Abstract
Purpose
Summarise survival of patients with resected lung cancers manifesting as part-solid nodules (PSNs).
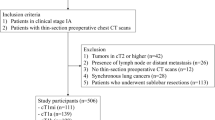
Methods
PubMed/MEDLINE and EMBASE databases were searched for all studies/clinical trials on CT-detected lung cancer in English before 21 December 2015 to identify surgically resected lung cancers manifesting as PSNs. Outcome measures were lung cancer-specific survival (LCS), overall survival (OS), or disease-free survival (DFS). All PSNs were classified by the percentage of solid component to the entire nodule diameter into category PSNs <80% or category PSNs ≥80%.
Results
Twenty studies reported on PSNs <80%: 7 reported DFS and 2 OS of 100%, 6 DFS 96.3-98.7%, and 11 OS 94.7-98.9% (median DFS 100% and OS 97.5%). Twenty-seven studies reported on PSNs ≥80%: 1 DFS and 2 OS of 100%, 19 DFS 48.0%-98.0% (median 82.6%), and 16 reported OS 43.0%-98.0% (median DFS 82.6%, OS 85.5%). Both DFS and OS were always higher for PSNs <80%.
Conclusion
A clear definition of the upper limit of solid component of a PSN is needed to avoid misclassification because cell-types and outcomes are different for PSN and solid nodules. The workup should be based on the size of the solid component.
Key points
• Lung cancers manifesting as PSNs are slow growing with high cure rates.
• Upper limits of the solid component are important for correct interpretation.
• Consensus definition is important for the management of PSNs.
• Median disease-free-survival (DFS) increased with decreasing size of the nodule.

Similar content being viewed by others
Abbreviations
- AIS:
-
Adenocarcinoma-in-situ
- DFS:
-
Disease-free or relapse-free survival
- GGO:
-
Ground-glass opacities
- I-ELCAP:
-
International Early Lung Cancer Action Program
- LCS:
-
Lung cancer-specific survival
- MIA:
-
Minimally invasive adenocarcinoma
- NLST:
-
National Lung Screening Trial
- NSN:
-
Nonsolid nodules
- OS:
-
Overall survival
- PSN:
-
Part-solid nodules
- TDR:
-
Disappearance rate
References
Yankelevitz DF, Yip R, Smith JP, Liang M, Liu Y, Xu DM et al (2015) CT screening for lung cancer: nonsolid nodules in baseline and annual repeat rounds. Radiology 277(2):555–564
Yip R, Yankelevitz DF, Hu M, Li K, Xu DM, Jirapatnakul A et al (2016) Lung cancer deaths in the National Lung Screening Trial attributed to nonsolid nodules. Radiology 281(2):589–596
Yip R, Wolf A, Tam K, Taioli E, Olkin I, Flores R et al (2016) Outcomes of lung cancers manifesting as nonsolid nodules. Lung Cancer 97:35–42
Henschke CI, Yip R, Smith JP, Wolf AS, Flores RM, Liang M et al (2016) CT screening for lung cancer: part-solid nodules in baseline and annual repeat rounds. AJR Am J Roentgenol 207(6):1176–1184
Yip R, Yankelevitz D, Li K, Xu D, Jirapatnakul A, Henschke C (2016) Lung cancer deaths in the National Lung Screening Trial attributed to cancers manifesting as part-solid nodules. AJR Am J Roentgenol. doi:10.2214/ajr.16.16930
Noguchi M, Morikawa A, Kawasaki M, Matsuno Y, Yamada T, Hirohashi S et al (1995) Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer 75(12):2844–2852
Noguchi M, Shimosato Y (1995) The development and progression of adenocarcinoma of the lung. Cancer Treat Res 72:131–142
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger K, Yatabe Y et al (2011) International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society: international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc 8(5):381–385
