Abstract
Objectives
This cross-sectional study aimed to determine the prevalence and risk factors for sleep-related breathing disorders (SRBD) in newly diagnosed, untreated rheumatoid arthritis (RA) and psoriatic arthritis (PsA) patients, and to develop a screening algorithm for early detection.
Methods
We evaluated newly diagnosed RA or PsA patients using the Epworth Sleepiness Scale (ESS) questionnaire, cardiorespiratory polygraphy (RPG), and clinical and laboratory assessments. Sleep apnea syndrome (SAS) was diagnosed based on pathological RPG findings excessive daytime sleepiness, defined as ESS score above 10.
Results
The study included 39 patients (22 RA, 17 PsA) and 23 controls. In RPG, SRBD was identified in 38.5% of arthritis patients compared to 39.1% of controls (p = 1.00), with male gender (p = .004) and age (p < .001) identified as risk factors. Excessive daytime sleepiness was noted in 36.4% of RA patients, 17.6% of PsA patients, and 21.7% of controls. Of the 24 patients diagnosed with SRBD, 41.6% met the criteria for SAS. SAS prevalence was 31.8% among RA patients, 0% in PsA patients, and 13% in controls. A significant association was observed between excessive daytime sleepiness and SRBD (p = .036).
Conclusion
Our findings reveal a high prevalence of SRBD in newly diagnosed, untreated RA and PsA patients in ESS and RPG, with excessive daytime sleepiness being a reliable predictor of SRBD. Patients with RA exhibited a higher predisposition to SAS. We therefore suggest incorporating ESS and RPG as screening tools in RA or PsA for early detection and management of SRBD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disorders, which include conditions like sleep-related breathing disorders (SRBD), insomnia, circadian rhythm disturbances, hypersomnia/narcolepsy, parasomnias, and restless legs syndrome disrupt normal sleep patterns, impairing quality of life and emotional health. This can negatively affect physical, mental, and emotional well-being, thereby compromising overall health and safety [1,2,3].
In the context of arthritis diseases such as rheumatoid arthritis (RA) and psoriatic arthritis (PsA), there is a well described association between sleep disorders and the overall well-being of patients [3,4,5]. The presence of one can amplify the symptoms of the other. For instance, inadequate disease management leading to joint pain can negatively affect sleep. Conversely, sleep disorders can reduce pain tolerance, amplifying arthritis-associated manifestations [6,7,8,9].
Previous studies have shown that a substantial fraction of RA patients, estimated between 40 and 70%, report sleep disturbances, with a higher incidence among men and the elderly [9,10,11]. Main contributors to these sleep disturbances include pain and functional disability [12, 13]. Similarly, PsA patients often face sleep disturbances, which subsequently contribute to fatigue, anxiety, and depression, negatively affecting their quality of life [4, 14,15,16]. It’s emphasized that in the case of PsA, sleep disturbances are more often linked to musculoskeletal inflammation than dermatological symptoms [7, 17, 18]. Previous research found that while 16% of individuals with psoriasis experience seep disturbances, this number increased to up to 45% for PsA patients [19, 20]. Across various studies, t’s widely agreed that pain, fatigue, and physical impairments are the major contributors to sleep disturbances in PsA patients, with pain being the predominant factor [4, 7, 20]. However, it’s important to mention that the effects of sleep disturbances on quality of life in RA or PsA patients are often underestimated by healthcare professionals [11, 15].
While numerous studies have explored sleep quality and disturbances in RA or PsA patients with subjective self-report studies, data on SRBD remains sparse. Sleep apnea, characterized by intermittent breathing interruptions during sleep, can stem from upper airway obstruction or insufficient central respiratory center stimulation [21, 22]. This can result in lowered oxygen saturation, frequent arousal, and the subsequent release of stress hormones, thereby leading to nocturnal and daytime symptoms [21, 22]. Such disruptions could significantly impair health, exacerbating daytime sleepiness and reducing physical and mental performance, while elevating cardiovascular morbidity and mortality risks [23, 24].
