Abstract
Purpose
Within-patient comparison of the enhancement patterns of normal liver parenchyma after gadobutrol and gadoxetate disodium, with emphasis on the start of hepatocytic uptake of gadoxetate disodium.
Materials and methods
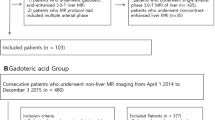
Twenty-one patients (12 female, 9 male) without chronic liver disease underwent 1.5-T contrast-enhanced MRI twice, once with an extracellular contrast agent (gadobutrol) and once with a hepatospecific agent (gadoxetate disodium), using a T1-weighted keyhole sequence. Fifteen whole-liver datasets were acquired up to 5 min for both contrast agents and two additional datasets, up to 20 min, for gadoxetate. Signal intensities (SI) of the parenchyma, aorta and portal vein were measured and analysed relative to pre-contrast parenchymal SI.
Results
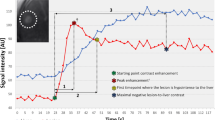
After gadoxetate, in 29 % of the patients the parenchymal SI decreased by ≥5 % after the initial vascular-phase-induced peak, while in the other 71 % the parenchymal SI remained stable or gradually increased until up to 20 min after the initial peak. The hepatocytic gadoxetate uptake started at a mean of 37.8 s (SD 14.7 s) and not later than 76 s after left ventricle enhancement.
Conclusion
Parenchymal enhancement due to hepatocytic uptake of gadoxetate can start as early as in the late arterial phase. This may confound the assessment of lesion appearance as compared to extracellular contrast such as gadobutrol.
Key Points
• Gadoxetate-enhanced liver MRI results in early enhancement of normal parenchyma in patients
• The start of the hepatobiliary phase coincides with the late arterial phase
• This may confound the assessment of lesion appearance compared to extracellular contrast
• Different parenchymal enhancement patterns after gadoxetate were found for normal parenchyma







Similar content being viewed by others
Abbreviations
- DCE:
-
dynamic contrast enhanced
- MRI:
-
magnetic resonance imaging
- SENSE:
-
sensitivity encoding
- TFE:
-
turbo field echo
- DWI:
-
diffusion-weighted imaging
- 4D-THRIVE:
-
four-dimensional T1-weighted high-resolution imaging with volume examination
- ROI:
-
region of interest
- SI:
-
signal intensity
- SD:
-
standard deviation
- LOA:
-
limits of agreement
- CI:
-
confidence interval
References
Feuerlein S, Gupta RT, Boll DT, Merkle EM (2012) Hepatocellular MR contrast agents: enhancement characteristics of liver parenchyma and portal vein after administration of gadoxetic acid in comparison to gadobenate dimeglumine. Eur J Radiol 81(9):2037–2041, Epub 2011/07/02
Cruite I, Schroeder M, Merkle EM, Sirlin CB (2010) Gadoxetate disodium-enhanced MRI of the liver: part 2, protocol optimization and lesion appearance in the cirrhotic liver. AJR Am J Roentgenol 195(1):29–41, Epub 2010/06/23
Purysko AS, Remer EM, Veniero JC (2011) Focal liver lesion detection and characterization with GD-EOB-DTPA. Clin Radiol 66(7):673–684, Epub 2011/04/29
Campos JT, Sirlin CB, Choi JY (2012) Focal hepatic lesions in Gd-EOB-DTPA enhanced MRI: the atlas. Insights Imaging 3(5):451–474, Epub 2012/06/16
Doo KW, Lee CH, Choi JW, Lee J, Kim KA, Park CM (2009) "Pseudo washout" sign in high-flow hepatic hemangioma on gadoxetic acid contrast-enhanced MRI mimicking hypervascular tumor. AJR Am J Roentgenol 193(6):W490–W496, Epub 2009/11/26
Van Kessel CS (2010) Online trial info: PRIDE-study (PRImovist enhanced mri for Detection and Evaluation of focal liver lesions). www.trialregister.nl/: Nederlands Trial Register; Available from: http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=1529
Beck GM, De Becker J, Jones AC, von Falkenhausen M, Willinek WA, Gieseke J (2008) Contrast-enhanced timing robust acquisition order with a preparation of the longitudinal signal component (CENTRA plus) for 3D contrast-enhanced abdominal imaging. J Magn Reson Imaging JMRI 27(6):1461–1467, Epub 2008/05/28
Coenegrachts K, Ghekiere J, Denolin V, Gabriele B, Herigault G, Haspeslagh M et al (2010) Perfusion maps of the whole liver based on high temporal and spatial resolution contrast-enhanced MRI (4D THRIVE): feasibility and initial results in focal liver lesions. Eur J Radiol 74(3):529–535, Epub 2009/04/21
Zizka J, Klzo L, Ferda J, Mrklovsky M, Bukac J (2007) Dynamic and delayed contrast enhancement in upper abdominal MRI studies: comparison of gadoxetic acid and gadobutrol. Eur J Radiol 62(2):186–191, Epub 2007/03/21
