Abstract
Objectives
To evaluate the clinical efficacy of magnetic resonance-guided focused ultrasound surgery in a Mexican mestizo population.
Methods
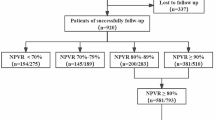
This retrospective study included 159 women (mean age 37 ± 6.4 years, range 22–53 years) from 2008 to 2010. Two hundred sixty-eight symptomatic uterine fibroids were treated using MR-guided focused ultrasound surgery. Parameters included initial perfused volume, final perfused volume, non-perfused volume (NPV), and treated volume ratio (TVR). Follow-up up to 15 months assessed treatment efficacy and symptomatic relief. Non-parametric statistics and the Kaplan-Meier method were performed.
Results
T2-weighted hypointense fibroids showed a frequency of 93.6 %; isointense and hyperintense fibroids had frequencies of 5.60 and 1.1 %. There was a negative correlation between NPV and age (r = -0.083, p = 0.307) and treatment time (r = -0.253, p = 0.001). Median TVR was 96.0 % in small fibroids and 76.5 % in large fibroids. Involution of 50 % and 80 % was achieved at months 6–7 and month 11, respectively. Relief of symptoms was significant (p < 0.05).
Conclusions
Our data show that higher TVR attained immediately post-treatment of MRgFUS favours higher involution percentages at follow-up; however, careful patient selection and use of pretreatment imaging are important components for predicting success using MR-guided focused ultrasound surgery.
Key Points
• Type 1 fibroids were the most common (93.2 %).
• Age and treated volume were not correlated (r s = -0.215, p = 0.165).
• Small fibroids achieved a higher treated volume than large (96.0 % vs. 76.5 %).
• A 50 % involution was achieved at 6-month follow-up for type-1 fibroid.
• A decrease of 80 % was reached at 11 months for type-1 fibroids.





Similar content being viewed by others
References
Khan AT, Shehmar M, Gupta JK (2014) Uterine fibroids: current perspectives. Int J Womens Health 6:95–114
Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM (2003) High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol 188:100–107
Hanstede MM, Tempany CM, Stewart EA (2007) Focused ultrasound surgery of intramural leiomyomas may facilitate fertility: a case report. Fertil Steril 88:e495–e497
Funaki K, Fukunishi H, Funaki T, Sawada K, Kaji Y, Maruo T (2007) Magnetic resonance-guided focused ultrasound surgery for uterine fibroids: relationship between the therapeutic effects and signal intensity of preexisting T2-weighted magnetic resonance images. Am J Obstet Gynecol 196:e181–e186
Himabindu Y, Sriharibabu M, Nyapathy V, Mishra A (2014) Early evaluation of magnetic resonance imaging guided focused ultrasound sonication in the treatment of uterine fibroids. Indian J Med Res 139:267–272
van der Kooij SM, Ankum WM, Hehenkamp WJ (2012) Review of nonsurgical/minimally invasive treatments for uterine fibroids. Curr Opin Obstet Gynecol 24:368–375
Stewart EA, Gedroyc WM, Tempany CM et al (2003) Focused ultrasound treatment of uterine fibroid tumors: safety and feasibility of a noninvasive thermoablative technique. Am J Obstet Gynecol 189:48–54
Tempany CM, Stewart EA, McDannold N, Quade BJ, Jolesz FA, Hynynen K (2003) MR imaging-guided focused ultrasound surgery of uterine leiomyomas: a feasibility study. Radiology 226:897–905
Hindley J, Gedroyc WM, Regan L et al (2004) MRI guidance of focused ultrasound therapy of uterine fibroids: early results. AJR Am J Roentgenol 183:1713–1719
Stewart EA, Rabinovici J, Tempany CM et al (2006) Clinical outcomes of focused ultrasound surgery for the treatment of uterine fibroids. Fertil Steril 85:22–29
Fennessy FM, Tempany CM, McDannold NJ et al (2007) Uterine leiomyomas: MR imaging-guided focused ultrasound surgery–results of different treatment protocols. Radiology 243:885–893
Leslie TA, Kennedy JE (2007) High intensity focused ultrasound in the treatment of abdominal and gynaecological diseases. Int J Hyperth 23:173–182
Vazquez-Lamadrid J, Fernandez-de Lara Y, Carrasco-Choque A, Romero-Trejo C, Cosme-Labarthe J, Roldan-Valadez E (2011) Principles and technique of magnetic resonance guided focused ultrasound surgery (MRgFUS) in the treatment of uterine fibroids. Gac Med Mex 147:333–341
Spies JB, Coyne K, Guaou Guaou N, Boyle D, Skyrnarz-Murphy K, Gonzalves SM (2002) The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol 99:290–300
Machtinger R, Fennessy FM, Stewart EA, Missmer SA, Correia KF, Tempany CM (2013) MR-guided focused ultrasound (MRgFUS) is effective for the distinct pattern of uterine fibroids seen in African-American women: data from phase III/IV, non-randomized, multicenter clinical trials. J Ther Ultrasound 1:23