In light of evidence suggesting that patients with arthritis, particularly those diagnosed with RA and PsA, are at a heightened risk for sleep apnea [25], our study sought to delve deeper into this connection. Previous research has shown varying prevalence rates of sleep apnea within the RA patient population, ranging from 10% to 50% [26,27,28, 10, 9], with a meta-analysis revealing a prevalence rate of 29.8% among RA patiens [29]. Conversely, data on PsA patients remain scarce, though some studies have pointed to a potential link between sleep apnea and an increased risk of developing PsA or psoriasis [30, 31], while others have found no significant association between PsA and an elevated risk of sleep apnea [32]. By focusing on RA and PsA, our research aims to fill a critical knowledge gap within the field of rheumatology and sleep medicine, while also acknowledging the broader spectrum of spondyloarthritis as an area for future exploration.
This study investigates the prevalence of SRBD in newly diagnosed and untreated RA or PsA patients. Utilizing a comprehensive approach, we incorporated Epworth Sleepiness Scale (ESS) questionnaire to evaluate daytime sleepiness alongside cardiorespiratory polygraphy (RPG) for empirical sleep assessment. Our aim was to establish SRBD screening protocols, enabling physicians to recognize early indicators, enhance patient outcomes, and bridge the existing knowledge gap surrounding SRBD in RA and PsA.
Materials and methods
Patient characteristics
Newly diagnosed and untreated RA or PsA patients from the the outpatient clinic of the Department of Rheumatology at the University Hospital Bonn, Germany, were enrolled between August 1, 2018, and August 31, 2022. Diagnosis was made by a board-certified rheumatologist. Inclusion criteria were: American College of Rheumatology (ACR)/ European League Against Rheumatism (EULAR) criteria of 2010 for diagnosis of RA [33], and GRAPPA Recommendations of 2016 for PsA [34]. Eligible patients were also required to have the necessary physical and mental capacity for study participation, be aged over 18, and provide consent for participation. Exclusion criteria included the use of any rheumatological or immunosuppressive medications prior to enrollment. Control participants were recruited from the same department, with a requirement of having no history of rheumatological conditions. Furthermore, each control was thoroughly assessed to confirm the absence of any rheumatological disease at the time of their inclusion in the study. To ensure comparability and reduce potential confounding factors, we performed group matching of these control individuals with our patient cohort based on age and gender. For each patient, demographic data and disease history were documented. The duration of arthritic symptoms and the Disease Activity Score in 28 joints using CRP (DAS28CRP) were recorded by the treating rheumatologist. Smoking history, pre-existing pulmonary conditions, medications, and current symptoms were assessed.
Cardiorespiratory polygraphy
All patients were tested for sleep apnea using RPG. Board-certified pulmonologists from the University Hospital Bonn interpreted the RPG results, applying criteria adapted from the 2012 American Academy of Sleep Medicine (AASM) guidelines for sleep and associated event assessments. The Apnea-Hypopnea Index (AHI), displaying the number of apneas and hypopneas per hour of total sleep time, was used [35]. An AHI exceeding 5 events/h was considered pathological and indicative of SRBD. SRBD severity levels were assessed as follows: AHI 0–5 events/h: non-pathological; AHI: 5–15 events/h: mild SRBD; AHI > 15–30 events/h: moderate SRBD; AHI > 30 events/h: severe SRBD. When SRBD was diagnosed, further differentiation into obstructive or central sleep apnea was performed. If RPG findings did not allow a clear distinction, the condition was termed nondifferentiable sleep apnea. The diagnosis of sleep apnea syndrome (SAS) required an AHI > 5 events/h and an ESS score exceeding 10. To rule out a cardiological cause for central sleep apnea, transthoracic echocardiography was conducted by a board-certified cardiologist from the University Hospital Bonn.
Sleep questionnaire
Each patient underwent an assessment using the ESS questionnaire [36]. This scale comprises eight questions with the aim to evaluate the likelihood of an individual dozing off or falling asleep during diverse daily activities. Scores on the ESS can range from 0 to 24. Scores of 10 or below were categorized as normal daytime sleepiness, scores above 10 were considered indicative of excessive, pathological daytime sleepiness.