Travis W, Brambilla E, Burke A, Marx A, Nicholson A (2015) WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart, 4th edn. International Agency for Research on Cancer, Lyon
Travis WD, Asamura H, Bankier AA, Beasley MB, Detterbeck F, Flieder DB et al (2016) The IASLC Lung Cancer Staging Project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming Eighth Edition of the TNM Classification of Lung Cancer. J Thorac Oncol 11(8):1204–1223
Kuriyama K, Seto M, Kasugai T, Higashiyama M, Kido S, Sawai Y et al (1999) Ground-glass opacity on thin-section CT: value in differentiating subtypes of adenocarcinoma of the lung. AJR Am J Roentgenol 173(2):465–469
Henschke C, Yankelevitz D, Mirtcheva R, McGuinness G, McCauley D, Miettinen O (2002) CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 178(5):1053–1057
Sone S, Nakayama T, Honda T, Tsushima K, Li F, Haniuda M et al (2007) Long-term follow-up study of a population-based 1996-1998 mass screening programme for lung cancer using mobile low-dose spiral computed tomography. Lung Cancer 58(3):329–341
Hasegawa M, Sone S, Takashima S, Li F, Yang ZG, Maruyama Y et al (2000) Growth rate of small lung cancers detected on mass CT screening. Br J Radiol 73(876):1252–1259
Naidich DP, Bankier AA, MacMahon H, Schaefer-Prokop CM, Pistolesi M, Goo JM et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 266(1):304–317
MacMahon H, Naidich DP, Goo JM, Lee KS, Leung AN, Mayo JR et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: From the Fleischner Society 2017. Radiology 161659
Callister ME, Baldwin DR, Akram AR, Barnard S, Cane P, Draffan J et al (2015) British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 70(Suppl 2):ii1–ii54
Miettinen OS, Henschke CI, Smith JP, Yankelevitz DF (2014) Is ground glass descriptive of a type of pulmonary nodule? Radiology 270(1):311–312
Sugi K, Kobayashi S, Sudou M, Sakano H, Matsuda E, Okabe K (2010) Long-term prognosis of video-assisted limited surgery for early lung cancer. Eur J Cardiothorac Surg 37(2):456–460
Matsuguma H, Mori K, Nakahara R, Suzuki H, Kasai T, Kamiyama Y et al (2013) Characteristics of subsolid pulmonary nodules showing growth during follow-up with CT scanning. Chest 143(2):436–443
Kim EA, Johkoh T, Lee KS, Han J, Fujimoto K, Sadohara J et al (2001) Quantification of ground-glass opacity on high-resolution CT of small peripheral adenocarcinoma of the lung: pathologic and prognostic implications. AJR Am J Roentgenol 177(6):1417–1422
Nakamura H, Saji H, Ogata A, Saijo T, Okada S, Kato H (2004) Lung cancer patients showing pure ground-glass opacity on computed tomography are good candidates for wedge resection. Lung Cancer 44(1):61–68
Tateishi U, Muller NL, Johkoh T, Maeshima A, Asamura H, Satake M et al (2005) Mucin-producing adenocarcinoma of the lung: thin-section computed tomography findings in 48 patients and their effect on prognosis. J Comput Assist Tomogr 29(3):361–368
Fukui T, Katayama T, Ito S, Abe T, Hatooka S, Mitsudomi T (2009) Clinicopathological features of small-sized non-small cell lung cancer with mediastinal lymph node metastasis. Lung Cancer 66(3):309–313
Vazquez M, Carter D, Brambilla E, Gazdar A, Noguchi M, Travis WD et al (2009) Solitary and multiple resected adenocarcinomas after CT screening for lung cancer: histopathologic features and their prognostic implications. Lung Cancer 64(2):148–154
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M et al (2012) Prognostic significance of using solid versus whole tumor size on high-resolution computed tomography for predicting pathologic malignant grade of tumors in clinical stage IA lung adenocarcinoma: a multicenter study. J Thorac Cardiovasc Surg 143(3):607–612
