Abstract
The Achilles tendon (AT) insertion is the most common site of enthesitis in psoriatic arthritis (PsA). The structure and function of the AT in PsA, and the prevalence of mid-portion pathology, is unknown. To compare the structure and function of the AT in people with PsA with self-reported AT pain (PsA + AT), PsA without self-reported AT pain (PsA-AT) and healthy controls. A cross-sectional, observational study was conducted. The ATs were assessed by clinical and US examination (B-mode and Power Doppler), performance-based testing (bilateral heel raise test (HRT) and 10 m walk test), and patient-reported outcome measures (PROMs) (including the Victorian Institute of Sport Assessment-Achilles [VISA-A]). Between-group differences were described using descriptive statistics, Chi-squared testing, parametric (1-way ANOVA) and non-parametric (Mann-Whitney or Kruskal-Wallis) testing. 22 PsA (11 per group) and 11 healthy control participants who were comparable in terms of sex, age, and BMI (PsA-AT = longer PsA disease duration) were recruited. VISA-A scores were significantly worse in the PsA + AT group compared to the PsA-AT group and healthy controls (p < 0.001). Inflammatory US features were significantly more prevalent in the PsA + AT group (p < 0.001). Mid-portion AT pathology was observed in the PsA + AT group, irrespective of entheseal disease. Clinical examination alone missed 5/7 cases of ‘active’ US-confirmed AT enthesitis. AT functional deficits were significant in the PsA + AT group and both PsA groups had lower HRT repetition rates and walked slower compared to healthy controls. Less than 1/3 of the PsA + AT group had received podiatry or physiotherapy care. Significant differences in the structure and function of the AT in PsA were noted. Despite management in line with current guidance, AT pain appears to persist and can result in severe functional impairment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Enthesitis, which presents as pain, swelling and inflammation at the insertion sites of tendons and ligaments to bone, is a hallmark clinical feature of psoriatic arthritis (PsA) with the insertion of the Achilles tendon (AT) to the posterior calcaneum the most common site affected [1]. The presence of enthesitis has been shown to be associated with increased levels of pain and disability, poorer quality of life and increased use of non-steroidal anti-inflammatory drugs (NSAIDs) and opioids [2]. Entheseal tissues may also play a role in the pro-inflammatory response to external stress and a possible link between repeated physical trauma and flare in PsA has previously been highlighted [3, 4]. Early identification and tight control of PsA disease activity, including enthesitis, is vital to prevent long-term functional impairment [5, 6].
The AT enthesis is often regarded as the archetypal ‘enthesis organ’ which includes the AT, retrocalcaneal bursa, Kager’s fat pad, calcaneal bone, fibrocartilage, and surrounding synovium [7]. Due to the location and weight-bearing nature of the AT, this tendon is prone to injury and micro-damage, even in healthy populations [8]. However, in contrast to enthesitis in PsA, in healthy populations the mid-portion of the AT (2–6 cm proximal to the insertion) is the most prevalent site of pathology [9, 10]. The prevalence and impact of mid-portion AT pathology in PsA has not yet been reported.
Clinical assessment of AT enthesitis in PsA has shown to correlate poorly with ultrasound (US) findings [11,12,13]. The Leeds Enthesitis Index (LEI) is the most widely used clinical enthesitis index validated in PsA and includes the AT but concerns around the sensitivity and specificity of the LEI have been reported [14, 15]. Clinical examination of AT enthesitis assesses pain on palpation at the AT insertion but cannot discriminate between inflammatory or structural pathology [12, 16]. It is also unclear whether clinical examination can differentiate between AT enthesitis and biomechanically-driven AT tendinopathy in a PsA population. Importantly, the management of enthesitis (NSAIDs, physiotherapy, corticosteroid injection, conventional disease-modifying anti-rheumatic drugs (csDMARDs) and biologics (bDMARDs)) [6, 17] differs greatly from the evidence-base and recommendations for more biomechanically-driven AT tendinopathy (eccentric exercises) [18].
US has shown good sensitivity and specificity for assessing features of AT enthesitis in PsA [11,12,13, 16, 19]. There are, however, a range of definitions and scoring criteria available for US assessment of AT enthesitis in PsA [20]. The latest OMERACT consensus-based definitions and scoring criteria are the first to group enthesitis features into either inflammatory (hypoechogenicity, increased tendon thickness and the presence of Doppler signal) or structural (enthesophytes/calcification and erosions) features [21]. To date, there are no evidence-informed treatment guidelines for AT enthesitis based on criteria derived from imaging-based outcomes i.e., the presence of structural or inflammatory changes. Individual US features of AT enthesitis also overlap with the US-based criteria for detecting insertional AT tendinopathy [22]. Due to the prevalence and pathogenesis of enthesitis in PsA, US research has largely focussed on entheseal pathology at the AT and the prevalence and impact of mid-portion AT tendinopathy has not yet been explored in PsA.
Despite a large number of studies highlighting the prevalence of AT enthesitis in PsA, very little has been published on the function of the AT in this population, which could be key to optimising care and lessening the burden of disease. Foot pain due to issues such as dactylitis, has been shown to reduce walking velocity in people with PsA [23, 24]. Woodburn et al. also reported reduced ankle power and AT force in a PsA cohort with US-confirmed AT enthesitis compared to healthy controls [25]. Exercise-based therapy has been advocated as a first-line treatment modality for enthesitis however PsA-related foot pain can be a barrier to physical activity but can also, significantly affect quality of life more generally [6, 26, 27].
