Abstract
Objectives
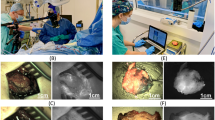
To assess the diagnostic performance of a new device for in situ label-free fluorescence spectral analysis of breast masses in freshly removed surgical specimens, in preparation for its clinical development.
Methods
Sixty-four breast masses from consenting patients who had undergone either a lumpectomy or a mastectomy were included. Label-free fluorescence spectral acquisitions were obtained with a 25G fibre-containing needle inserted into the mass. Data from benign and malignant masses were compared to establish the most discriminating thresholds and measurement algorithms. Accuracy was verified using the bootstrap method.
Results
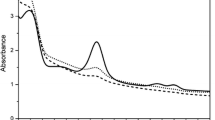
The final histological examination revealed 44 invasive carcinomas and 20 benign lesions. The maximum intensity of fluorescence signal was discriminant between benign and malignant masses (p < .0001) whatever their sizes. Statistical analysis indicated that choosing five random measurements per mass was the best compromise to obtain high sensitivity and high negative predictive value with the fewest measurements. Thus, malignant tumours were identified with a mean sensitivity, specificity, negative and positive predictive value of 98.8%, 85.4%, 97.2% and 93.5%, respectively.
Conclusion
This new in situ tissue autofluorescence evaluation device allows accurate discrimination between benign and malignant breast masses and deserves clinical development.
Key Points
• A new device allows in situ label-free fluorescence analysis of ex vivo breast masses
• Maximum fluorescence intensity discriminates benign from malignant masses (p < .0001)
• Five random measurements allow a high negative predictive value (97.2%)






Similar content being viewed by others
References
Raza S, Odulate A, EMW O et al (2010) Using real-time tissue elastography for breast lesion evaluation our initial experience. J Ultrasound Med 29:551–563
Delaloge S, Bonastre J, Borget I et al (2016) The challenge of rapid diagnosis in oncology: diagnostic accuracy and cost analysis of a large-scale one-stop breast clinic. Eur J Cancer 66:131–137
Wagnieres G, Star W (1998) In vivo fluorescence spectroscopy and imaging for oncological applications. Photochem Photobiol 68:603–632
Vo-Dinh T, Panjehpour M (1995) In vivo cancer diagnosis of the esophagus using differential normalized fluorescence (DNF) indices. Lasers Surg Med 16:41–47
Lane P, Lam S, Follen M, MacAulay C (2012) Oral fluorescence imaging using 405-nm excitation, aiding the discrimination of cancers and precancers by identifying changes in collagen and elastic breakdown and neovascularization in the underlying stroma. Gend Med 9:S78–S82.e8
McAlpine JN, El Hallani S, Lam SF et al (2011) Autofluorescence imaging can identify preinvasive or clinically occult lesions in fallopian tube epithelium: a promising step towards screening and early detection. Gynecol Oncol 120:385–392
Chen W, Gao X, Tian Q, Chen L (2011) A comparison of autofluorescence bronchoscopy and white light bronchoscopy in detection of lung cancer and preneoplastic lesions: a meta-analysis. Lung Cancer 73:183–188
Alfano R, Tata D, Cordero J et al (1984) Laser induced fluorescence spectroscopy from native cancerous and normal tissue. IEEE J Quantum Electron 20:1507–1511
Tang GC, Pradhan A, Alfano RR (1989) Spectroscopic differences between human cancer and normal lung and breast tissues. Lasers Surg Med 9:290–295
Yang Y, Katz A, Celmer EJ et al (1997) Fundamental differences of excitation spectrum between malignant and benign breast tissues. Photochem Photobiol 66:518–522
Gupta PK, Majumder SK, Uppal A (1997) Breast cancer diagnosis using N2 laser excited autofluorescence spectroscopy. Lasers Surg Med 21:417–422
