Abstract
Purpose
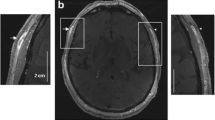
To assess deep temporal artery and temporalis muscle involvement in patients with giant cell arteritis (GCA).
Material and methods
Ninety-nine patients who received magnetic resonance imaging (MRI) and superficial temporal artery biopsy (TAB) were included in this study. Patients with positive TAB (n = 61) were defined as GCA patients, those with negative TAB (n = 38) as the GCA-negative reference group. Contrast-enhanced T1w-images were acquired utilizing 1.5 T and 3 T MRI. Two radiologists assessed the images. Mural contrast-hyperenhancement and wall thickening of the deep temporal artery and hyperenhancement of the muscle were defined as inflammation. MRI results were correlated with jaw claudication in 70 patients.
Results
The two observers found temporalis muscle involvement in 19.7 % (n = 12) and 21.3 % (n = 13) of GCA patients. It occurred bilaterally in 100 %. Specificities were 92/97 % and sensitivities were 20/21 %. Deep temporal artery involvement was found in 34.4 % (n = 21) and 49.2 % (n = 30) and occurred bilaterally in 80/90.5 %. Specificities were 84/95 % and sensitivities were 34/49 %. Both structures were affected simultaneously in 18/21.3 %. Jaw claudication correlated moderately with inflammation of the temporalis muscle (r = 0.31; p < 0.05) and the deep temporal artery (r = 0.38; p = 0.01).
Conclusion
MRI visualizes changes in the temporalis muscle and the deep temporal artery in GCA. Moderate correlation of clinical symptoms with MRI results was observed.
Key Points
• Approximately 20 % of GCA patients presented with temporalis muscle inflammation.
• A total of 34-49 % of GCA patients presented with vasculitis of the deep temporal artery.
• In approximately 20 % of GCA patients, both structures were simultaneously involved.
• Involvement of both structures correlated moderately with presence of jaw claudication.
• MRI is a suitable tool for the assessment of vasculitis and muscle inflammation.


Similar content being viewed by others
References
Salvarani C, Cantini F, Boiardi L, Hunder GG (2002) Polymyalgia rheumatica and giant-cell arteritis. N Engl J Med 347:261–271. doi:10.1056/NEJMra011913
Salvarani C, Crowson CS, O’Fallon WM et al (2004) Reappraisal of the epidemiology of giant cell arteritis in Olmsted County, Minnesota, over a fifty-year period. Arthritis Rheum 51:264–268. doi:10.1002/art.20227
González-Gay MA, García-Porrúa C, Llorca J et al (2000) Visual manifestations of giant cell arteritis. Trends and clinical spectrum in 161 patients. Medicine (Baltimore) 79:283–292
Wenkel H (2001) Bilateral amaurosis in 11 patients with giant cell arteritis confirmed by arterial biopsy. Klin Monbl Augenheilkd 218:658–661. doi:10.1055/s-2001-18387
Fitzgerald AJ, Ironside JW, Summers DM et al (2010) Two cases of recurrent stroke in treated giant cell arteritis: diagnostic and therapeutic dilemmas. J Clin Rheumatol 16:225–228. doi:10.1097/RHU.0b013e3181e9a338
Valesky EM, Wahle M, Vranes S et al (2012) Bitemporal scalp necrosis : a very rare manifestation of giant cell arteritis. Z Rheumatol 71:806–809. doi:10.1007/s00393-012-1009-5
González-Gay MA, Blanco R, Rodríguez-Valverde V et al (1998) Permanent visual loss and cerebrovascular accidents in giant cell arteritis: predictors and response to treatment. Arthritis Rheum 41:1497–1504. doi:10.1002/1529-0131(199808)41:8<1497::AID-ART22>3.0.CO;2-Z
Smetana GW, Shmerling RH (2002) Does this patient have temporal arteritis? JAMA 287:92–101
Bley TA, Wieben O, Uhl M et al (2005) High-resolution MRI in giant cell arteritis: imaging of the wall of the superficial temporal artery. AJR Am J Roentgenol 184:283–287
Bley TA, Uhl M, Markl M et al (2007) MRI in giant cell (temporal) arteritis. Röfo 179:703–711. doi:10.1055/s-2007-963123
Bley TA, Weiben O, Uhl M et al (2005) Assessment of the cranial involvement pattern of giant cell arteritis with 3 T magnetic resonance imaging. Arthritis Rheum 52:2470–2477. doi:10.1002/art.21226
Hunder GG, Bloch DA, Michel BA et al (1990) The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 33:1122–1128
Geiger J, Ness T, Uhl M et al (2009) Involvement of the ophthalmic artery in giant cell arteritis visualized by 3 T MRI. Rheumatology (Oxford) 48:537–541. doi:10.1093/rheumatology/kep011
Bley TA, Uhl M, Carew J et al (2007) Diagnostic value of high-resolution MR imaging in giant cell arteritis. AJNR Am J Neuroradiol 28:1722–1727. doi:10.3174/ajnr.A0638
Hauenstein C, Reinhard M, Geiger J et al (2012) Effects of early corticosteroid treatment on magnetic resonance imaging and ultrasonography findings in giant cell arteritis. Rheumatology (Oxford) 51:1999–2003. doi:10.1093/rheumatology/kes153
Imai N, Kuroda R, Konishi T et al (2011) Giant cell arteritis: clinical features of patients visiting a headache clinic in Japan. Intern Med 50:1679–1682
Kleinegger CL, Lilly GE (1999) Cranial arteritis: a medical emergency with orofacial manifestations. J Am Dent Assoc 130:1203–1209
Cheung LK (1996) The blood supply of the human temporalis muscle: a vascular corrosion cast study. J Anat 189:431–438
Padovano I, Pazzola G, Pipitone N, et al (2013) Anterior ischaemic optic neuropathy in eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome): a case report and review of the literature. Clin Exp Rheumatol
Kumar B, Toney DE, Alikhan M, Lohr KM (2013) Giant cell arteritis presenting as depressed mood and headache in an elderly patient. J Clin Rheumatol 19:405–406. doi:10.1097/RHU.0b013e3182a701e8
Slemp SN, Martin SE, Burgett RA, Hattab EM (2013) Giant cell arteritis presenting with uveitis. Ocul Immunol Inflamm. doi:10.3109/09273948.2013.849351
Klein RG, Campbell RJ, Hunder GG, Carney JA (1976) Skip lesions in temporal arteritis. Mayo Clin Proc 51:504–510
Goodman BW, Shepard FA (1983) Jaw claudication. Its value as a diagnostic clue. Postgrad Med 73:177–183
Acknowledgements
The scientific guarantor of this publication is Professor Dr. med. Thorsten A. Bley. The authors of this manuscript declare relationships with the following companies: Thorsten Bley: Payment for lectures (past) - Bayer, Bracco, Guerbet. Thomas Neß: Consultancy (current) - Sanofi, Santen, Novartis, Expert testimony (past) - Novartis. MRI contrast agents of the above-mentioned companies were used. The authors of this manuscript declare no other relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by DFG. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. No study subjects or cohorts have been previously reported. Methodology: prospective, diagnostic study, multi-center study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Veldhoen, S., Klink, T., Geiger, J. et al. MRI displays involvement of the temporalis muscle and the deep temporal artery in patients with giant cell arteritis. Eur Radiol 24, 2971–2979 (2014). https://doi.org/10.1007/s00330-014-3255-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3255-1