This cross-sectional observational study aimed to compare AT structure and function, by utilising US imaging and performance-based testing, in people with PsA, with and without AT pain, compared to healthy controls. Greater understanding of both AT pathology and associated impairments in people with PsA with and without AT pain may help to inform more appropriate, targeted medical and non-medical management strategies in future.
Materials and methods
Sample population
This study compared 3 groups: people with PsA with AT pain, people with PsA without AT pain and age and sex-matched healthy controls. Adults aged ≥ 18 years with a clinician-diagnosis of PsA, with (PsA + AT) and without (PsA-AT) current uni/bilateral self-reported AT pain, were recruited from NHS Greater Glasgow and Clyde rheumatology outpatient clinics from January 2020 to February 2022. Participants were excluded if they reported a recent change in their systemic medication (within the last 6 weeks); intramuscular or local corticosteroid injection within the last 6 weeks; a history of AT rupture; a history of AT or major lower limb surgery; recent serious medical event or severe comorbid disease. Age and sex-matched healthy controls were recruited via Glasgow Caledonian University (GCU) staff email if they fulfilled the same criteria and had no history of an inflammatory arthropathy or self-reported AT pain.
Non-probability sampling was adopted, and participants were consecutively identified by the referring clinician (rheumatology health care professional). Written informed consent was obtained for all participants and the study was approved by the London Bridge Research Ethics Committee (19/LO/1139) and GCU School of Health and Life Sciences research ethics committee (HLS/PSWAHS/18/185) for PsA patients and healthy volunteers, respectively.
Study protocol
Demographic data including age, sex, PsA disease duration, smoking status and current medications were collected using a standardised questionnaire. Patient-reported outcome measures (PROMs) included the Victorian Institute for Sports Assessment – Achilles (VISA-A) [28] questionnaire to assess the severity of AT symptoms ; the Health Assessment Questionnaire – Disability Index (HAQ-DI) [29] questionnaire to assess self-reported functional ability; the PsA Impact of Disease 12-item (PsAID-12) [30] questionnaire to assess PsA disease-related quality of life; the Hospital Anxiety and Depression Scale (HADS) [31] to assess levels of anxiety and depression; current and average AT pain (over the last 7 days) was reported using 0–10 pain visual analogue scale (VAS) and in the absence of a PsA-specific tool, the Rheumatoid Arthritis Foot Disease Activity Index-5 (RADAI-F5) [32] was used to measure foot disease activity.
Clinical assessment of AT
Clinical assessment was performed by the lead researcher (AP - podiatrist) prior to US examination. The LEI was conducted to clinically assess for the presence of pain/tenderness on palpation at each AT enthesis. Subjective clinical assessments included the presence of current self-reported pain in the ATs and self-reported morning stiffness at the AT. Pain during passive dorsiflexion of the AT (with the knee flexed) and resisted plantarflexion of the ankle was also assessed.
US assessment of AT
The European Alliance of Associations for Rheumatology (EULAR) recommendations for the reporting of US studies in rheumatic and musculoskeletal diseases (RMDs) were used to guide the reporting of US procedures and results [33]. A CASE-trained (Consortium for the Accreditation of Sonographic Education postgraduate certificate) US practitioner (AP) with 3 years of scanning experience performed all US examinations. The 2017 EULAR standardised procedures for US imaging in rheumatology were followed [34]. Participants were positioned prone with both feet in passive plantarflexion. The ATs were scanned in both longitudinal and transverse views and both static images and dynamic cine-loops were recorded. Image acquisition and US reporting was performed by the same US practitioner during a single study visit.
All scanning was performed on the same GE LOGIQ S8 US machine in the same consulting room using a multi-frequency linear transducer (L6-15 MHz). Conventional greyscale (B-mode) and Power Doppler imaging were utilised to assess the full length of the ATs. Power Doppler settings were adjusted (pulse repetition frequency, gain, box size/positioning) for each participant and the pressure on the tendons from the transducer was minimised to increase sensitivity and reduce the presence of artefacts [35].
The OMERACT consensus-based definitions of features of enthesitis on US were adopted [21]. Power Doppler signal at the entheses was scored from 0 to 3 (0 = No Doppler signal, 1 = < 2 punctiform (discrete areas) Doppler signal with no confluent (merging together) Doppler signal, 2 = 2–4 punctiform Doppler signal or 1 confluent Doppler signal and 3 = > 4 punctiform Doppler signals or > 1 confluent Doppler signal) based on OMERACT recommendations [36]. The anteroposterior diameter of the AT was measured in both longitudinal and transverse planes at 3 locations: (1) the insertion of the deep margin of the AT to the calcaneal bone, (2) the thickest part of the mid-portion (2–6 cm from insertion), and (3) the soleus myotendinous junction [37].
AT function
Functional endurance of the AT was measured using the bilateral heel raise test [38]. Participants were instructed to lift their heels and rise onto their forefoot with both feet on the ground, with the option of holding on to the wall for stability. When participants reached maximum plantarflexion, the researcher marked the participants’ height (top of head) using an adjustable height chart bar. Participants performed as many heel-raises as they could (with the top of their head reaching the bar) until the point of self-determined fatigue. If participants were unable to do any heel raises the score was recorded as zero. No encouragement was given throughout the test. Speed of repetitions was self-selected, and the repetition rate (repetitions per second) was recorded.
Gait speed was assessed by the 10-metre walk test (10MWT). A 14-metre walkway was set up with 2 m to warm up and 2 m at the end to slow down to a stop [24]. Participants were instructed to walk at a ‘comfortable pace’ and could rest between the two walking trials. If required, participants were permitted to use a walking aid device for stability. The average speed (in seconds) of the two walking trials was recorded.