Statistical analysis
Exploratory statistical calculations were performed using IBM SPSS 29.0 for Windows. Metric data were presented as mean (± standard deviation (SD)) if normality was assumed and as median (range) for skewed data. In contrast, categorical data were reported as frequencies and percentages. To analyze differences between several groups in terms of metric data, the independent samples t-test or Mann-Whitney U test was used, considering assumptions of normality and homogeneity of variances. To examine differences between binary groups when categorical data were available, the Chi-square test or in the case of small numbers Fisher’s exact test was applied. P < .05 was considered statistically significant. Kolmogorov-Smirnov test in conjunction with visual inspection of Q-Q diagrams and histograms were used to evaluate the normality of data distribution. The Levene test of equality of variances was used. Potential confounding factors were controlled by adjusting the inclusion criteria of the control patients according to age and gender. Missing data were handled using a complete case analysis, minimizing the impact of missing data on the results.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and has been reviewed and approved by the ethics committee of the University Hospital Bonn, Germany (reference number: 209/18). Written informed consent was obtained from every patient prior to inclusion in the study. Additionally, ethical considerations regarding the diagnosis and management of sleep-related breathing disorders in arthritis patients were carefully acknowledged and addressed.
Results
Patient characteristics
The study prospectively enrolled 39 arthritis patients: 22 with RA and 17 with PsA. Of these, 59.0% (23 patients) were male and 41.0% (16 patients) were female. The control group comprised 23 patients: 60.9% (14 patients) male and 39.1% (9 patients) female. Table 1 presents detailed demographics and characteristics.
Cardiorespiratory polygraphy
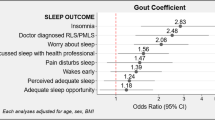
In the cohort of arthritis patients, 15 patients (38.5%) were diagnosed with sleep apnea with an AHI > 5 events/h. This included 45.5% of RA patients (10/22) and 29.4% of PsA patients (5/17). In the control group, 9 individuals (39.1%) exhibited sleep apnea (Fig. 1). Exemplary results from cardiorespiratory polygraphy testing are shown in Fig. 2. Detected risk factors for SRBD include male gender and higher age (Table 1). Comprehensive RPG results are depicted in Table 2. No significant differences were observed between the arthritis and control groups in these findings (p > .05). Results from transthoracic echocardiography did not reveal any clinically significant findings or differences related to the presence or absence of SRBD (data not shown).
Presence of sleep-related breathing disorders in rheumatoid arthritis patients, psoriatic arthritis patients and control patients: Distribution of sleep-related breathing disorders among patients with rheumatoid arthritis or psoriatic arthritis, and control patients. Within the arthritis cohort, 45.5% of rheumatoid arthritis and 29.4% of psoriatic arthritis patients were diagnosed with sleep-related breathing disorders, compared to 39.1% in the control group; abbrv.: RA: rheumatoid arthritis, PsA: psoriatic arthritis, SRBD: sleep-related breathing disorder
Sleep questionnaire
In the cohort of all 62 patients, the median ESS score was 7.5 (range: 0–18). RA patients exhibited a median ESS of 8.0 (range: 0–17), while the median score for PsA patients was 7.0 (range: 4–15). The control group reported a median ESS of 8.0 (range: 0–18). There was no significant association between the presence (RA/PsA patients) or absence (control patients) of rheumatic disease and ESS scores (p = .765).
Among patients with SRBD, the median ESS score was 9.0 (range: 0–18). Conversely, those with non-pathological RPG findings exhibited a median ESS score of 7.0 (range: 0–15) (p = .132) (Fig. 3). Excessive daytime sleepiness, defined by an ESS score > 10, was identified in 28.2% (11/39) of arthritis patients, 36.4% (8/22) in RA and 17.6% (3/17) in PsA, and in 21.7% (5/23) of controls. Among the 24 patients diagnosed with sleep apnea, 41.6% (10/24) had an ESS score > 10, with a significant difference observed between the subgroups: Seven RA patients, no PsA patient and three control group patients met the criteria for SAS (p = .017). A significant association was observed between excessive daytime sleepiness and the presence of SRBD as determined by RPG (p = .036).