Rabinovici J, Inbar Y, Revel A et al (2007) Clinical improvement and shrinkage of uterine fibroids after thermal ablation by magnetic resonance-guided focused ultrasound surgery. Ultrasound Obstet Gynecol 30:771–777
Pallant J (2011) Correlation. In: Pallant J (ed) SPSS survival manual, 4th edn. Allen & Unwin, Crows Nest, pp 128–142
Pallant J (2011) Non-parametric statistics. In: Pallant J (ed) SPSS survival manual, 4th edn. Allen & Unwin, Crows Nest, pp 213–238
Stel VS, Dekker FW, Tripepi G, Zoccali C, Jager KJ (2011) Survival analysis I: the Kaplan-Meier method. Nephron Clin Pract 119:c83–c88
Ingelsson E, Lundholm C, Johansson AL, Altman D (2011) Hysterectomy and risk of cardiovascular disease: a population-based cohort study. Eur Heart J 32:745–750
Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F (2002) Accuracy of magnetic resonance imaging and transvaginal ultrasonography in the diagnosis, mapping, and measurement of uterine myomas. Am J Obstet Gynecol 186:409–415
Byun JY, Kim SE, Choi BG, Ko GY, Jung SE, Choi KH (1999) Diffuse and focal adenomyosis: MR imaging findings. Radiographics 19:S161–170
Kim HS, Baik JH, Pham LD, Jacobs MA (2011) MR-guided high-intensity focused ultrasound treatment for symptomatic uterine leiomyomata: long-term outcomes. Acad Radiol 18:970–976
Funaki K, Fukunishi H, Sawada K (2009) Clinical outcomes of magnetic resonance-guided focused ultrasound surgery for uterine myomas: 24-month follow-up. Ultrasound Obstet Gynecol 34:584–589
Gorny KR, Woodrum DA, Brown DL et al (2011) Magnetic resonance-guided focused ultrasound of uterine leiomyomas: review of a 12-month outcome of 130 clinical patients. J Vasc Interv Radiol 22:857–864
Yoon SW, Cha SH, Ji YG, Kim HC, Lee MH, Cho JH (2013) Magnetic resonance imaging-guided focused ultrasound surgery for symptomatic uterine fibroids: estimation of treatment efficacy using thermal dose calculations. Eur J Obstet Gynecol Reprod Biol 169:304–308
Mindjuk I, Trumm CG, Herzog P, Stahl R, Matzko M (2014) MRI predictors of clinical success in MR-guided focused ultrasound (MRgFUS) treatments of uterine fibroids: results from a single centre. Eur Radiol. doi:10.1007/s00330-014-3538-6
Machtinger R, Inbar Y, Cohen-Eylon S, Admon D, Alagem-Mizrachi A, Rabinovici J (2012) MR-guided focus ultrasound (MRgFUS) for symptomatic uterine fibroids: predictors of treatment success. Hum Reprod 27:3425–3431
Okada A, Morita Y, Fukunishi H, Takeichi K, Murakami T (2009) Non-invasive magnetic resonance-guided focused ultrasound treatment of uterine fibroids in a large Japanese population: impact of the learning curve on patient outcome. Ultrasound Obstet Gynecol 34:579–583
Lenard ZM, McDannold NJ, Fennessy FM et al (2008) Uterine leiomyomas: MR imaging-guided focused ultrasound surgery–imaging predictors of success. Radiology 249:187–194
Yamashita Y, Torashima M, Takahashi M et al (1993) Hyperintense uterine leiomyoma at T2-weighted MR imaging: differentiation with dynamic enhanced MR imaging and clinical implications. Radiology 189:721–725
Smart OC, Hindley JT, Regan L, Gedroyc WG (2006) Gonadotrophin-releasing hormone and magnetic-resonance-guided ultrasound surgery for uterine leiomyomata. Obstet Gynecol 108:49–54
Hudson SB, Stewart EA (2008) Magnetic resonance-guided focused ultrasound surgery. Clin Obstet Gynecol 51:159–166
Tempany CM (2007) From the RSNA refresher courses: image-guided thermal therapy of uterine fibroids. Radiographics 27:1819–1826
Acknowledgments
The scientific guarantor of this publication is Ernesto Roldan-Valadez. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.This article was supported in part by Medica Sur Clinic and Foundation.
Ana Luz Carrasco-Choque, MD, was enrolled as clinical fellow of the whole-body MRI program during 2009-2010. Ingrid Vivas-Bonilla, MD, was attending radiologist at the MRI unit from 2001 to 2009. Cecilia Romero-Trejo, MD, was attending radiologist at the MRI unit from 2005 to 2010.
Antonio R. Villa MD, PhD, provided statistical advice for the preparation of this manuscript.
One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Methodology: retrospective.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carrasco-Choque, A.L., Lara, Y.Fd., Vivas-Bonilla, I. et al. Perfusion volume correlates, percentage of involution, and clinical efficacy at diverse follow-up survey times after MR-guided focused ultrasound surgery in uterine fibroids: first report in a Mexican mestizo population. Eur Radiol 25, 2905–2912 (2015). https://doi.org/10.1007/s00330-015-3707-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3707-2