Majumder SK, Gupta PK, Jain B, Uppal A (1999) UV excited autofluorescence spectroscopy of human breast tissue for discriminating cancerous tissue from benign tumor and normal tissue. Lasers Life Sci 8:249–264
Palmer GM, Zhu C, Breslin TM et al (2003) Comparison of multiexcitation fluorescence and diffuse reflectance spectroscopy for the diagnosis of breast cancer (March 2003). IEEE Trans Biomed Eng 50:1233–1242
Chowdary MVP, Mahato KK, Kumar KK et al (2009) Autofluorescence of breast tissues: evaluation of discriminating algorithms for diagnosis of normal, benign, and malignant conditions. Photomed Laser Surg 27:241–252
Volynskaya Z, Haka AS, Bechtel KL et al (2008) Diagnosing breast cancer using diffuse reflectance spectroscopy and intrinsic fluorescence spectroscopy. J Biomed Opt 13:024012
Alchab L, Dupuis G, Balleyguier C et al (2010) Towards an optical biopsy for the diagnosis of breast cancer in vivo by endogenous fluorescence spectroscopy. J Biophotonics 3:373–384
Gust L, Toullec A, Benoit C et al (2015) Pulmonary endogenous fluorescence allows the distinction of primary lung cancer from the perilesional lung parenchyma. PLoS One 10:e0134559
Sinn H-P, Kreipe H (2013) A brief overview of the WHO classification of breast tumors, 4th edition, focusing on issues and updates from the 3rd edition. Breast Care 8:149–154
International Electrotechnical Commission (2014) IEC 60825-1 / Safety of laser products – Part 1: Equipment classification and requirements. Int Stand
Thomsen S, Tatman D (1998) Physiological and pathological factors of human breast disease that can influence optical diagnosisa. Ann N Y Acad Sci 838:171–193
Peyrol S, Raccurt M, Gerard F et al (1997) Lysyl oxidase gene expression in the stromal reaction to in situ and invasive ductal breast carcinoma. Am J Pathol 150:497–507
Zhu C, Palmer GM, Breslin TM et al (2008) Diagnosis of breast cancer using fluorescence and diffuse reflectance spectroscopy: a Monte-Carlo-model-based approach. J Biomed Opt 13:034015
Alfano RR, Pradhan A, Tang GC, Wahl SJ (1989) Optical spectroscopic diagnosis of cancer and normal breast tissues. J Opt Soc Am B 6:1015–1023
Sordillo LA, Sordillo PP, Budansky Y et al (2014) Differences in fluorescence profiles from breast cancer tissues due to changes in relative tryptophan content via energy transfer: tryptophan content correlates with histologic grade and tumor size but not with lymph node metastases. J Biomed Opt 19:125002
Pu Y, Wang W, Yang Y, Alfano RR (2013) Native fluorescence spectra of human cancerous and normal breast tissues analyzed with non-negative constraint methods. Appl Opt 52:1293–1301
Onstad M, Stuckey A (2013) Benign breast disorders. Obstet Gynecol Clin N Am 40:459–473
Acknowledgements
We would like to thank the various biological resource centres for providing the paraffin blocks required for a centralized histological review.
We would also like to thank Lionel Auffray from the Fluids, Automatic and Thermal Systems Laboratory for his engineering expertise, particularly in high-quality 3D printing and Yuki Takahashi for editing this manuscript.
Funding
This study has received funding by Nodea Medical.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is MC Mathieu, MD
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Nodea Medical.
Statistics and biometry
MedPass International (France) kindly provided statistical analysis for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Methodology
• prospective
• observational
• multicentre study
Electronic supplementary material
Table S1
(JPEG 43 kb)
Rights and permissions
About this article
Cite this article
Mathieu, MC., Toullec, A., Benoit, C. et al. Preclinical ex vivo evaluation of the diagnostic performance of a new device for in situ label-free fluorescence spectral analysis of breast masses. Eur Radiol 28, 2507–2515 (2018). https://doi.org/10.1007/s00330-017-5228-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5228-7