Epworth Sleepiness Scale scores in patients with sleep-related breathing disorders: In patients diagnosed with sleep-related breathing disorder, the median Epworth Sleepiness Scale score was 9.0 (range: 0–18). Patients with non-pathological cardiorespiratory polygraphy exhibited a median Epworth Sleepiness Scale score of 7.0 (range 0–15) (p = .132); abbrv.: SRBD: sleep-related breathing disorder
Discussion
This study aimed to assess the prevalence of SRBD and associated risk factors in newly diagnosed, untreated RA or PsA patients. To our knowledge, this is the first analysis in this cohort, employing a multimodal approach with the ESS questionnaire for self-reported daytime sleepiness and the RPG for empirical sleep assessment. Furthermore, our objective was to develop a SRBD screening algorhythm for these two diseases, with the goal to improve early detection by clinicians and thereby enhance patient outcomes.
Previous research, largely cross-sectional studies utilizing self-reported questionnaires, have primarily explored sleep disorders among RA and PsA with chronic conditions experiencing general sleep disturbances [9,10,11, 4, 14, 15]. Musculoskeletal manifestations and associated pain have been identified as primary contributors to disrupted sleep [12, 13]. In our study, the ESS questionnaire was employed to assess these sleep disturbances [36]. No significant deviation in the ESS score was observed when comparing patients with RA or PsA to controls. Excessive daytime sleepiness was evident in 28.2% of arthritis patients (RA:36.4%; PsA: 17.6%) and 21.7% o controls.
The reduced prevalence of sleep disturbances observed in our study relative to existing research on RA [9,10,11] and PsA [4, 14,15,16] patients, and the absence of a statistically significant association between sleep disturbance prevalence and diagnosis as indicated by the ESS, may be attributed to our emphasis on investigating newly diagnosed patients. It’s well-established that sleep disturbances in patients with RA or PsA can origin from acute inflammation leading to pain and articular damage [12, 13]. Furthermore, fragmented sleep can exacerbate pain, engendering a vicious cycle [37]. Thus, while acute inflammation with subsequent pain may remain the primary contributor to reported sleep disturbances in our cohort, our focus on patients with first diagnosis excluded the potential contribution of post arthritis joint damage to sleep disturbances. This reiterates the importance of timely diagnosis and intervention in these diseases. With the advancement in therapeutic strategies, which proficiently reduce inflammation, there’s a likelihood that both sleep disturbances due to acute inflammation as well as sleep disturbances tied to joint damage might diminish over time. This could translate to a reduced prevalence of sleep disturbances. Future research would benefit from a longitudinal assessment of ESS questionnaires to track any emerging trends.
However, given the multifaceted nature of sleep disorders, a singular focus on inflammation-associated symptoms, subsequent pain, and self-reported daytime sleepiness falls short of encompassing the full spectrum of potential sleep disturbances in arthritis diseases. Few studies have investigated the prevalence of SRBD among individuals with RA or PsA before [30, 31, 26,27,28, 10, 9, 29]. A significant knowledge gap persists due to the absence of prospective, observational studies on the prevalence of SRBD in early-stage and newly diagnosed patients. An easily available and applicable screening instrument for SRBD is urgently needed. While polysomnography remains the gold-standart for diagnosing SRBD due to its sensitivity, its application has limits. It is notably time-intensive and requires considerable resources, including specialized expertise for accurate administration, assessment, and interpretation [10]. In contrast, RPG emerges as a more accessible, cost-effective, and expedient alternative, requiring less specialized knowledge for interpretation. RPG has been validated as an effective tool for screening, efficiently identifying individuals at heightened risk of SRBD, in particular suitable for primary care and outpatient settings [38]. Given these considerations, our study opted for the ESS and RPG, prioritizing ease of access, patient comfort, and adherence, as well as the pragmatic applicability in a clinical setting, providing valuable insights into the prevalence and risk factors of SRBD in newly diagnosed and untreated RA or PsA patients.