Nakamura S, Fukui T, Taniguchi T, Usami N, Kawaguchi K, Ishiguro F et al (2013) Prognostic impact of tumor size eliminating the ground glass opacity component: modified clinical T descriptors of the tumor, node, metastasis classification of lung cancer. J Thorac Oncol 8(12):1551–1557
Gierada DS, Pinsky P, Nath H, Chiles C, Duan F, Aberle DR (2014) Projected outcomes using different nodule sizes to define a positive CT lung cancer screening examination. J Natl Cancer Inst. 106(11)
Iwata H, Shirahashi K, Mizuno Y, Yamamoto H, Takemura H (2014) Feasibility of segmental resection in non-small-cell lung cancer with ground-glass opacity. Eur J Cardiothorac Surg 46(3):375–379, discussion 9
Hattori A, Suzuki K, Takamochi K, Oh S (2015) Clinical features of multiple lung cancers based on thin-section computed tomography: what are the appropriate surgical strategies for second lung cancers? Surg Today 45(2):189–196
Kobayashi Y, Sakao Y, Deshpande GA, Fukui T, Mizuno T, Kuroda H et al (2014) The association between baseline clinical-radiological characteristics and growth of pulmonary nodules with ground-glass opacity. Lung Cancer 83(1):61–66
Kodama H, Yamakado K, Hasegawa T, Takao M, Taguchi O, Fukai I et al (2014) Radiofrequency ablation for ground-glass opacity-dominant lung adenocarcinoma. J Vasc Interv Radiol 25(3):333–339
Nakata M, Sawada S, Saeki H, Takashima S, Mogami H, Teramoto N et al (2003) Prospective study of thoracoscopic limited resection for ground-glass opacity selected by computed tomography. Ann Thorac Surg 75(5):1601–1605, discussion 5-6
Henschke CI, Shaham D, Yankelevitz DF, Kramer A, Kostis WJ, Reeves AP et al (2006) CT screening for lung cancer: significance of diagnoses in its baseline cycle. Clin Imaging 30(1):11–15
Henschke CI, Yankelevitz DF, Miettinen OS (2006) International Early Lung Cancer Action Program I. Computed tomographic screening for lung cancer: the relationship of disease stage to tumor size. Arch Intern Med 166(3):321–325
Kodama K, Higashiyama M, Takami K, Oda K, Okami J, Maeda J et al (2008) Treatment strategy for patients with small peripheral lung lesion(s): intermediate-term results of prospective study. Eur J Cardiothorac Surg 34(5):1068–1074
Carretta A, Ciriaco P, Melloni G, Bandiera A, Libretti L, Puglisi A et al (2009) Surgical treatment of multiple primary adenocarcinomas of the lung. Thorac Cardiovasc Surg 57(1):30–34
Kohno T, Fujimori S, Kishi K, Fujii T (2010) Safe and effective minimally invasive approaches for small ground glass opacity. Ann Thorac Surg 89(6):S2114–S2117
Zhou Q, Suzuki K, Anami Y, Oh S, Takamochi K (2010) Clinicopathologic features in resected subcentimeter lung cancer − status of lymph node metastases. Interact Cardiovasc Thorac Surg 10(1):53–57
Matsunaga T, Suzuki K, Hattori A, Fukui M, Kitamura Y, Miyasaka Y et al (2013) Lung cancer with scattered consolidation: detection of new independent radiological category of peripheral lung cancer on thin-section computed tomography. Interact Cardiovasc Thorac Surg 16(4):445–449
Ambrosini-Spaltro A, Ruiu A, Seebacher C, Vattemi E, Gentile L, Feil B et al (2014) Impact of the IASLC/ATS/ERS classification in pN0 pulmonary adenocarcinomas: a study with radiological-pathological comparisons and survival analyses. Pathol Res Pract 210(1):40–46