Statistical analysis
Statistical analyses were performed using SPSS version 26 (IBM Corp, Armonk, NY, USA). Descriptive statistics were used to describe demographic, clinical, US, and performance-based data as mean (standard deviation (SD)), median (inter-quartile range (IQR)), or absolute (n) and relative frequencies (%). Between group differences were described using Chi-squared testing (X2), parametric (1-way ANOVA and post-hoc testing) and non-parametric (Mann-Whitney (U) or Kruskal-Wallis (H)) testing where appropriate (statistical significance was defined as p ≤ 0.05). Using one-way ANOVA to evaluate differences between groups, based on an anticipated effect size of 0.55, p = 0.05 significance and 0.8 power, we aimed for 12 participants in each group (total n = 36). As no follow-up was involved, it was not necessary to account for attrition.
Results
A total of 33 participants were recruited to the study, with 11 in each (Table 1)group. There were no significant differences in sex (H(2) = 0.241, p = 0.887), age (H(2) = 2.119, p = 0.347) or body mass index (BMI) (H(2) = 3.619, p = 0.164) between the three groups. The PsA-AT group had a significantly higher disease duration than the PsA + AT group (U = 95.5, p = 0.019) but age (U = 80.5, p = 0.193) and BMI scores (U = 30.0, p = 0.152) were not significantly different between these two PsA groups. In the PsA + AT group, the duration of AT symptoms varied (median 2 years, range 0.25-20 years) and 3/11 participants experienced AT symptoms prior to their PsA diagnosis (range 2–6 years).
In line with the study design, there was a significant association between group allocation and the presence of AT involvement on LEI (X2(2) = 14.67, p = 0.001), self-reported current AT pain (X2(2) = 33.0, p < 0.001), self-reported AT morning stiffness (X2(2) = 21.21, p < 0.001), pain on passive dorsiflexion of the ankle (X2(2) = 29.07, p = 0.011) and pain on resisted plantarflexion of the ankle (X2(2) = 2.06, p = 0.003) (Table 2). Self-reported AT pain VAS scores were significantly different between groups for both current AT pain (H(2) = 19.78, p < 0.001) and average AT pain over the last 7 days (H(2) = 20.5, p < 0.001). There were no significant differences between groups for the 10MWT but pairwise comparison testing showed the heel raise repetition rate was significantly different between PsA groups (p = 0.005) and between PsA participants and healthy controls (U = 53.0, p = 0.008).
Ultrasound features
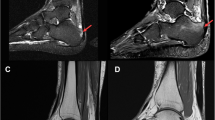
The presence of ‘active’ enthesitis (2018 OMERACT definition [21]), was detected in 7/22 AT entheses (5 participants, including 2 with bilateral) in the PsA + AT group (Table 3). Data regarding US features in participants is also presented (Supplementary Table 1.) No participants in the other two groups had US evidence of active enthesitis. ‘Non-active’ enthesitis, i.e. US enthesitis features but no Power Doppler signal, was detected across all three groups, with no significant differences between groups.
While individual inflammatory features of hypoechogenicity and increased thickness were also noted in some PsA and healthy participants without AT pain, these were much more common in those with PsA + AT while Power Doppler was only noted in the PsA + AT group. Individual structural US features were noted in both PsA groups, regardless of presence of current AT pain, and significantly more often than in healthy controls. The most common structural US finding in healthy controls was the presence of enthesophytes. The main and only significant difference in AT thickness on US was increased AT thickness at the entheseal insertion in those with PsA + AT.
Inflammatory and structural US changes were more common in the PsA + AT group. Relative to the healthy control group, both PsA groups exhibited more structural features of entheseal pathology. Inflammation identified by Power Doppler imaging was only detected in the PsA + AT group.
Of the 22 participants with PsA, AT enthesitis was detected on LEI in 9 entheses (6 participants with PsA + AT). The association of US findings with LEI is presented in Table 4. The presence of non-active enthesitis features (X2(1) = 7.49, p = 0.006), inflammatory features (X2(1) = 9.634, p = 0.002) including hypoechogenicity ( X2(1) = 13.489, p < 0.001) and entheseal thickening X2(1) = 11.016, p = 0.001), structural features (X2(1) = 5.852, p = 0.016) including enthesophytes (X2(1) = 7.833, p = 0.005) and erosions (X2(1) = 9.610, p = 0.002) were significantly different between groups. For AT thickness, only entheseal thickness measurements were significantly different between groups (U = 275, p < 0.001).
PROMs in the three groups were assessed although PsAID-12 (impact of PsA on quality of life) was only assessed in PsA participants (Table 5). The presence of self-reported AT pain was significantly associated with higher PsAID-12, HAQ-DI and RADAI-F5 scores indicating a negative impact on quality of life and foot disease activity. In contrast, the anxiety and depression scores were higher in participants with PsA compared to healthy controls, regardless of the presence or absence of self-reported AT pain.
Table 6. presents a summary of the clinical and demographic data for the PsA + AT group. Only 3/11 participants had received, or were waiting to receive, treatment for their AT pain/pathology.
Discussion
This study presents and brings together novel findings around the pathology, structure, and function of the AT in people with PsA with and without self-reported AT pain. The PsA + AT group showed significant AT functional impairment and lower PsA-related quality of life scores (assessed by the PsAID-12) compared to the PsA-AT group and healthy controls. While some US AT findings were noted in all groups, these were mainly structural findings in those without AT pain, with inflammatory features of enthesitis on US (hypoechogenicity, tendon thickening and Power Doppler signal) more prevalent in the PsA + AT group, although not in all.
