, central medial tibiofemoral compartment cartilage loss over 24 months was associated with radiographic progression at 24–28 months with a similar odds ratio (3.8 [95% CI 2.7 to 5.5]) to that for 12–18-month change in combined texture score (3.8 [2.0 – 7.8]) in this study [25]. In the same FNIH cohort, associations between femoral bone shape change (odds ratio 2.7 [2.0 to 3.6]) and femoral bone area change (2.9 [2.1 to 3.9]) over 24 months and radiographic progression at 24-48 months were also of a similar magnitude to those described here [26]. Associations between fractal signature analysis (FSA) parameters obtained from plain radiographs and radiographic progression in the FNIH OA biomarkers cohort were weaker than those described in this study, as was the predictive ability of FSA [5].
Our results demonstrate that MRI TA of subchondral bone can be considered a useful addition to the suite of imaging biomarkers available for further OA imaging research studies. One advantage over alternative techniques is the multidimensional data output of texture analysis, which is well-placed to interact with machine-learning-based approaches to image interpretation. Indeed, the LASSO method employed here is an example of such an approach.
One disadvantage of MRI TA is that it is not always clear what the biological or structural correlates of individual texture features are, despite previous demonstration of association with histomorphometry [11]. However, as has been shown by the use of texture analysis in imaging applications other than assessment of subchondral bone, this lack of correspondence to an underlying structural ‘ground-truth’ does not preclude the use of this method to improve our understanding of the underlying disease process [27,28,29]. In the present study, MRI TA has usefully quantified the degree of ‘abnormality’ in the appearance of the subchondral bone despite limited structural correlation of the texture parameters used.
Future work could evaluate MRI TA of subchondral bone in alternative populations, and a head-to-head comparison of different methods for analysing subchondral bone would help to determine the optimal imaging biomarker for use in clinical trials. A barrier to performing this comparison in the present study was the fact that the platforms used for several alternative methods are not freely available, in contrast to the method used here. Automation of the time-consuming ROI-drawing procedure would also encourage wider use of this method.
There are several limitations to the present study. Structural correlates for texture parameters have been assessed in previous studies, but using a different MRI sequence. Nevertheless, a comparison of texture features between sequences has shown similar changes in both, so it is reasonable to assume similar structural correlates for the texture features derived from the MRI sequence used in this study [22]. We used a retrospective case-control design which is subject to selection bias. However, our matching process ensured that cases and controls were well-matched for important baseline characteristics. In common with other longitudinal studies using the OAI dataset, it is not possible to completely separate concurrent from predictive validity for MR subchondral bone texture as the period of follow-up for change in MR texture features overlapped with the follow-up period for radiographic progression. We had a small sample size for the number of texture features analyzed which risks introducing bias into any classification procedure. We have aimed to minimise this by excluding texture features with poor reproducibility, using cross-validation, and using penalised regression to limit the number of texture features incorporated into our classification models. Finally, we defined OA progression based on change in radiographic joint space width. This measure is established and robust but captures only one aspect of OA progression. Symptomatic progression is also important, but not considered in this study due to the low numbers of symptomatic progressors in our cohort.
In conclusion, initial and 12–18-month change in combinations of MR subchondral bone texture features were associated with 36-month radiographic OA progression, with better predictive performance of 12–18-month change data.
Abbreviations
- BAS:
-
Bone Ancillary Study
- OAI:
-
Osteoarthritis Initiative
- minJSW:
-
Minimum (medial tibiofemoral) joint space width
- MRI TA:
-
Magnetic resonance imaging texture analysis
References
Goldring MB, Goldring SR (2010) Articular cartilage and subchondral bone in the pathogenesis of osteoarthritis. Ann N Y Acad Sci 1192:230–237
Kwan Tat S, Lajeunesse D, Pelletier J-P, Martel-Pelletier J (2010) Targeting subchondral bone for treating osteoarthritis: what is the evidence? Best Pract Res Clin Rheumatol 24:51–70
Chang G, Xia D, Chen C et al (2015) 7T MRI detects deterioration in subchondral bone microarchitecture in subjects with mild knee osteoarthritis as compared with healthy controls. J Magn Reson Imaging 41:1311–1317
Kraus VB, Feng S, Wang S et al (2013) Subchondral Bone Trabecular Integrity Predicts and Changes Concurrently with Radiographic and Magnetic Resonance Imaging-Determined Knee Osteoarthritis Progression. Arthritis Rheum 65:1812–1821
Kraus VB, Collins JE, Charles HC et al (2017) Predictive validity of radiographic trabecular bone texture in knee OA - The OARSI / FNIH OA biomarkers consortium. Arthritis Rheum. https://doi.org/10.1002/art.40348
Lo GH, Schneider E, Driban JB et al (2018) Periarticular Bone Predicts Knee Osteoarthritis Progression: Data from the Osteoarthritis Initiative. Semin Arthritis Rheum. https://doi.org/10.1016/j.semarthrit.2018.01.008
Lo GH, Tassinari AM, Driban JB et al (2012) Cross-sectional DXA and MR measures of tibial periarticular bone associate with radiographic knee osteoarthritis severity. Osteoarthritis Cartilage 20:686–693