Ye B, Cheng M, Ge XX, Geng JF, Li W, Feng J et al (2014) Factors that predict lymph node status in clinical stage T1aN0M0 lung adenocarcinomas. World J Surg Oncol 12:42
Ye B, Cheng M, Li W, Ge XX, Geng JF, Feng J et al (2014) Predictive factors for lymph node metastasis in clinical stage IA lung adenocarcinoma. Ann Thorac Surg 98(1):217–223
Kudo Y, Matsubayashi J, Saji H, Akata S, Shimada Y, Kato Y et al (2015) Association between high-resolution computed tomography findings and the IASLC/ATS/ERS classification of small lung adenocarcinomas in Japanese patients. Lung Cancer 90(1):47–54
Yoshioka M, Ichiguchi O (2009) Selection of sublobar resection for c-stage IA non-small cell lung cancer based on a combination of structural imaging by CT and functional imaging by FDG PET. Ann Thorac Cardiovasc Surg 15(2):82–88
Matsuguma H, Yokoi K, Anraku M, Kondo T, Kamiyama Y, Mori K et al (2002) Proportion of ground-glass opacity on high-resolution computed tomography in clinical T1 N0 M0 adenocarcinoma of the lung: A predictor of lymph node metastasis. J Thorac Cardiovasc Surg 124(2):278–284
Matsuguma H, Nakahara R, Anraku M, Kondo T, Tsuura Y, Kamiyama Y et al (2004) Objective definition and measurement method of ground-glass opacity for planning limited resection in patients with clinical stage IA adenocarcinoma of the lung. Eur J Cardiothorac Surg 25(6):1102–1106
Sagawa M, Higashi K, Usuda K, Aikawa H, Machida Y, Tanaka M et al (2009) Curative wedge resection for non-invasive bronchioloalveolar carcinoma. Tohoku J Exp Med 217(2):133–137
Kim TJ, Park CM, Goo JM, Lee KW (2012) Is there a role for FDG PET in the management of lung cancer manifesting predominantly as ground-glass opacity? AJR Am J Roentgenol 198(1):83–88
Seok Y, Cho S, Kim K, Jheon S (2014) Partly solid pulmonary nodules: waiting for change or surgery outright? Interact Cardiovasc Thorac Surg 19(4):556–560
Yoshida J, Ishii G, Hishida T, Aokage K, Tsuboi M, Ito H et al (2015) Limited resection trial for pulmonary ground-glass opacity nodules: case selection based on high-resolution computed tomography-interim results. Jpn J Clin Oncol 45(7):677–681
Ohta Y, Shimizu Y, Kobayashi T, Matsui O, Minato H, Matsumoto I et al (2006) Pathologic and biological assessment of lung tumors showing ground-glass opacity. Ann Thorac Surg 81(4):1194–1197
Suzuki K, Kusumoto M, Watanabe S, Tsuchiya R, Asamura H (2006) Radiologic classification of small adenocarcinoma of the lung: radiologic-pathologic correlation and its prognostic impact. Ann Thorac Surg 81(2):413–419
Asamura H, Suzuki K, Watanabe S, Matsuno Y, Maeshima A, Tsuchiya R (2003) A clinicopathological study of resected subcentimeter lung cancers: a favorable prognosis for ground glass opacity lesions. Ann Thorac Surg 76(4):1016–1022
Ohde Y, Nagai K, Yoshida J, Nishimura M, Takahashi K, Suzuki K et al (2003) The proportion of consolidation to ground-glass opacity on high resolution CT is a good predictor for distinguishing the population of non-invasive peripheral adenocarcinoma. Lung Cancer 42(3):303–310
Aokage K, Yoshida J, Ishii G, Matsumura Y, Haruki T, Hishida T et al (2013) Identification of early t1b lung adenocarcinoma based on thin-section computed tomography findings. J Thorac Oncol 8(10):1289–1294
Duann CW, Hung JJ, Hsu PK, Huang CS, Hsieh CC, Hsu HS et al (2013) Surgical outcomes in lung cancer presenting as ground-glass opacities of 3 cm or less: a review of 5 years' experience. J Chin Med Assoc 76(12):693–697
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M et al (2014) Segmentectomy for clinical stage IA lung adenocarcinoma showing solid dominance on radiology. Eur J Cardiothorac Surg 46(4):637–642