The PsA + AT pain group had the highest number of features of AT pathology on clinical examination, and positive results for AT tendinopathy based on tendon loading tests (pain on passive dorsiflexion and pain on resisted plantarflexion) were only found in the PsA + AT group. However, this study adds to a body of evidence that suggests there is a poor correlation between clinical assessment for AT enthesitis (palpatory tenderness) and US findings [11,12,13, 16]. Importantly, clinical examination only picked up on 2/7 (28.6%) cases of US ‘active’ enthesitis (US enthesitis features with the presence of Doppler signal). Over 50% of AT entheses in the PsA-AT group had one or more structural feature of enthesitis (calcification, enthesophytes or erosion) on US examination and 30% had one or more inflammatory features (hypoechogenicity, thickening, Power Doppler signal). This potential lack of correlation between clinically-defined and US-defined AT enthesitis has been previously reported in a spondyloarthritis cohort where the authors suggested that differential diagnosis for clinically-defined AT enthesitis included subtalar joint arthritis, tibialis posterior tenosynovitis and retrocalcaneal bursitis [39]. In this study, mid-portion AT tendinopathic changes, intra-substance mid-portion tears and retrocalcaneal bursitis were observed on US in both PsA groups. This again highlights the potential clinical utility of using US to define the underlying pathology at the AT and use this to tailor treatment accordingly.
The OMERACT consensus-based, validated definitions and scoring of enthesitis features used in this study have been reported to have excellent inter and intra-reader agreement [21]. Individual enthesitis features were scored as present/absent and although the original OMERACT enthesitis scoring system does not include a score for Doppler signal, the presence of Power Doppler signal was scored from 0 to 3 in this study based on the updated 2019 OMERACT definitions for ultrasonographic pathologies and elementary lesions of RMDs [36]. Power Doppler signal was detected at 7 AT entheses (31.8%) in the PsA + AT group (15.9% PsA participants) and all scored as Grade 1 (< 2 punctiform Doppler signals with no confluent Doppler signal). Previous studies have reported similar incidences of Doppler activity at the AT enthesis in PsA (range = 6-36%) [40,41,42,43,44].
PsA disease duration was significantly higher (p = 0.019) in the PsA-AT group compared to the PsA + AT group and this could potentially explain the similar prevalence of structural enthesitis features on US. Alternatively, individuals with PsA could just exhibit more US enthesitis features that may be asymptomatic. This could suggest participants have experienced symptoms of AT enthesitis (or subclinical manifestations) earlier on in their disease course that has resulted in persisting structural change i.e., this may reflect the natural course of AT enthesitis in PsA. Despite a relatively short PsA disease duration (9/11 participants < 8 years), and 10/11 participants on either csDMARD or bDMARD therapy, the majority of the PsA + AT group had structural features of AT enthesitis on US. Although enthesophytes have been detected in ‘normal’ AT entheses in healthy populations and appear to be more prevalent with increasing age [44], no significant differences in age were noted between PsA groups. Healthy control participants in this study also exhibited both structural and inflammatory features of enthesitis at the AT at lower rates that those with PsA + AT and none exhibited Power Doppler signal. Although these structural US features were significantly more prevalent in the PsA cohort compared to controls, it does highlight the likely role of biomechanics and resultant micro-trauma on the ‘normal’ enthesis. As the presence of enthesophytes is common in healthy populations and appears to be associated with age, the clinical relevance of the presence of structural entheseal features on US in PsA has been questioned [39, 44].
Previous studies have reported changes in walking speed and gait parameters in PsA [24,25,26]. This study showed a reduction in average walking speed in both PsA groups compared to healthy controls, but the difference was not statistically significant (p = 0.086). This difference may also be due to involvement of other lower limb or axial joints in PsA, which were not formally assessed. In this study, AT function assessed using the heel raise test was significantly impaired in the PsA groups compared to healthy controls (p = 0.008). The PsA + AT group also scored significantly worse on the PsAID-12, HAQ-DI and RADAI-F5 compared to the PsA-AT group. However, in the absence of PsA-validated PROMs, the measurement properties of the RADAI-F5 for PsA populations is still unknown and this can also be affected by involvement of other joints in the foot and/or ankle beyond the AT.
In the PsA + AT group, three participants experienced AT symptoms prior to their PsA diagnosis, of which two exhibited the highest number of AT enthesitis features on US compared to the rest of the symptomatic group. These three participants with AT pain prior to their PsA diagnosis had either visited a physiotherapist or podiatrist for AT treatment, or were awaiting treatment, while the rest of the symptomatic cohort reported no physiotherapy or podiatry input. Inadequate access to foot care provision in PsA has previously been highlighted with only 20% of PsA patients with moderate-to-high levels of foot impairment and disability receiving foot care in the UK in 2010 [45] and similar barriers to accessing care reported in Australia and New Zealand in 2019 [27]. This study has also demonstrated that AT pathology can often extend beyond the enthesis in PsA and therefore identification of the origin of pain using US as a supporting tool, i.e., structural, inflammatory, or mid-portion pathology, could help guide more targeted therapy.
