Abstract
Objectives
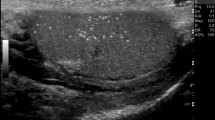
The increasing detection of small testicular lesions by ultrasound (US) in adults can lead to unnecessary orchiectomies. This article describes their nature, reviews the available literature on this subject and illustrates some classical lesions. We also suggest recommendations to help characterization and management.
Methods
The ESUR scrotal imaging subcommittee searched for original and review articles published before May 2015 using the Pubmed and Medline databases. Key words used were ‘testicular ultrasound’, ‘contrast-enhanced sonography’, ‘sonoelastography’, ‘magnetic resonance imaging’, ‘testis-sparing surgery’, ‘testis imaging’, ‘Leydig cell tumour’, ‘testicular cyst’. Consensus was obtained amongst the members of the subcommittee, urologist and medical oncologist.
Results
Simple cysts are frequent and benign, and do not require follow up or surgery. Incidentally discovered small solid testicular lesions detected are benign in up to 80 %, with Leydig cell tumours being the most frequent. However, the presence of microliths, macrocalcifications and hypoechoic areas surrounding the nodule are findings suggestive of malignant disease.
Conclusion
Asymptomatic small testicular lesions found on ultrasound are mainly benign, but findings such as microliths or hypoechoic regions surrounding the nodules may indicate malignancy. Colour Doppler US remains the basic examination for characterization. The role of newer imaging modalities in characterization is evolving.
Key points
• Characterization of testicular lesions is primarily based on US examination.
• The role of MRI, sonoelastography, contrast-enhanced ultrasound is evolving.
• Most small non-palpable testicular lesions seen on ultrasound are benign simple cysts.
• Leydig cell tumours are the most frequent benign lesions.
• Associated findings like microliths or hypoechoic regions may indicate malignancy.













Similar content being viewed by others

Abbreviations
- US:
-
Ultrasound
- MRI:
-
Magnetic resonance imaging :
- CEUS:
-
Contrast-enhanced ultrasound
- ESUR:
-
European Society of Urogenital Radiology
- WI:
-
Weighted image
- ADC:
-
Apparent diffusion coefficient
References
Woodward PJ, Sohaey R, O’Donoghue MJ, Green DE (2002) From the archives of the AFIP: tumors and tumorlike lesions of the testis: radiologic-pathologic correlation. Radiogr Rev Publ Radiol Soc N Am Inc 22:189–216
Brunocilla E, Gentile G, Schiavina R et al (2013) Testis-sparing Surgery for the Conservative Management of Small Testicular Masses: An Update. Anticancer Res 33:5205–5210
Dieckmann K-P, Frey U, Lock G (2013) Contemporary diagnostic work-up of testicular germ cell tumours. Nat Rev Urol 10:703–712
Dogra VS, Gottlieb RH, Oka M, Rubens DJ (2003) Sonography of the scrotum. Radiology 227:18–36
Bhatt S, Jafri SZH, Wasserman N, Dogra VS (2011) Imaging of non-neoplastic intratesticular masses. Diagn Interv Radiol Ank Turk 17:52–63
Avci A, Erol B, Eken C, Ozgok Y (2008) Nine cases of nonpalpable testicular mass: an incidental finding in a large scale ultrasonography survey. Int J Urol Off J Jpn Urol Assoc 15:833–836
Connolly SS, D’Arcy FT, Gough N et al (2006) Carefully selected intratesticular lesions can be safely managed with serial ultrasonography. BJU Int 98:1005–1007, discussion 1007
Toren PJ, Roberts M, Lecker I et al (2010) Small incidentally discovered testicular masses in infertile men-is active surveillance the new standard of care? J Urol 183:1373–1377
Isidori AM, Pozza C, Gianfrilli D, et al. (2014) Differential Diagnosis of Nonpalpable Testicular Lesions: Qualitative and Quantitative Contrast-enhanced US of Benign and Malignant Testicular Tumors. Radiology 273:606–619
Martínez-Berganza MT, Sarría L, Cozcolluela R et al (1998) Cysts of the tunica albuginea: sonographic appearance. AJR Am J Roentgenol 170:183–185
Leung ML, Gooding GA, Williams RD (1984) High-resolution sonography of scrotal contents in asymptomatic subjects. AJR Am J Roentgenol 143:161–164
