Abstract
Objectives
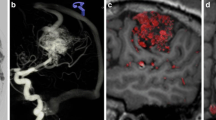
The current gold standard in the assessment of lateral intracranial dural arteriovenous fistulas (LDAVF) is digital subtraction angiography (DSA). However, magnetic resonance imaging (MRI) is a non-invasive emerging tool for the evaluation of such lesions. The aim of our study was to compare the DSA to our 3 T MR-imaging protocol including a highly spatial resolved (ce-MRA) and a temporal resolved (“time-resolved imaging of contrast kinetics”, TRICKS) contrast-enhanced MR angiography to evaluate if solely DSA can remain the gold-standard imaging modality for the treatment planning of LDAVF.
Methods
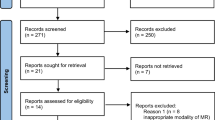
We retrospectively reviewed matched pairs of DSA and 3 T MRI examinations of 24 patients with LDAVF (03/2008–04/2014) by the same list of relevant criteria for an endovascular LDAVF treatment planning. In particular, we determined intermodality agreement for the Cognard classification, the identifeication of arterial feeders, and the detailed assessment of each venous drainage pattern.
Results
Intermodality agreement for the Cognard classification was excellent (ĸ = 1.0). Whereas MRI failed in identifying small arterial feeders, it was superior to the DSA in the assessment of the sinus and the venous drainage pattern.
Conclusions
The combination of MRI and DSA is the new gold standard in LDAVF treatment planning.
Key Points
• DSA is superior to the MRI in detecting LDAVF arterial feeders.
• MRI excellently evaluates the venous side of an LDAVF.
• MRI can replace DSA in initial diagnosis and monitoring of LDAVF.
• MRI and DSA combined are the new gold standard in LDAVF treatment planning.



Similar content being viewed by others
Abbreviations
- LDAVF:
-
Lateral dural arteriovenous fistula
- DSA:
-
Digital subtraction angiography
- MRI:
-
Magnetic resonance imaging
- MRA:
-
Magnetic resonance angiography
- TRICKS:
-
Time-resolved imaging of contrast kinetics
- FLAIR:
-
Fluid-attenuated inversion recovery
- FSPGR:
-
Fast spoiled gradient echo
- TOF:
-
Time of flight
- ce-MRA:
-
Contrast-enhanced magnetic resonance angiography
- TR:
-
Repetition time
- TE:
-
Echo time
- FOV:
-
Field of view
- ST:
-
Slice thickness
- PACS:
-
Picture archiving and communication system
- AOE:
-
A. occipitalis externa
- AMM:
-
A. meningea media
- AAP:
-
A. auricularis posterior
- APharAsc:
-
A. pharyngea ascendens
- ATent:
-
A. tentorii
- AMP:
-
A. meningea posterior
- VA:
-
Vertebral artery
- BJV:
-
Bulb of jugular vein
- SigS:
-
Sigmoid sinus
- TrS:
-
Transverse sinus
- CS:
-
Confluence of sinuses
- StrS:
-
Straight sinus
- SSS:
-
Superior sagittal sinus
- SD:
-
Standard deviation
- DWI :
-
Diffusion weighted imaging
References
Borden JA, Wu JK, Shucart WA (1995) A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg 82:166–179
Nishimura S, Hirai T, Sasao A et al (2010) Evaluation of dural arteriovenous fistulas with 4D contrast-enhanced MR angiography at 3T. AJNR Am J Neuroradiol 31:80–85
Van Dijk JMC, terBrugge KG, Willinsky RA, Wallace MC (2002) Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke J Cereb Circ 33:1233–1236
Cognard C, Gobin YP, Pierot L et al (1995) Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology 194:671–680
Farb RI, Agid R, Willinsky RA et al (2009) Cranial dural arteriovenous fistula: diagnosis and classification with time-resolved MR angiography at 3T. AJNR Am J Neuroradiol 30:1546–1551
Bink A, Berkefeld J, Wagner M et al (2012) Detection and grading of dAVF: prospects and limitations of 3T MRI. Eur Radiol 22:429–438
Meckel S, Maier M, Ruiz DSM et al (2007) MR angiography of dural arteriovenous fistulas: diagnosis and follow-up after treatment using a time-resolved 3D contrast-enhanced technique. AJNR Am J Neuroradiol 28:877–884
Korosec FR, Frayne R, Grist TM, Mistretta CA (1996) Time-resolved contrast-enhanced 3D MR angiography. Magn Reson Med 36:345–351
Cashen TA, Carr JC, Shin W et al (2006) Intracranial time-resolved contrast-enhanced MR angiography at 3T. AJNR Am J Neuroradiol 27:822–829
Jang J, Schmitt P, Kim B et al (2014) Non-contrast-enhanced 4D MR angiography with STAR spin labeling and variable flip angle sampling: a feasibility study for the assessment of Dural Arteriovenous Fistula. Neuroradiology 56:305–314
Iryo Y, Hirai T, Kai Y et al (2014) Intracranial dural arteriovenous fistulas: evaluation with 3-T four-dimensional MR angiography using arterial spin labeling. Radiology 271:193–199
Acknowledgments
Our special thanks are extended to Dr. A. Crispin (Institute for Medical Informatics, Biometry and Epidemiology, University of Munich) for his professional guidance and valuable statistical advice. The scientific guarantor of this publication is Prof. H. Brückmann. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Part of the data (patient overlap: 20) was presented in the annual meeting of the German Society of Neuroradiology in 10/2013 and awarded as best presentation by „Der Lebenszweig e.V. - Verein für Hirn-Aneurysma-Erkrankte“ (patient association). Distinct from our paper submitted in European Radiology, it was a single-reader-only comparison of MRT and DSA in terms of visibility and grading of intracranial dural fistulas. The collective included different types of fistulas (lateral type and carotid-cavernosus-fistulae). It did not provide any detailed aspects on therapy planning (luminal patency, flow direction, cervical drainage, best method, etc.) and was not published as an original research paper. Methodology: retrospective, not applicable, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ertl, L., Brückmann, H., Kunz, M. et al. Assessment and treatment planning of lateral intracranial dural arteriovenous fistulas in 3 T MRI and DSA: A detailed analysis under consideration of time-resolved imaging of contrast kinetics (TRICKS) and ce-MRA sequences. Eur Radiol 26, 4284–4292 (2016). https://doi.org/10.1007/s00330-016-4335-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4335-1