Limitations
A limitation of the study is the small sample size and possibility of selection bias as we did not adopt random sampling. As a result, the US and clinical presentation of AT pathology in the PsA groups may not be representative of the PsA population. However, the prevalence of AT pathology in both PsA participants and healthy controls is in line with previously published US studies [11, 13, 43]. Based on the EULAR recommendations for the reporting of US studies in RMDs, we acknowledge some further US protocol-related limitations to our study [34]. Although there are advantages to the same US practitioner using the same US machine to perform all examinations, this meant the US practitioner was not blinded to the results of the clinical examination or group allocation. Although US image acquisition was standardised, there remains an element of subjectivity and US practitioner-interpretation with all US-based findings. We also did not control for contextual factors such as the ambient temperature [47], limiting physical activity prior to US examination or controlling the use of NSAIDs prior to examination, which could all influence Doppler imaging [48]. In the PsA + AT cohort, 3/11 reported their AT symptoms at the time of assessment were unilateral however US scores (B-mode and Power Doppler) were reported for both ATs. The decision to include both ATs in the symptomatic group was made based on previous research that has shown pathology can often occur at the contralateral limb but be asymptomatic [49, 50]. The study also adopted PROMs not yet validated in a PsA population, including the VISA-A.
Conclusion
In summary, there were significant differences in the structure and function of the AT between groups which could be clinically relevant when assessing and managing AT pain in people with PsA, although the presence of these features in the general population also needs to be considered. The results of this study add to a body of literature suggesting AT pathology in PsA cannot be fully assessed by clinical examination alone. Although the prevalence of AT enthesitis in PsA is well-documented, our findings reveal that AT enthesitis and mid-portion Achilles tendinopathy may co-exist in people with PsA, or be misdiagnosed, which could affect the efficacy of treatment interventions. As treatment guidelines for AT enthesitis and AT tendinopathy vary greatly, and distinguishing these is complex, it is likely that PsA patients with symptomatic ATs may be receiving inappropriate, or suboptimal, care.
Assessments of AT function showed significant impairment in people with PsA compared to healthy controls, regardless of self-reported AT pain. Less than a third of participants had received treatment from podiatrist or physiotherapist for their AT symptoms, further highlighting the unmet need for foot and ankle care in PsA. Of note, PsA participants with AT pain in receipt of medical management in line with the current clinical guidelines appear to still be severely impacted by their AT pain despite these therapies. Robust research is required to address the evidence gap with regards to standardised assessment and non-pharmacological management of AT pathology in PsA.
Abbreviations
- 10MWT − 10:
-
Metre walk test
- AT:
-
Achilles tendon
- bDMARDs:
-
Biologic disease-modifying anti-rheumatic drugs
- BMI:
-
Body mass index
- CASE:
-
Consortium for the Accreditation of Sonographic Education
- csDMARDs:
-
Conventional disease-modifying anti-rheumatic drugs
- EULAR:
-
European Alliance of Associations for Rheumatology
- GCU:
-
Glasgow Caledonian University
- HADS:
-
Hospital Anxiety and Depression Scale
- HADS:
-
A-Hospital Anxiety and Depression Scale-Anxiety component
- HADS:
-
D-Hospital Anxiety and Depression Scale-Depression component
- HAQ:
-
DI-Health Assessment Questionnaire-Disability Index
- HRT:
-
Heel raise test
- IQR:
-
Inter-quartile range
- LEI:
-
Leeds Enthesitis Index
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- OMERACT:
-
Outcome Measures in Rheumatology
- PROMs:
-
Patient-reported outcome measures
- PsA:
-
Psoriatic arthritis
- PsA + AT:
-
PsA with self-reported Achilles tendon pain
- PsA:
-
AT-PsA with no self-reported Achilles tendon pain
- PsAID:
-
12-PsA Impact of Disease-12 items
- RADAI:
-
F5-Rheumatoid Arthritis Foot Disease Activity Index-5
- RMDs:
-
Rheumatic and musculoskeletal diseases
- SD:
-
Standard deviation
- US:
-
Ultrasound
- VAS:
-
Visual analogue scale
- VISA:
-
A-Victorian Institute for Sports Assessment-Achilles questionnaire
References
Polachek A, Mmath SL, Chandran V, Gladman DD (2016) Clinical Enthesitis in a prospective longitudinal psoriatic arthritis cohort: incidence, prevalence, characteristics, and Outcome. Arthritis Care Res (Hoboken) 69:1685–1691. https://doi.org/10.1002/acr.23174