Yanagawa M, Tanaka Y, Leung AN, Morii E, Kusumoto M, Watanabe S et al (2014) Prognostic importance of volumetric measurements in stage I lung adenocarcinoma. Radiology 272(2):557–567
Cho JH, Choi YS, Kim J, Kim HK, Zo JI, Shim YM (2015) Long-term outcomes of wedge resection for pulmonary ground-glass opacity nodules. Ann Thorac Surg 99(1):218–222
Hattori A, Suzuki K, Matsunaga T, Miyasaka Y, Takamochi K, Oh S (2015) What is the appropriate operative strategy for radiologically solid tumours in subcentimetre lung cancer patients?dagger. Eur J Cardiothorac Surg 47(2):244–249
Li Z, Ye B, Bao M, Xu B, Chen Q, Liu S et al (2015) Radiologic predictors for clinical stage IA lung adenocarcinoma with ground glass components: a multi-center study of long-term outcomes. PLoS One 10(9), e0136616
Nakamura S, Fukui T, Kawaguchi K, Fukumoto K, Hirakawa A, Yokoi K (2015) Does ground glass opacity-dominant feature have a prognostic significance even in clinical T2aN0M0 lung adenocarcinoma? Lung Cancer 89(1):38–42
Sakurai H, Nakagawa K, Watanabe S, Asamura H (2015) Clinicopathologic features of resected subcentimeter lung cancer. Ann Thorac Surg 99(5):1731–1738
Yano M, Yoshida J, Koike T, Kameyama K, Shimamoto A, Nishio W et al (2015) Survival of 1737 lobectomy-tolerable patients who underwent limited resection for cStage IA non-small-cell lung cancer. Eur J Cardiothorac Surg 47(1):135–142
Kodama K, Higashiyama M, Yokouchi H, Takami K, Kuriyama K, Mano M et al (2001) Prognostic value of ground-glass opacity found in small lung adenocarcinoma on high-resolution CT scanning. Lung Cancer 33(1):17–25
Aoki T, Tomoda Y, Watanabe H, Nakata H, Kasai T, Hashimoto H et al (2001) Peripheral lung adenocarcinoma: correlation of thin-section CT findings with histologic prognostic factors and survival. Radiology 220(3):803–809
Takashima S, Maruyama Y, Hasegawa M, Saito A, Haniuda M, Kadoya M (2003) High-resolution CT features: prognostic significance in peripheral lung adenocarcinoma with bronchioloalveolar carcinoma components. Respiration 70(1):36–42
Ikeda N, Maeda J, Yashima K, Tsuboi M, Kato H, Akada S et al (2004) A clinicopathological study of resected adenocarcinoma 2 cm or less in diameter. Ann Thorac Surg 78(3):1011–1016
Sakao Y, Nakazono T, Sakuragi T, Natsuaki M, Itoh T (2004) Predictive factors for survival in surgically resected clinical IA peripheral adenocarcinoma of the lung. Ann Thorac Surg 77(4):1157–1161, discussion 61-2
Seki N, Sawada S, Nakata M, Inoue T, Nishimura R, Segawa Y et al (2008) Lung cancer with localized ground-glass attenuation represents early-stage adenocarcinoma in nonsmokers. J Thorac Oncol 3(5):483–490
Higashi K, Sakuma T, Ito K, Niho S, Ueda Y, Kobayashi T et al (2009) Combined evaluation of preoperative FDG uptake on PET, ground-glass opacity area on CT, and serum CEA level: identification of both low and high risk of recurrence in patients with resected T1 lung adenocarcinoma. Eur J Nucl Med Mol Imaging 36(3):373–381
Inoue M, Minami M, Sawabata N, Utsumi T, Kadota Y, Shigemura N et al (2010) Clinical outcome of resected solid-type small-sized c-stage IA non-small cell lung cancer. Eur J Cardiothorac Surg 37(6):1445–1449
Shi CL, Zhang XY, Han BH, He WZ, Shen J, Chu TQ (2011) A clinicopathological study of resected non-small cell lung cancers 2 cm or less in diameter: a prognostic assessment. Med Oncol 28(4):1441–1446
