Abstract
Purpose
The National Lung Screening Trial (NLST) demonstrated a reduction in lung cancer and all-cause mortality with low-dose CT (LDCT) screening. The aim of our study was to examine the time to diagnosis (TTD) of lung cancer in the LDCT arm of the NLST and assess its relationship with cancer characteristics and survival.
Methods
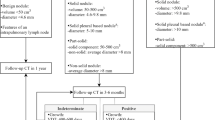
The subjects (N = 462) with a positive baseline screen and subsequent lung cancer diagnosis within 3 years were evaluated by data and image review to confirm the baseline abnormality. The cases were analysed for the relationship between TTD and imaging features, cancer type, stage and survival for 7 years from baseline screen.
Results
Cancer was judged to be present at baseline in 397/462 cases. The factors that showed significant association (p value trend less than 0.05) with longer TTD included smaller nodule size, pure ground glass nodules (GGNs), smooth/lobulated margins, stages I/II, adenocarcinoma, and decreasing lung cancer mortality. The logistic regression model for lung cancer death showed significant inverse relationships with size less than 20 mm (OR = 0.32), pure GGNs (OR = 0.24), adenocarcinoma (OR = 0.57) and direct relationship with age (OR = 1.4).
Conclusion
TTD after a positive LDCT screen in the NLST showed a strong association with imaging features, stage and mortality.
Key Points
• NLST observed variable time to lung cancer diagnosis from positive baseline screen.
• Time to diagnosis was associated with imaging features, cancer type and stage.
• In univariate but not multivariate analysis, longer TTD correlated with decreased mortality.
Similar content being viewed by others
References
American Cancer Society (2014) Cancer facts & figures, 2014. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures 2014.html. Accessed 22 Mar 2017
NIH (2017) National Cancer Institute: Surveillance, Epidemiology, and End Results (SEER) Program Cancer statistics review, 2006–2012. https://seer.cancer.gov/statfacts/html/lungb.html. Accessed 22 Mar 2017
National Lung Screening Trial Research Team, Aberle DR, Adams AM et al (2011) Reduced lung cancer mortality with low-dose computed tomographic screening. N Engl J Med 365:395–409
Aberle DR, DeMello S, Berg CD et al (2013) Results of the two incidence screenings in the National Lung Screening Trial. N Engl J Med 369:920–931
National Lung Screening Trial Research Team, Aberle DR, Berg CD et al (2011) The National Lung Screening Trial: overview and study design. Radiology 258:243–253
Olsson JK, Schultz EM, Gould MK (2009) Timeliness of care in patients with lung cancer: a systematic review. Thorax 64:749–756
Koyi H, Hillerdal G, Brandén E (2002) Patient’s and doctors’ delays in the diagnosis of chest tumors. Lung Cancer 35:53–57
Porta M, Gallén M, Malats N, Planas J (1991) Influence of ‘diagnostic delay’ upon cancer survival: an analysis of five tumour sites. J Epidemiol Community Health 45:225–230
Pita-Fernández S, Montero-Martinez C, Pértega-Diaz S, Verea-Hernando H (2003) Relationship between delayed diagnosis and the degree of invasion and survival in lung cancer. J Clin Epidemiol 56:820–825
Salomaa ER, Sällinen S, Hiekkanen H, Liippo K (2005) Delays in the diagnosis and treatment of lung cancer. Chest 128:2282–2288
Kanashiki M, Satoh H, Ishikawa H, Yamashita YT, Ohtsuka M, Sekizawa K (2003) Time from finding abnormality on mass screening to final diagnosis of lung cancer. Oncol Rep 10:649–652
Kashiwabara K, Koshi S, Itonaga K, Nakahara O, Tanaka M, Toyonaga M (2003) Outcome in patients with lung cancer found on lung cancer mass screening roentgenograms, but who did not subsequently consult a doctor. Lung Cancer 40:67–72
Tørring ML, Frydenberg M, Hansen RP, Olesen F, Vedsted P (2013) Evidence of increasing mortality with longer diagnostic intervals for five common cancers: a cohort study in primary care. Eur J Cancer 49:2187–2198
Myrdal G, Lambe M, Hillerdal G, Lamberg K, Agustsson T, Ståhle E (2004) Effect of delays on prognosis in patients with non-small cell lung cancer. Thorax 59:45–49
Comber H, Cronin DP, Deady S, Lorcain PO, Riordan P (2005) Delays in treatment in the cancer services: impact on cancer stage and survival. Ir Med J 98:238–299
Annakkaya AN, Arbak P, Balbay O, Bilgin C, Erbas M, Bulut I (2007) Effect of symptom-to-treatment interval on prognosis in lung cancer. Tumori 93:61–67
Kodama K, Higashiyama M, Yokouchi H et al (2001) Prognostic value of ground-glass opacity found in small lung adenocarcinoma on high-resolution CT scanning. Lung Cancer 33:17–25
ELCAP Group, Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS (2002) CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 178:1053–1057
Vazquez M, Carter D, Brambilla E et al (2009) Solitary and multiple resected adenocarcinomas after CT screening for lung cancer: histopathologic features and their prognostic implications. Lung Cancer 64:148–154
Heyneman LE, Patz EF (2002) PET imaging in patients with bronchioloalveolar cell carcinoma. Lung Cancer 38:261–266
Wu HB, Wang L, Wang QS et al (2015) Adenocarcinoma with BAC features presented as the nonsolid nodule is prone to be false-negative on 18 F-FDGPET/CT. Biomed Res Int 2015:243681
Chang B, Hwang JH, Choi YH et al (2013) Natural history of pure ground glass opacity lung nodules detected by low-dose CT scan. Chest 143:172–178
Yip R, Yankelevitz DF, Hu M et al (2016) Lung cancer deaths in the National Lung Screening Trial attributed to nonsolid nodules. Radiology 281:589–596
MacMahon H, Naidich DP, Goo JM et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. doi:10.1148/radiol.2017161659
Guideline Development Group, Baldwin DR, Callister ME (2015) The British Thoracic Society guidelines on the investigation and management of pulmonary nodules. Thorax 70:794–798
Lung-RADS™ Version 1.0 Assessment Categories. Release date April 28, 2014
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Paul Pinsky.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
This study has received funding by NIH and our research is a subanalysis from the original data.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study as a part of NLST enrolment.
Ethical approval
Institutional review board approval was obtained.
Study subjects or cohorts overlap
The study subjects or cohorts have not been previously reported.
Methodology
• Retrospective
• Observational
• Multicentre study
Rights and permissions
About this article
Cite this article
Sonavane, S.K., Pinsky, P., Watts, J. et al. The relationship of cancer characteristics and patient outcome with time to lung cancer diagnosis after an abnormal screening CT. Eur Radiol 27, 5113–5118 (2017). https://doi.org/10.1007/s00330-017-4886-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4886-9