Orbai AM, Birt JA, Holdsworth EA, Booth N, Malatestinic WN, Sprabery AT, Reginato AM (2020) Impact of Enthesitis on Psoriatic Arthritis patient-reported outcomes and physician satisfaction with treatment: data from a multinational patient and physician survey. Rheumatol Ther 7:937–948. https://doi.org/10.1007/s40744
Eder L, Law T, Chandran V, Shanmugarajah S, Shen H, Rosen CF, Cook RJ, Gladman DD (2011) Association between environmental factors and onset of psoriatic arthritis in patients with psoriasis. Arthritis Care Res (Hoboken) 63:1091–1097. https://doi.org/10.1002/ACR.20496
Thorarensen SM, Lu N, Ogdie A, Gelfand JM, Choi HK, Love TJ (2017) Physical trauma recorded in primary care is associated with the onset of psoriatic arthritis among patients with psoriasis. Ann Rheum Dis 76:521–525. https://doi.org/10.1136/ANNRHEUMDIS-2016-209334
Coates LC, Moverley AR, McParland L, Brown S, Navarro-Coy N, O’Dwyer JL, Meads DM, Emery P, Conaghan PG, Helliwell PS (2016) Effect of tight control of inflammation in early psoriatic arthritis (TICOPA): a UK Multicentre, open-label, randomised controlled trial. Lancet 386:2489–2498. https://doi.org/10.1016/S0140-6736(15)00347-5
Coates LC, Soriano ER, Corp N, Bertheussen H, Callis Duffin K, Campanholo CB, Chau J, Eder L, Fernández-Ávila DG, FitzGerald O, Garg A, Gladman DD, Goel N, Helliwell PS, Husni ME, Jadon DR, Katz A, Laheru D, Latella J, Leung YY, Lindsay C, Lubrano E, Mazzuoccolo LD, Mease PJ, O’Sullivan D, Ogdie A, Olsder W, Palominos PE, Schick L, Steinkoenig I, de Wit M, van der Windt DA, Kavanaugh A (2022) Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA): updated treatment recommendations for psoriatic arthritis. Nat Rev Rheumatol 18(8):465–479. https://doi.org/10.1038/s41584-022-00798-0. GRAPPA Treatment Recommendations domain subcommittees
Benjamin M, McGonagle D (2009) The enthesis organ concept and its relevance to the spondyloarthropathies. Adv Exp Med Biol 649:57–70. https://doi.org/10.1007/978-1-4419-0298-6_4
Wang Y, Zhou H, Nie Z, Cui S (2022) Prevalence of Achilles tendinopathy in physical exercise: a systematic review and meta-analysis. Sports Med Health Sci 4(3):152–159. https://doi.org/10.1016/j.smhs.2022.03.003
Maffulli N, Sharma P, Luscombe KL (2004) Achilles tendinopathy: aetiology and management. J R Soc Med 97(10):472–476. https://doi.org/10.1177/0141076809701004
de Jonge S, van den Berg C, de Vos RJ, van der Heide HJ, Weir A, Verhaar JA, Bierma-Zeinstra SM, Tol JL (2011) Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med 45(13):1026–1028. https://doi.org/10.1136/bjsports-2011-090342
Michelsen B, Diamantopoulos AP, Soldal DM, Hammer HB, Kavanaugh A, Haugeberg G (2017) Achilles enthesitis defined by ultrasound is not associated with clinical enthesitis in patients with psoriatic arthritis. RMD Open 3(2):e000486. https://doi.org/10.1136/rmdopen-2017-000486
Yamada Y, Inui K, Okano T, Mandai K, Mamoto K, Koike T, Takeda S, Yamashita E, Yoshida Y, Tateishi C, Tsuruta D, Nakamura H (2021) Ultrasound assessment, unlike clinical assessment, reflects enthesitis in patients with psoriatic arthritis. Clin Exp Rheumatol 39(1):139–145. https://doi.org/10.55563/clinexprheumatol/u8qc6c
Freeston JE, Coates LC, Helliwell PS, Hensor EM, Wakefield RJ, Emery P, Conaghan PG (2012) Is there subclinical enthesitis in early psoriatic arthritis? A clinical comparison with power doppler ultrasound. Arthritis Care Res (Hoboken) 64(10):1617–1621. https://doi.org/10.1002/acr.21733
Healy PJ, Helliwell PS (2008) Measuring clinical enthesitis in psoriatic arthritis: assessment of existing measures and development of an instrument specific to psoriatic arthritis. Arthritis Rheum 59(5):686–691. https://doi.org/10.1002/art.23568
Mease P (2020) Enthesitis in psoriatic arthritis (part 3): clinical assessment and management. Rheumatology (Oxford) 59(Suppl 1):i21–i28. https://doi.org/10.1093/rheumatology/keaa042
Kristensen S, Christensen JH, Schmidt EB, Olesen JL, Johansen MB, Arvesen KB, Schlemmer A (2016) Assessment of enthesitis in patients with psoriatic arthritis using clinical examination and ultrasound. Muscles Ligaments Tendons J 6(2):241–247. https://doi.org/10.11138/mltj/2016.6.2.241
Mian A, Ibrahim F, Scott DL (2019) A systematic review of guidelines for managing rheumatoid arthritis. BMC Rheumatol 3:42. https://doi.org/10.1186/s41927-019-0090-7
Silbernagel KG, Hanlon S, Sprague A (2020) Current clinical concepts: conservative management of Achilles Tendinopathy. J Athl Train 55(5):438–447. https://doi.org/10.4085/1062-6050-356-19
Dubash SR, De Marco G, Wakefield RJ, Tan AL, McGonagle D, Marzo-Ortega H (2020) Ultrasound Imaging in Psoriatic Arthritis: what have we Learnt in the last five years? Front Med (Lausanne) 7:487. https://doi.org/10.3389/fmed.2020.00487