Lederlin M, Puderbach M, Muley T, Schnabel PA, Stenzinger A, Kauczor HU et al (2013) Correlation of radio- and histomorphological pattern of pulmonary adenocarcinoma. Eur Respir J 41(4):943–951
Matsuguma H, Oki I, Nakahara R, Suzuki H, Kasai T, Kamiyama Y et al (2013) Comparison of three measurements on computed tomography for the prediction of less invasiveness in patients with clinical stage I non-small cell lung cancer. Ann Thorac Surg 95(6):1878–1884
Shiono S, Yanagawa N, Abiko M, Sato T (2014) Detection of non-aggressive stage IA lung cancer using chest computed tomography and positron emission tomography/computed tomography. Interact Cardiovasc Thorac Surg 19(4):637–643
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M et al (2014) Appropriate sublobar resection choice for ground glass opacity-dominant clinical stage IA lung adenocarcinoma: wedge resection or segmentectomy. Chest 145(1):66–71
Hwang EJ, Park CM, Ryu Y, Lee SM, Kim YT, Kim YW et al (2015) Pulmonary adenocarcinomas appearing as part-solid ground-glass nodules: is measuring solid component size a better prognostic indicator? Eur Radiol 25(2):558–567
Kakinuma R, Kodama K, Yamada K, Yokoyama A, Adachi S, Mori K et al (2008) Performance evaluation of 4 measuring methods of ground-glass opacities for predicting the 5-year relapse-free survival of patients with peripheral nonsmall cell lung cancer: a multicenter study. J Comput Assist Tomogr 32(5):792–798
Okada M, Nakayama H, Okumura S, Daisaki H, Adachi S, Yoshimura M et al (2011) Multicenter analysis of high-resolution computed tomography and positron emission tomography/computed tomography findings to choose therapeutic strategies for clinical stage IA lung adenocarcinoma. J Thorac Cardiovasc Surg 141(6):1384–1391
Dong B, Sato M, Sagawa M, Endo C, Usuda K, Sakurada A et al (2002) Computed tomographic image comparison between mediastinal and lung windows provides possible prognostic information in patients with small peripheral lung adenocarcinoma. J Thorac Cardiovasc Surg 124(5):1014–1020
Murakawa T, Konoeda C, Ito T, Inoue Y, Sano A, Nagayama K et al (2013) The ground glass opacity component can be eliminated from the T-factor assessment of lung adenocarcinoma. Eur J Cardiothorac Surg 43(5):925–932
Hashizume T, Yamada K, Okamoto N, Saito H, Oshita F, Kato Y et al (2008) Prognostic significance of thin-section CT scan findings in small-sized lung adenocarcinoma. Chest 133(2):441–447
Henschke CI, Yankelevitz DF, Libby DM, Pasmantier MW, Smith JP, Miettinen OS (2006) Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med. 1763–1771. United States: 2006 Massachusetts Medical Society
Henschke CI, Yankelevitz DF, Yip R, Reeves AP, Farooqi A, Xu D et al (2012) Lung cancers diagnosed at annual CT screening: volume doubling times. Radiology 263(2):578–583
Network NCC. Clinical Practice Guidelines in Oncology (NCCN Guidelines). Version 1.2014 Lung Cancer Screening. http://www.nccn.org/professionals/physician_gls/pdf/lung_screening.pdf. Accessed March 27, 2015
Higashiyama M, Kodama K, Yokouchi H, Takami K, Mano M, Kido S et al (1999) Prognostic value of bronchiolo-alveolar carcinoma component of small lung adenocarcinoma. Ann Thorac Surg 68(6):2069–2073
International Early Lung Cancer Action Program Protocol http://www.ielcap.org/sites/default/files/I-ELCAP%20protocol-v21-3-1-14.pdf. Accessed May 30, 2017
Henschke C, Yankelevitz D, Naidich D, McCauley D, McGuinness G, Libby D et al (2004) CT screening for lung cancer: suspiciousness of nodules according to size on baseline scans. Radiology 231(1):164–168