Employing RPG, our research revealed a 45.5% prevalence of SRBD in RA patients, which partially exceeds the prevalence reported in previous cross sectional studies. For instance, a meta-analysis conducted by Thakur et al. noted a 29.8% prevalence of SRBD among RA patients [29]. Importantly, there has been just one other prospective, albeit cross-sectional, study that has utilized empirical sleep assessment (polysomnography) to ascertain the prevalence of SRBD in RA, finding sleep apnea in 47.7% o the participants [39]. Literature on SRBD prevalence in PsA remains even more limited, with cross-sectional, self-reported sleep assessments being the primary method for examining the link between SRBD and PsA [30, 31]. Our research assesses SRBD among newly diagnosed and untreated patients with PsA, with our findings indicating a 29.4% prevalence ofSRBD in this cohort, the first report in this patient population.
To identify potential risk factors for SRBD in RA or PsA, we examined the relationship between demographic data and RPG findings. Existing literature has identified several risk factors for SRBD, including male gender, advancing age, obesity, smoking habits, and disease ativity [21, 22]. In alignment with these findings, our study indicates male gender and older age as significant risk indicators for SRBD in patients newly diagnosed with RA or PsA. Notably, our investigation found no substantial link between the duration of RA or PsA symptoms and SRBD occurrence. It’s important to recognize, however, that the relatively short median symptom duration of 6 months, as observed in our study group, might not be representative for disease experiences in regular RA and PsA patient.
In contrast, our study suggests possible links between smoking status, disease activity as reflected by DAS28CRP scores and BMI with the occurrence of SRBD, although these associations did not achieve statistical significance. The potential association between increased BMI and SRBD warrants particular focus, especially in the light of the link that recent research has revealed between rheumatological diseases, metabolic syndrome, and sleep apnea [40]. The presence of metabolic syndrome has been associated with a heightened risk of developing RA and PsA, further amplifying the risk of SRBD [41, 42]. Thus, central obesity, insulin resistance, dyslipidemia, and hypertension has been shown to contribute to upper airway obstruction and impaired respiratory function during sleep [43]. The reciprocal relationships between metabolic syndrome, arthritis, and sleep apnea need to be investigated in more detail to possibly decipher synergistic therapeutic approaches. Future large-scale studies are needed to confirm these risk factors for SRBD in newly diagnosed and untreated RA or PsA patients.
Comparing the ESS scores with RPG results, the ESS score was shown to be a reliable predictor for SRBD, revealing an association with RPG-identified SRBD. Moreover, we found that the occurrence of SAS, defined by an ESS score exceeding 10 combined with pathological RPG outcomes, was significantly more prevalent in RA patients than in PsA patients or the control group. Several hypotheses can be discussed regarding the observed epidemiological link between SAS and RA. Elevated levels of proinflammatory cytokines in patients with SRBD such as TNF-α, IL-6, IL-8, may exacerbate systemic inflammatory responses and, consequently, increase the vulnerability to RA [44,45,46,47]. Moreover, shared etiological factors such as genetic predispositon, environmental exposures, prevalent comorbidities, and lifestyle determinants might contribute to the noted association between RA and SRBD [48].
In conclusion, our study evaluates prevalence of SRBD in newly diagnosed, untreated RA or PsA patients in a multimodal approach. The ESS questionnaire and RPG have emerged as viable diagnostic tools, revealing a high prevalence of excessive daytime sleepiness and SRBD in this cohort. Moreover, ESS questionnaire serves as a valuable predictor for SRBD and SAS, which were frequently detected in our arthritis patients, particularly those with RA. Clinicians should be alert to the detected key risk factors for SRBD, especially male sex and older age above 55 years, considering the negative impact of SRBD on daily physical and cognitive functions. We advocate for the incorporation of routine ESS questionnaire and RPG screenings, as easy, cost-efficient diagnostic tools for all newly diagnosed RA or PsA patients. Such an approach ensures the timely identification and treatment of SRBD, significantly improving patient outcome.