Tamada T, Ito K, Sone T, Yamamoto A, Yoshida K, Kakuba K et al (2009) Dynamic contrast-enhanced magnetic resonance imaging of abdominal solid organ and major vessel: comparison of enhancement effect between Gd-EOB-DTPA and Gd-DTPA. J Magn Reson Imaging JMRI 29(3):636–640, Epub 2009/02/27
Zech CJ, Vos B, Nordell A, Urich M, Blomqvist L, Breuer J et al (2009) Vascular enhancement in early dynamic liver MR imaging in an animal model: comparison of two injection regimen and two different doses Gd-EOB-DTPA (gadoxetic acid) with standard Gd-DTPA. Investig Radiol 44(6):305–310, Epub 2009/05/23
Kuhn JP, Hegenscheid K, Siegmund W, Froehlich CP, Hosten N, Puls R (2009) Normal dynamic MRI enhancement patterns of the upper abdominal organs: gadoxetic acid compared with gadobutrol. AJR Am J Roentgenol 193(5):1318–1323, Epub 2009/10/22
Reimer P, Rummeny EJ, Daldrup HE, Hesse T, Balzer T, Tombach B et al (1997) Enhancement characteristics of liver metastases, hepatocellular carcinomas, and hemangiomas with Gd-EOB-DTPA: preliminary results with dynamic MR imaging. Eur Radiol 7(2):275–280, Epub 1997/01/01
Dahlqvist Leinhard O, Dahlstrom N, Kihlberg J, Sandstrom P, Brismar TB, Smedby O et al (2012) Quantifying differences in hepatic uptake of the liver specific contrast agents Gd-EOB-DTPA and Gd-BOPTA: a pilot study. Eur Radiol 22(3):642–653, Epub 2011/10/11
Frydrychowicz A, Nagle SK, D'Souza SL, Vigen KK, Reeder SB (2011) Optimized high-resolution contrast-enhanced hepatobiliary imaging at 3 tesla: a cross-over comparison of gadobenate dimeglumine and gadoxetic acid. J Magn Reson Imaging JMRI 34(3):585–594, Epub 2011/07/14
Motosugi U, Ichikawa T, Tominaga L, Sou H, Sano K, Ichikawa S et al (2009) Delay before the hepatocyte phase of Gd-EOB-DTPA-enhanced MR imaging: is it possible to shorten the examination time? Eur Radiol 19(11):2623–2629, Epub 2009/05/28
van Kessel CS, Veldhuis WB, van den Bosch MA, van Leeuwen MS (2012) MR liver imaging with Gd-EOB-DTPA: a delay time of 10 minutes is sufficient for lesion characterisation. Eur Radiol 22(10):2153–2160, Epub 2012/05/31
Goshima S, Kanematsu M, Watanabe H, Kondo H, Mizuno N, Kawada H et al (2011) Gadoxetate disodium-enhanced MR imaging: differentiation between early-enhancing non-tumorous lesions and hypervascular hepatocellular carcinomas. Eur J Radiol 79(2):e108–e112, Epub 2011/05/20
Rohrer M, Bauer H, Mintorovitch J, Requardt M, Weinmann HJ (2005) Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Investig Radiol 40(11):715–724, Epub 2005/10/19
Ringe KI, Husarik DB, Sirlin CB, Merkle EM (2010) Gadoxetate disodium-enhanced MRI of the liver: part 1, protocol optimization and lesion appearance in the noncirrhotic liver. AJR Am J Roentgenol 195(1):13–28, Epub 2010/06/23
Lee NK, Kim S, Lee JW, Lee SH, Kang DH, Kim GH et al (2009) Biliary MR imaging with Gd-EOB-DTPA and its clinical applications. Radiographics 29(6):1707–1724, Epub 2009/12/05
Vogl TJ, Kummel S, Hammerstingl R, Schellenbeck M, Schumacher G, Balzer T et al (1996) Liver tumors: comparison of MR imaging with Gd-EOB-DTPA and Gd-DTPA. Radiology 200(1):59–67, Epub 1996/07/01
Chung SH, Kim MJ, Choi JY, Hong HS (2010) Comparison of two different injection rates of gadoxetic acid for arterial phase MRI of the liver. J Magn Reson Imaging JMRI 31(2):365–372, Epub 2010/01/26
Tamada T, Ito K, Yoshida K, Kanki A, Higaki A, Tanimoto D et al (2011) Comparison of three different injection methods for arterial phase of Gd-EOB-DTPA enhanced MR imaging of the liver. Eur J Radiol 80(3):e284–e288, Epub 2011/02/08
Schmid-Tannwald C, Herrmann K, Oto A, Panteleon A, Reiser M, Zech C (2012) Optimization of the dynamic, Gd-EOB-DTPA-enhanced MRI of the liver: the effect of the injection rate. Acta Radiol 53(9):961–965, Epub 2012/10/02
Acknowledgments
The scientific guarantor of this publication is Dr. M.S. van Leeuwen. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this article. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, experimental study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schalkx, H.J., van Stralen, M., Coenegrachts, K. et al. Liver perfusion in dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI): comparison of enhancement in Gd-BT-DO3A and Gd-EOB-DTPA in normal liver parenchyma. Eur Radiol 24, 2146–2156 (2014). https://doi.org/10.1007/s00330-014-3275-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3275-x