Henschke C, Yip R, Yankelevitz D, Smith J (2013) Definition of a positive test result in computed tomography screening for lung cancer: a cohort study. Ann Intern Med 158(4):246–252
Yip R, Henschke C, Yankelevitz D, Boffetta P, Smith J (2015) The International Early Lung Cancer Investigators. The impact of the regimen of screening on lung cancer cure: a comparison of I-ELCAP and NLST. Eur J Cancer Prev 24(3):201–208
Ettinger DS, Wood DE, Akerley W, Bazhenova LA, Borghaei H, Camidge DR et al (2016) NCCN Guidelines Insights: Non-Small Cell Lung Cancer, Version 4.2016. J Natl Compr Canc Netw 14(3):255–264
Pinsky PF, Gierada DS, Black W, Munden R, Nath H, Aberle D et al (2015) Performance of Lung-RADS in the National Lung Screening Trial: a retrospective assessment. Ann Intern Med 162(7):485–491
Kazerooni E, Austin J, Black W, Dyer D, Hazelton T, Leung A et al (2014) ACR-STR practice parameter for the performance and reporting of lung cancer screening thoracic computed tomography. J Thorac Imaging 29(5):310–316
American College of Radiology. http://www.acr.org/Quality-Safety/Resources/LungRADS. Accessed May 30, 2017
Acknowledgements
We would also like to thank Ms. Camille Chan, who provided assistance with the literature search and identification of relevant studies to be included in this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantors of this publication are Dr Claudia Henschke and Ms. Rowena Yip.
Conflict of interest
Dr Yankelevitz is a named inventor on a number of patents and patent applications relating to the evaluation of diseases of the chest including measurement of nodules. Some of these, which are owned by Cornell Research Foundation (CRF), are non-exclusively licensed to General Electric. As an inventor of these patents, Dr Yankelevitz is entitled to a share of any compensation that CRF may receive from its commercialisation of these patents. He is also an equity owner in Accumetra, a privately held technology company committed to improving the science and practice of image-based decision-making. Dr Yankelevitz also serves on the advisory board of GRAIL.
Dr Henschke is the President and serves on the board of the Early Diagnosis and Treatment Research Foundation. She receives no compensation from the Foundation. The Foundation is established to provide grants for projects, conferences, and public databases for research on early diagnosis and treatment of diseases. Dr Claudia Henschke is also a named inventor on a number of patents and patent applications relating to the evaluation of pulmonary nodules on CT scans of the chest that are owned by Cornell Research Foundation (CRF). Since 2009, Dr Henschke has not accepted any financial benefit from these patents including royalties and any other proceeds related to the patents or patent applications owned by CRF.
Other authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Funding
Funding for this study was in part by the Flight Attendants Medical Research Institute.
Statistics and biometry
Dr. Claudia Henschke, Ms. Rowena Yip, Dr Betsy Becker and Dr Emanuela Taioli kindly provided statistical advice for this manuscript.
At least one of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because this study is a review of existing literature and no human subjects were involved.
Ethical approval
Institutional Review Board approval was not required because this study is a review of existing literature and no human subjects were involved.