Patience A, Steultjens MP, Hendry GJ (2021) Ultrasound features of Achilles enthesitis in psoriatic arthritis: a systematic review. Rheumatol Adv Pract 5(Suppl 2):ii19–ii34. https://doi.org/10.1093/rap/rkab056
Balint PV, Terslev L, Aegerter P, Bruyn GAW, Chary-Valckenaere I, Gandjbakhch F, Iagnocco A, Jousse-Joulin S, Möller I, Naredo E, Schmidt WA, Wakefield RJ, D’Agostino MA (2018) OMERACT Ultrasound Task Force members. Reliability of a consensus-based ultrasound definition and scoring for enthesitis in spondyloarthritis and psoriatic arthritis: an OMERACT US initiative. Ann Rheum Dis 77(12):1730–1735. https://doi.org/10.1136/annrheumdis-2018-213609
Matthews W, Ellis R, Furness JW, Rathbone E, Hing W (2020) Staging achilles tendinopathy using ultrasound imaging: the development and investigation of a new ultrasound imaging criteria based on the continuum model of tendon pathology. BMJ Open Sport Exerc Med 6(1):e000699. https://doi.org/10.1136/bmjsem-2019-000699
Wilkins RA, Siddle HJ, Redmond AC, Helliwell PS (2016) Plantar forefoot pressures in psoriatic arthritis-related dactylitis: an exploratory study. Clin Rheumatol 35(9):2333–2338. https://doi.org/10.1007/s10067-016-3304-z
Walha R, Gaudreault N, Dagenais P, Boissy P (2022) Spatiotemporal parameters and gait variability in people with psoriatic arthritis (PsA): a cross-sectional study. J Foot Ankle Res 15(1):19. https://doi.org/10.1186/s13047-022-00521-y
Woodburn J, Hyslop E, Barn R, McInnes IB, Turner DE (2013) Achilles tendon biomechanics in psoriatic arthritis patients with ultrasound proven enthesitis. Scand J Rheumatol 42(4):299–302. https://doi.org/10.3109/03009742.2012.747626
Rausch Osthoff AK, Niedermann K, Braun J, Adams J, Brodin N, Dagfinrud H, Duruoz T, Esbensen BA, Günther KP, Hurkmans E, Juhl CB, Kennedy N, Kiltz U, Knittle K, Nurmohamed M, Pais S, Severijns G, Swinnen TW, Pitsillidou IA, Warburton L, Yankov Z, Vliet Vlieland TPM (2018) 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis 77(9):1251–1260. https://doi.org/10.1136/annrheumdis-2018-213585
Carter K, Walmsley S, Chessman D, Rome K, Turner DE (2019) Perspectives of patients and health professionals on the experience of living with psoriatic arthritis-related foot problems: a qualitative investigation (. Clin Rheumatol 38(6):1605–1613. https://doi.org/10.1007/s10067-018-04411-2
Robinson JM, Cook JL, Purdam C, Visentini PJ, Ross J, Maffulli N, Taunton JE, Khan KM, Victorian Institute Of Sport Tendon Study Group (2001) The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med 35(5):335–341. https://doi.org/10.1136/bjsm.35.5.335
Bruce B, Fries JF (2003) The Stanford Health Assessment Questionnaire: dimensions and practical applications. Health Qual Life Outcomes 1:20. https://doi.org/10.1186/1477-7525-1-20
Gossec L, de Wit M, Kiltz U, Braun J, Kalyoncu U, Scrivo R, Maccarone M, Carton L, Otsa K, Sooäär I, Heiberg T, Bertheussen H, Cañete JD, Sánchez Lombarte A, Balanescu A, Dinte A, de Vlam K, Smolen JS, Stamm T, Niedermayer D, Békés G, Veale D, Helliwell P, Parkinson A, Luger T, Kvien TK, EULAR PsAID Taskforce (2014) A patient-derived and patient-reported outcome measure for assessing psoriatic arthritis: elaboration and preliminary validation of the psoriatic arthritis impact of Disease (PsAID) questionnaire, a 13-country EULAR initiative. Ann Rheum Dis 73(6):1012–1019. https://doi.org/10.1136/annrheumdis-2014-205207
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Hoque A, Gallagher K, McEntegart A, Porter D, Steultjens M, Woodburn J, Hendry GJ (2021) Measuring inflammatory Foot Disease in Rheumatoid Arthritis: Development and Validation of the Rheumatoid Arthritis Foot Disease Activity Index-5. Arthritis Care Res (Hoboken) 73(9):1290–1299. https://doi.org/10.1002/acr.24259
Costantino F, Carmona L, Boers M, Backhaus M, Balint PV, Bruyn GA, Christensen R, Conaghan PG, Ferreira RJO, Garrido-Castro JL, Guillemin F, Hammer HB, van der Heijde D, Iagnocco A, Kortekaas MC, Landewé RB, Mandl P, Naredo E, Schmidt WA, Terslev L, Terwee CB, Thiele R, D’Agostino MA (2021) EULAR recommendations for the reporting of ultrasound studies in rheumatic and musculoskeletal diseases (RMDs). Ann Rheum Dis 80(7):840–847. https://doi.org/10.1136/annrheumdis-2020-219816
Möller I, Janta I, Backhaus M, Ohrndorf S, Bong DA, Martinoli C, Filippucci E, Sconfienza LM, Terslev L, Damjanov N, Hammer HB, Sudol-Szopinska I, Grassi W, Balint P, Bruyn GAW, D’Agostino MA, Hollander D, Siddle HJ, Supp G, Schmidt WA, Iagnocco A, Koski J, Kane D, Fodor D, Bruns A, Mandl P, Kaeley GS, Micu M, Ho C, Vlad V, Chávez-López M, Filippou G, Cerón CE, Nestorova R, Quintero M, Wakefield R, Carmona L, Naredo E (2017) The 2017 EULAR standardised procedures for ultrasound imaging in rheumatology. Ann Rheum Dis 76(12):1974–1979. https://doi.org/10.1136/annrheumdis-2017-211585