While our study sheds light on the link between SRBD and RA or PsA, it also underscores the need for additional research due to several acknowledged limitations. One notable constraint is the potential restricted applicability of our results, stemming from single center recruitment of RA and PsA patients. This selection process might not fully represent the diversity of demographic characteristics and disease severity seen across broader populations, possibly influencing the reported prevalence and risk factors for SRBD and introducing selection bias. Furthermore, our study’s relatively modest sample size could diminish the statistical robustness of our findings, suggesting the necessity for future investigations with larger cohorts to validate our observations. Additionally, our analysis might not have comprehensively accounted for all conceivable confounding variables. Critical factors such as comorbid conditions (e.g., diabetes and hypertension), medication usage, socioeconomic factors, symptom duration, and neck circumference were not exhaustively evaluated and were not part of the exclusion criteria, which could compromise the reliability of our conclusions.
Future research should adopt a longitudinal framework to examine the evolution of SRBD following the initiation of treatment for RA or PsA. This perspective would allow for a detailed examination of the reciprocal influences between SRBD and arthritis progression over time. Furthermore, it remains to be clarified whether the sleep disturbances identified in our study are specific to RA and PsA, or if they manifest a common pattern across various forms of arthritis or autoimmune diseases, including the broader category of spondyloarthritis.
Related Congress Abstract Publication
Parts of this study were presented at the EULAR 2023 congress and have been published in the EULAR abstract supplement of the Annals of the Rheumatic Diseases [49].
Data availability
Data are available on reasonable request.
References
Michelsen B, Uhlig T, Sexton J et al (2018) Health-related quality of life in patients with psoriatic and rheumatoid arthritis: data from the prospective multicentre NOR-DMARD study compared with Norwegian general population controls. Ann Rheum Dis 77:1290–1294. https://doi.org/10.1136/annrheumdis-2018-213286
Holmqvist M, Ljung L, Askling J (2018) Mortality following new-onset rheumatoid arthritis: has modern Rheumatology had an impact? Ann Rheum Dis 77:85–91. https://doi.org/10.1136/annrheumdis-2017-212131
Gerhold K, Richter A, Schneider M et al (2015) Health-related quality of life in patients with long-standing rheumatoid arthritis in the era of biologics: data from the German biologics register RABBIT. Rheumatology (Oxford) 54:1858–1866. https://doi.org/10.1093/rheumatology/kev194
Haugeberg G, Lund Nilsen TI, Kavanaugh A et al (2021) Physical and psychosocial burden of psoriatic arthritis: Longitudinal Data from a Population-based study in Norway. Arthritis Care Res (Hoboken) 73:138–145. https://doi.org/10.1002/acr.24412
Michelsen B, Fiane R, Diamantopoulos AP et al (2015) A comparison of disease burden in rheumatoid arthritis, psoriatic arthritis and axial spondyloarthritis. PLoS ONE 10:e0123582. https://doi.org/10.1371/journal.pone.0123582
Finan PH, Goodin BR, Smith MT (2013) The association of sleep and pain: an update and a path forward. J Pain 14:1539–1552. https://doi.org/10.1016/j.jpain.2013.08.007
Wong ITY, Chandran V, Li S et al (2017) Sleep disturbance in Psoriatic Disease: Prevalence and Associated factors. J Rheumatol 44:1369–1374. https://doi.org/10.3899/jrheum.161330