Hirvasniemi J, Thevenot J, Guermazi A et al (2017) Differences in tibial subchondral bone structure evaluated using plain radiographs between knees with and without cartilage damage or bone marrow lesions - the Oulu Knee Osteoarthritis study. Eur Radiol 27:4874–4882
MacKay JW, Murray PJ, Kasmai B et al (2016) MRI texture analysis of subchondral bone at the tibial plateau. Eur Radiol 26:3034–3045
MacKay JW, Murray PJ, Low SBL et al (2016) Quantitative analysis of tibial subchondral bone: Texture analysis outperforms conventional trabecular microarchitecture analysis. J Magn Reson Imaging 43:1159–1170
MacKay JW, Murray PJ, Kasmai B et al (2017) Subchondral bone in osteoarthritis: association between MRI texture analysis and histomorphometry. Osteoarthritis Cartilage 25:700–707
Hunter DJ, Nevitt M, Losina E, Kraus V (2014) Biomarkers for osteoarthritis: Current position and steps towards further validation. Best Pract Res Clin Rheumatol 28:61–71
Nevitt MC, Peterfy C, Guermazi A et al (2007) Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum 56:1512–1520
Duryea J, Neumann G, Niu J et al (2010) Comparison of radiographic joint space width with magnetic resonance imaging cartilage morphometry: analysis of longitudinal data from the Osteoarthritis Initiative. Arthritis Care Res 62:932–937
Felson DT, Nevitt MC, Yang M et al (2008) A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol 35:2047–2054
Iranpour-Boroujeni T, Li J, Lynch JA et al (2014) A new method to measure anatomic knee alignment for large studies of OA: data from the osteoarthritis initiative. Osteoarthritis Cartilage 22:1668–1674
Schneider E, Lo GH, Sloane G et al (2011) Magnetic resonance imaging evaluation of weight-bearing subchondral trabecular bone in the knee. Skeletal Radiol 40:95–103
Szczypiński PM, Strzelecki M, Materka A, Klepaczko A (2009) MaZda--a software package for image texture analysis. Comput Methods Prog Biomed 94:66–76
Zou GY (2012) Sample size formulas for estimating intraclass correlation coefficients with precision and assurance. Stat Med 31:3972–3981
Ho D, Imai K, King G, Stuart EA (2011) MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. J Stat Softw 42:1–28
Friedman J, Hastie T, Tibshirani R (2010) Regularization Paths for Generalized Linear Models via Coordinate Descent. J Stat Softw 33:1–22
MacKay JW, Low SBL, Murray PJ, et al (2016) MR texture analysis of subchondral bone in osteoarthritis. In: Proc Intl Soc Mag Reson Med 25. Singapore, p 4485.Available via http://dev.ismrm.org/2016/4485.html. Accessed 29 Jan 2018
Collins JE, Losina E, Nevitt MC et al (2016) Semiquantitative Imaging Biomarkers of Knee Osteoarthritis Progression: Data From the Foundation for the National Institutes of Health Osteoarthritis Biomarkers Consortium. Arthritis Rheum 68:2422–2431
LaValley MP, Lo GH, Price LL et al (2017) Development of a clinical prediction algorithm for knee osteoarthritis structural progression in a cohort study: value of adding measurement of subchondral bone density. Arthritis Res Ther 19:95. https://doi.org/10.1186/s13075-017-1291-3
Eckstein F, Collins JE, Nevitt MC et al (2015) Brief Report: Cartilage Thickness Change as an Imaging Biomarker of Knee Osteoarthritis Progression: Data from the Foundation for the National Institutes of Health Osteoarthritis Biomarkers Consortium. Arthritis Rheum 67:3184–3189
Hunter D, Nevitt M, Lynch J et al (2016) Longitudinal validation of periarticular bone area and 3D shape as biomarkers for knee OA progression? Data from the FNIH OA Biomarkers Consortium. Ann Rheum Dis 75:1607–1614
Hodgdon T, McInnes MDF, Schieda N et al (2015) Can Quantitative CT Texture Analysis be Used to Differentiate Fat-poor Renal Angiomyolipoma from Renal Cell Carcinoma on Unenhanced CT Images? Radiology 276:787–796
Ng F, Ganeshan B, Kozarski R et al (2013) Assessment of Primary Colorectal Cancer Heterogeneity by Using Whole-Tumor Texture Analysis: Contrast-enhanced CT Texture as a Biomarker of 5-year Survival. Radiology 266:177–184
Rajani NK, Joshi NV, Elkhawad M et al (2014) CT textural analysis of abdominal aortic aneurysms as a biomarker for aneurysm growth. Lancet 383:S87
Acknowledgements
The Role of Bone in Knee Osteoarthritis Progression is supported by NIH/NIAMS (grant R01 AR054938). The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services and conducted by the OAI Study Investigators. Private funding partners include Pfizer, Inc.; Novartis Pharmaceuticals Corporation; Merck Research Laboratories; and GlaxoSmithKline. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript has received the approval of the OAI Publications Committee based on a review of its scientific content and data interpretation. This work was supported in part by the Houston VA HSR&D Center of Excellence (HFP90-020). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
JM is supported by an Addenbrooke’s Charitable Trust Clinical Research Training Fellowship.
The study team would like to acknowledge the support of the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre.
Funding
This study has received funding from the Addenbrooke’s Charitable Trust and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes for Health (NIH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Professor Fiona Gilbert.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Two of the authors (JM, AT) have significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts may have been previously reported in other manuscripts (by other groups) using publicly available Osteoarthritis Initiative data. However, none of these studies have performed the analyses described in this manuscript.
Methodology
• retrospective
• case-control study
• multicentre study
Electronic supplementary material
ESM 1
(DOCX 34 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
MacKay, J.W., Kapoor, G., Driban, J.B. et al. Association of subchondral bone texture on magnetic resonance imaging with radiographic knee osteoarthritis progression: data from the Osteoarthritis Initiative Bone Ancillary Study. Eur Radiol 28, 4687–4695 (2018). https://doi.org/10.1007/s00330-018-5444-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5444-9