Torp-Pedersen S, Christensen R, Szkudlarek M, Ellegaard K, D’Agostino MA, Iagnocco A, Naredo E, Balint P, Wakefield RJ, Torp-Pedersen A, Terslev L (2015) Power and color doppler ultrasound settings for inflammatory flow: impact on scoring of disease activity in patients with rheumatoid arthritis. Arthritis Rheumatol 67(2):386–395. https://doi.org/10.1002/art.38940
Bruyn GA, Iagnocco A, Naredo E, Balint PV, Gutierrez M, Hammer HB, Collado P, Filippou G, Schmidt WA, Jousse-Joulin S, Mandl P, Conaghan PG, Wakefield RJ, Keen HI, Terslev L, D’Agostino MA, OMERACT Ultrasound Working Group (2019) OMERACT definitions for Ultrasonographic Pathologies and Elementary lesions of Rheumatic disorders 15 years on. J Rheumatol 46(10):1388–1393. https://doi.org/10.3899/jrheum.181095
Aydın SZ, Filippucci E, Atagündüz P, Yavuz Ş, Grassi W, Direskeneli H (2014) Sonographic measurement of Achilles tendon thickness in seronegative spondyloarthropathies. Eur J Rheumatol 1(1):7–10. https://doi.org/10.5152/eurjrheum.2014.002
Monteiro DP, Britto RR, Fregonezi GAF, Dias FAL, Silva MGD, Pereira DAG (2017) Reference values for the bilateral heel-rise test. Braz J Phys Ther 21(5):344–349. https://doi.org/10.1016/j.bjpt.2017.06.002
Felbo SK, Østergaard M, Sørensen IJ, Terslev L (2022) Ultrasound of the Heel improves diagnosis-Tender entheses in the Heel Region rarely corresponds to Inflammatory Enthesitis in patients with Peripheral Spondyloarthritis. J Clin Med 11(9):2325. https://doi.org/10.3390/jcm11092325
ElMallah R, Abdo M, Mobasher S (2020) The incremental value of ultrasound in detection of subclinical peripheral enthesitis in patients with spondyloarthritis. Egypt Rheumatologist 42(4):255–260. https://doi.org/10.1016/J.EJR.2019.04.005
Xie D, Jiao H, Yang A, Liu Z, He X (2019) Imaging features and diagnosis of early psoriatic arthritis with lower limb entheseal abnormalities in psoriasis patients under high frequency ultrasonography. Int J Clin Exp Med 12(6):7701–7708
Wervers K, Vis M, Rasappu N, van der Ven M, Tchetverikov I, Kok MR, Gerards AH, Hazes J, Luime JJ (2018) Modification of a sonographic enthesitis score to differentiate between psoriatic arthritis and young healthy volunteers. Scand J Rheumatol 47(4):291–294. https://doi.org/10.1080/03009742.2017.1393695
Fiorenza A, Bonitta G, Gerratana E, Marino F, Sarzi-Puttini P, Salaffi F, Atzeni F (2020) Assessment of enthesis in patients with psoriatic arthritis and fibromyalgia using clinical examination and ultrasound. Clin Exp Rheumatol 38(Suppl 123):31–39
Guldberg-Møller J, Terslev L, Nielsen SM, Kønig MJ, Torp-Pedersen ST, Torp-Pedersen A, Christensen R, Bliddal H, Ellegaard K (2019) Ultrasound pathology of the entheses in an age and gender stratified sample of healthy adult subjects: a prospective cross-sectional frequency study. Clin Exp Rheumatol (3):408–413
Hyslop E, McInnes IB, Woodburn J, Turner DE (2010) Foot problems in psoriatic arthritis: high burden and low care provision. Ann Rheum Dis 69(5):928. https://doi.org/10.1136/ard.2009.111971
Bandinelli F, Prignano F, Bonciani D, Bartoli F, Collaku L, Candelieri A, Lotti T, Matucci-Cerinic M (2013) Ultrasound detects occult entheseal involvement in early psoriatic arthritis independently of clinical features and psoriasis severity. Clin Exp Rheumatol 31(2):219–224
D’Agostino MA, Said-Nahal R, Hacquard-Bouder C, Brasseur JL, Dougados M, Breban M (2003) Assessment of peripheral enthesitis in the spondylarthropathies by ultrasonography combined with power doppler: a cross-sectional study. Arthritis Rheum 48(2):523–533. https://doi.org/10.1002/art.10812
Zayat AS, Conaghan PG, Sharif M, Freeston JE, Wenham C, Hensor EM, Emery P, Wakefield RJ (2011) Do non-steroidal anti-inflammatory drugs have a significant effect on detection and grading of ultrasound-detected synovitis in patients with rheumatoid arthritis? Results from a randomised study. Ann Rheum Dis 70(10):1746–1751. https://doi.org/10.1136/annrheumdis-2011-200017
Li Q, Zhang Q, Cai Y, Hua Y (2018) Patients with Achilles Tendon Rupture have a degenerated Contralateral Achilles Tendon: an Elastography Study. Biomed Res Int 2018(2367615). https://doi.org/10.1155/2018/2367615
Zhang Q, Cai Y, Hua Y, Shi J, Wang Y, Wang Y (2017) Sonoelastography shows that Achilles tendons with insertional tendinopathy are harder than asymptomatic tendons. Knee Surg Sports Traumatol Arthrosc 25(6):1839–1848. https://doi.org/10.1007/s00167-016-4197-8
Funding
This study was funded by a GCU-funded PhD studentship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Patience, A., Steultjens, M., Siebert, S. et al. Significant functional impairment and disability in individuals with psoriatic arthritis and Achilles tendon pain: a cross-sectional observational study. Rheumatol Int 44, 1469–1479 (2024). https://doi.org/10.1007/s00296-024-05629-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-024-05629-x