Westhovens R, van der Elst K, Matthys A et al (2014) Sleep problems in patients with rheumatoid arthritis. J Rheumatol 41:31–40. https://doi.org/10.3899/jrheum.130430
Wolfe F, Michaud K, Li T (2006) Sleep disturbance in patients with rheumatoid arthritis: evaluation by medical outcomes study and visual analog sleep scales. J Rheumatol 33:1942–1951
Bourguignon C, Labyak SE, Taibi D (2003) Investigating sleep disturbances in adults with rheumatoid arthritis. Holist Nurs Pract 17:241–249. https://doi.org/10.1097/00004650-200309000-00005
Lyne L, Åkerstedt T, Alfredsson L et al (2022) Sleep problems in rheumatoid arthritis over 12 years from diagnosis: results from the Swedish EIRA study. RMD Open 8. https://doi.org/10.1136/rmdopen-2021-001800
An J, Nyarko E, Hamad MA (2019) Prevalence of comorbidities and their associations with health-related quality of life and healthcare expenditures in patients with rheumatoid arthritis. Clin Rheumatol 38:2717–2726. https://doi.org/10.1007/s10067-019-04613-2
Taylor PC, Moore A, Vasilescu R et al (2016) A structured literature review of the burden of illness and unmet needs in patients with rheumatoid arthritis: a current perspective. Rheumatol Int 36:685–695. https://doi.org/10.1007/s00296-015-3415-x
Husni ME, Merola JF, Davin S (2017) The psychosocial burden of psoriatic arthritis. Semin Arthritis Rheum 47:351–360. https://doi.org/10.1016/j.semarthrit.2017.05.010
Gossec L, de Wit M, Kiltz U et al (2014) A patient-derived and patient-reported outcome measure for assessing psoriatic arthritis: elaboration and preliminary validation of the psoriatic arthritis impact of Disease (PsAID) questionnaire, a 13-country EULAR initiative. Ann Rheum Dis 73:1012–1019. https://doi.org/10.1136/annrheumdis-2014-205207
Krajewska-Włodarczyk M, Owczarczyk-Saczonek A, Placek W (2018) Sleep disorders in patients with psoriatic arthritis and psoriasis. Reumatologia 56:301–306. https://doi.org/10.5114/reum.2018.79501
Gezer O, Batmaz İ, Sariyildiz MA et al (2017) Sleep quality in patients with psoriatic arthritis. Int J Rheum Dis 20:1212–1218. https://doi.org/10.1111/1756-185X.12505
Callis Duffin K, Wong B, Horn EJ et al (2009) Psoriatic arthritis is a strong predictor of sleep interference in patients with psoriasis. J Am Acad Dermatol 60:604–608. https://doi.org/10.1016/j.jaad.2008.10.059
Haugeberg G, Hoff M, Kavanaugh A et al (2020) Psoriatic arthritis: exploring the occurrence of sleep disturbances, fatigue, and depression and their correlates. Arthritis Res Ther 22:198. https://doi.org/10.1186/s13075-020-02294-w
Duvetorp A, Østergaard M, Skov L et al (2019) Quality of life and contact with healthcare systems among patients with psoriasis and psoriatic arthritis: results from the NORdic PAtient survey of psoriasis and psoriatic arthritis (NORPAPP). Arch Dermatol Res 311:351–360. https://doi.org/10.1007/s00403-019-01906-z
Young T, Palta M, Dempsey J et al (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235. https://doi.org/10.1056/NEJM199304293281704
Veasey SC, Rosen IM (2019) Obstructive sleep apnea in adults. N Engl J Med 380:1442–1449. https://doi.org/10.1056/NEJMcp1816152
Milleron O, Pillière R, Foucher A et al (2004) Benefits of obstructive sleep apnoea treatment in coronary artery disease: a long-term follow-up study. Eur Heart J 25:728–734. https://doi.org/10.1016/j.ehj.2004.02.008
Parish JM, Somers VK (2004) Obstructive sleep apnea and cardiovascular disease. Mayo Clin Proc 79:1036–1046. https://doi.org/10.4065/79.8.1036