Nistal M, Paniagua R (2008) Non-neoplastic disease of the testis. In: Bostwick D, Liang C (eds) Urologic Surgical Pathology, 2nd edn. Edinburgh, Mosby Elsevier, p 622–623
Zhang C, Berney DM, Hirsch MS et al (2013) Evidence supporting the existence of benign teratomas of the postpubertal testis: a clinical, histopathologic, and molecular genetic analysis of 25 cases. Am J Surg Pathol 37:827–835
Giannarini G, Dieckmann K-P, Albers P et al (2010) Organ-sparing surgery for adult testicular tumours: a systematic review of the literature. Eur Urol 57:780–790
Eifler JB Jr, King P, Schlegel PN (2008) Incidental testicular lesions found during infertility evaluation are usually benign and may be managed conservatively. J Urol 180:261–264, discussion 265
Westlander G, Ekerhovd E, Granberg S et al (2001) Testicular ultrasonography and extended chromosome analysis in men with nonmosaic Klinefelter syndrome: a prospective study of possible predictive factors for successful sperm recovery. Fertil Steril 75:1102–1105
Ekerhovd E, Westlander G (2002) Testicular sonography in men with Klinefelter syndrome shows irregular echogenicity and blood flow of high resistance. J Assist Reprod Genet 19:517–522
Rock A, Marcelli F, Robin G et al (2014) [Clinical and paraclinical features of Klinefelter syndrome consulting for male infertility.]. Progres En Urol J Assoc Francaise Urol Soc Francaise Urol 24:757–763
Accardo G, Vallone G, Esposito D, et al. (2014) Testicular parenchymal abnormalities in Klinefelter syndrome: a question of cancer? Examination of 40 consecutive patients. Asian J Androl 17:154-158
Kim I, Young RH, Scully RE (1985) Leydig cell tumors of the testis. A clinicopathological analysis of 40 cases and review of the literature. Am J Surg Pathol 9:177–192
Silberstein JL, Bazzi WM, Vertosick E et al (2014) Clinical Outcomes for Local and Metastatic Testicular Sex Cord-Stromal Tumors. J Urol 192:415–419
Nicolai N, Necchi A, Raggi D et al (2015) Clinical Outcome in Testicular Sex Cord Stromal Tumors: Testis Sparing vs Radical Orchiectomy and Management of Advanced Disease. Urology 85:402–406
de Wit R, Fizazi K (2006) Controversies in the management of clinical stage I testis cancer. J Clin Oncol Off J Am Soc Clin Oncol 24:5482–5492
Kim W, Rosen MA, Langer JE et al (2007) US MR imaging correlation in pathologic conditions of the scrotum. Radiogr Rev Publ Radiol Soc N Am Inc 27:1239–1253
Coursey Moreno C, Small WC, Camacho JC et al (2015) Testicular tumors: what radiologists need to know-differential diagnosis, staging, and management. Radiogr Rev Publ Radiol Soc N Am Inc 35:400–415
Bertolotto M, Derchi LE, Secil M et al (2015) Grayscale and color Doppler features of testicular lymphoma. J Ultrasound Med Off J Am Inst Ultrasound Med 34:1139–1145
Dogra VS, Gottlieb RH, Rubens DJ, Liao L (2001) Benign intratesticular cystic lesions: US features. Radiogr Rev Publ Radiol Soc N Am Inc 21(Spec No):S273–S281
McDonald MW, Reed AB, Tran PT, Evans LA (2012) Testicular tumor ultrasound characteristics and association with histopathology. Urol Int 89:196–202
Richenberg J, Belfield J, Ramchandani P et al (2015) Testicular microlithiasis imaging and follow-up: guidelines of the ESUR scrotal imaging subcommittee. Eur Radiol 25:323–330
Miacola C, Colamonico O, Bettocchi C et al (2014) Burned-out in a mixed germ cell tumor of the testis: The problem of pT0. Case report. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol Assoc Ric Urol 86:389–390
Tasu J-P, Faye N, Eschwege P et al (2003) Imaging of burned-out testis tumor: five new cases and review of the literature. J Ultrasound Med Off J Am Inst Ultrasound Med 22:515–521
Balalaa N, Selman M, Hassen W (2011) Burned-out testicular tumor: a case report. Case Rep Oncol 4:12–15
Philips S, Nagar A, Dighe M et al (2012) Benign non-cystic scrotal tumors and pseudotumors. Acta Radiol Stockh Swed 1987 53:102–111
Maizlin ZV, Belenky A, Kunichezky M et al (2004) Leydig cell tumors of the testis: gray scale and color Doppler sonographic appearance. J Ultrasound Med Off J Am Inst Ultrasound Med 23:959–964