Methodology
• prospective
• observational
• multi-centre study
Appendix A
Appendix A
Part Solid - All Concept
Embase
-
1.
part-solid.mp.
-
2.
partsolid.mp.
-
3.
semi-solid.mp.
-
4.
semisolid.mp.
-
5.
subsolid.mp.
-
6.
ground glass.mp.
-
7.
1 or 2 or 3 or 4 or 5 or 6
-
8.
lung cancer/
-
9.
lung tumor/
-
10.
((lung or pulmonary) and (cancer or cancers or tumor or tumors or carcinoma or carcinomas or neoplasm or neoplasms)).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
11.
8 or 9 or 10
-
12.
mortality/or cancer mortality/
-
13.
disease free survival/or cancer survival/or disease specific survival/or event free survival/or cancer specific survival/or long term survival/or metastasis free survival/or survival/or overall survival/
-
14.
recurrent disease/
-
15.
metastasis/or lung metastasis/
-
16.
(mortality or survival or recurrence or metastasis or metastases or death rate or relapsing disease or relapse).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
17.
12 or 13 or 14 or 15 or 16
-
18.
computer assisted tomography/
-
19.
(CT scan or CT scans or CAT scan or cat scans).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
20.
(Comput$ adj3 Tomography).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
21.
18 or 19 or 20
-
22.
7 and 11 and 17 and 21
PS all concept
Medline
-
1.
Solitary Pulmonary Nodule/or part-solid.mp.
-
2.
part solid.mp.
-
3.
semi-solid.mp.
-
4.
semisolid.mp.
-
5.
subsolid.mp. or Solitary Pulmonary Nodule/
-
6.
ground glass.mp.
-
7.
ground-glass.mp.
-
8.
1 or 2 or 3 or 4 or 5 or 6 or 7
-
9.
Disease-Free Survival/or Survival Analysis/or Survival/or Survival Rate/or survival.mp.
-
10.
Hospital Mortality/or Mortality/or mortality.mp.
-
11.
Recurrence/or Neoplasm Recurrence, Local/or recurrence.mp.
-
12.
metastasis.mp. or Neoplasm Metastasis/
-
13.
metastases.mp. or Neoplasm Metastasis/
-
14.
fatality.mp.
-
15.
fatalities.mp.
-
16.
9 or 10 or 11 or 12 or 13 or 14 or 15
-
17.
cancer.mp. or Neoplasms/
-
18.
cancers.mp. or Neoplasms/
-
19.
carcinoma.mp. or Carcinoma/or Carcinoma, Small Cell/or Carcinoma, Non-Small-Cell Lung/or Carcinoma, Squamous Cell/or Carcinoma, Adenosquamous/
-
20.
carcinomas.mp. or Carcinoma/
-
21.
tumor.mp. or Neoplasms/
-
22.
tumors.mp. or Neoplasms/
-
23.
17 or 18 or 19 or 20 or 21 or 22
-
24.
lung.mp. or Lung/
-
25.
pulmonary.mp.
-
26.
24 or 25
-
27.
23 and 26
-
28.
Lung Neoplasms.mp. or Lung Neoplasms/
-
29.
27 or 28
-
30.
CT scan.mp.
-
31.
CT scans.mp.
-
32.
CAT scan.mp.
-
33.
CAT scans.mp.
-
34.
Tomography, X-Ray Computed/or computed scan.mp.
-
35.
Tomography, X-Ray Computed/or computed scans.mp.
-
36.
Tomography, X-Ray Computed/or computed assisted tomography.mp.
-
37.
computerized scan.mp.
-
38.
computerized scans.mp.
-
39.
30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38
-
40.
8 and 16 and 29 and 39
Rights and permissions
About this article
Cite this article
Yip, R., Li, K., Liu, L. et al. Controversies on lung cancers manifesting as part-solid nodules. Eur Radiol 28, 747–759 (2018). https://doi.org/10.1007/s00330-017-4975-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4975-9