Lock G, Schröder C, Schmidt C, et al. (2014) Contrast-Enhanced Ultrasound and Real-Time Elastography for the Diagnosis of Benign Leydig Cell Tumors of the Testis - A Single Center Report on 13 Cases. Ultraschall Med Stuttg Ger 1980. doi: 10.1055/s-0034-1385038
Patel K, Sellars ME, Clarke JL, Sidhu PS (2012) Features of Testicular Epidermoid Cysts on Contrast-Enhanced Sonography and Real-time Tissue Elastography. J Ultrasound Med 31:115–122
Lung PFC, Jaffer OS, Sellars ME et al (2012) Contrast-enhanced ultrasound in the evaluation of focal testicular complications secondary to epididymitis. AJR Am J Roentgenol 199:W345–W354
Bertolotto M, Derchi LE, Sidhu PS et al (2011) Acute segmental testicular infarction at contrast-enhanced ultrasound: early features and changes during follow-up. AJR Am J Roentgenol 196:834–841
Huang DY, Sidhu PS (2012) Focal testicular lesions: colour Doppler ultrasound, contrast-enhanced ultrasound and tissue elastography as adjuvants to the diagnosis. Br J Radiol 85(Spec No 1):S41–S53
Aigner F, De Zordo T, Pallwein-Prettner L et al (2012) Real-time sonoelastography for the evaluation of testicular lesions. Radiology 263:584–589
Goddi A, Sacchi A, Magistretti G et al (2012) Real-time tissue elastography for testicular lesion assessment. Eur Radiol 22:721–730
Pastore AL, Palleschi G, Maceroni P et al (2014) Correlation between semiquantitative sonoelastography and immunohistochemistry in the evaluation of testicular focal lesions. Cancer Imaging Off Publ Int Cancer Imaging Soc 14:29
Correas JM, Drakonakis E, Isidori AM et al (2013) Update on ultrasound elastography: miscellanea. Prostate, testicle, musculo-skeletal. Eur J Radiol 82:1904–1912
Patel MD, Patel BM (2007) Sonographic and magnetic resonance imaging appearance of a burned-out testicular germ cell neoplasm. J Ultrasound Med Off J Am Inst Ultrasound Med 26:143–146
Fernández GC, Tardáguila F, Rivas C et al (2004) MRI in the diagnosis of testicular Leydig cell tumour. Br J Radiol 77:521–524
Tsili AC, Argyropoulou MI, Astrakas LG et al (2013) Dynamic contrast-enhanced subtraction MRI for characterizing intratesticular mass lesions. AJR Am J Roentgenol 200:578–585
Manganaro L, Vinci V, Pozza C, et al. (2015) A prospective study on contrast-enhanced magnetic resonance imaging of testicular lesions: distinctive features of Leydig cell tumours. Eur Radiol (in press)
Tsili AC, Argyropoulou MI, Giannakis D et al (2012) Diffusion-weighted MR imaging of normal and abnormal scrotum: preliminary results. Asian J Androl 14:649–654
Tsili AC, Sylakos A, Ntorkou A et al (2015) Apparent diffusion coefficient values and dynamic contrast enhancement patterns in differentiating seminomas from nonseminomatous testicular neoplasms. Eur J Radiol. Eur J Radiol 84:1219–1226
Al-Agha OM, Axiotis CA (2007) An in-depth look at Leydig cell tumor of the testis. Arch Pathol Lab Med 131:311–317
Shaida N, Berman LH (2012) Percutaneous testicular biopsy for indeterminate testicular lesions. Br J Radiol 85:S54–S58
Acknowledgments
The scientific guarantor of this publication is Jonathan Richenberg. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. This manuscript is a review but institutional review board approval was obtained to publish radiological data. Written informed consent was waived by the institutional review board. Methodology: review. We thank Vincent Izard, our guest specialized urologist for his contribution. We thank Mustafa Cecil, Pietro Pavlica, Michal Studniarek for their active participation in the group. We thank Valentine Sallerin for her initial English revision.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rocher, L., Ramchandani, P., Belfield, J. et al. Incidentally detected non-palpable testicular tumours in adults at scrotal ultrasound: impact of radiological findings on management Radiologic review and recommendations of the ESUR scrotal imaging subcommittee. Eur Radiol 26, 2268–2278 (2016). https://doi.org/10.1007/s00330-015-4059-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4059-7