Taylor-Gjevre RM, Nair BV, Gjevre JA (2013) Obstructive sleep apnoea in relation to rheumatic disease. Rheumatology (Oxford) 52:15–21. https://doi.org/10.1093/rheumatology/kes210
Hirsch M, Carlander B, Vergé M et al (1994) Objective and subjective sleep disturbances in patients with rheumatoid arthritis. A reappraisal. Arthritis Rheum 37:41–49. https://doi.org/10.1002/art.1780370107
Mahowald MW, Mahowald ML, Bundlie SR et al (1989) Sleep fragmentation in rheumatoid arthritis. Arthritis Rheum 32:974–983. https://doi.org/10.1002/anr.1780320806
Lavie P, Epstein R, Tzischinsky O et al (1992) Actigraphic measurements of sleep in rheumatoid arthritis: comparison of patients with low back pain and healthy controls. J Rheumatol 19:362–365
Thakur B, Pathak M, Singh P et al (2021) Prevalence of obstructive sleep apnea among patients with rheumatoid arthritis and its association with age and body mass index: a systematic review and meta-analysis. Int J Rheum Dis 24:1354–1361. https://doi.org/10.1111/1756-185X.14178
Yang Y-W, Kang J-H, Lin H-C (2012) Increased risk of psoriasis following obstructive sleep apnea: a longitudinal population-based study. Sleep Med 13:285–289. https://doi.org/10.1016/j.sleep.2011.07.018
Gupta MA, Simpson FC, Gupta AK (2016) Psoriasis and sleep disorders: a systematic review. Sleep Med Rev 29:63–75. https://doi.org/10.1016/j.smrv.2015.09.003
Cohen JM, Jackson CL, Li TY et al (2015) Sleep disordered breathing and the risk of psoriasis among US women. Arch Dermatol Res 307:433–438. https://doi.org/10.1007/s00403-015-1536-4
Aletaha D, Neogi T, Silman AJ et al (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum 62:2569–2581. https://doi.org/10.1002/art.27584
Coates LC, Kavanaugh A, Mease PJ et al (2016) Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol 68:1060–1071. https://doi.org/10.1002/art.39573
(1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Chung W-S, Lin C-L (2018) Sleep disorders associated with risk of rheumatoid arthritis. Sleep Breath 22:1083–1091. https://doi.org/10.1007/s11325-018-1639-1
Rundo JV (2019) Obstructive sleep apnea basics. Cleve Clin J Med 86:2–9. https://doi.org/10.3949/ccjm.86.s1.02
Fouda N, Dayem AA (2014) Obstructive sleep apnea in patients with rheumatoid arthritis: correlation with disease activity and pulmonary function tests. Egypt Rheumatologist 36:165–171. https://doi.org/10.1016/j.ejr.2014.04.002
Myasoedova E, Gabriel SE (2010) Cardiovascular disease in rheumatoid arthritis: a step forward. Curr Opin Rheumatol 22:342–347. https://doi.org/10.1097/BOR.0b013e3283379b91
Daïen CI, Tubery A, Beurai-Weber M et al (2019) Relevance and feasibility of a systematic screening of multimorbidities in patients with chronic inflammatory rheumatic diseases. Joint Bone Spine 86:49–54. https://doi.org/10.1016/j.jbspin.2018.03.016
Nurmohamed MT, Heslinga M, Kitas GD (2015) Cardiovascular comorbidity in rheumatic diseases. Nat Rev Rheumatol 11:693–704. https://doi.org/10.1038/nrrheum.2015.112
Zahnert T (2011) Schlafbezogene Atmungsstörungen (Sleep related breathing disorders). Laryngorhinootologie 90:691–707. https://doi.org/10.1055/s-0031-1293532
Chen W-S, Chang Y-S, Chang C-C et al (2016) Management and risk reduction of rheumatoid arthritis in individuals with obstructive sleep apnea: a Nationwide Population-based study in Taiwan. Sleep 39:1883–1890. https://doi.org/10.5665/sleep.6174
Nadeem R, Molnar J, Madbouly EM et al (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med 9:1003–1012. https://doi.org/10.5664/jcsm.3070
Alberti A, Sarchielli P, Gallinella E et al (2003) Plasma cytokine levels in patients with obstructive sleep apnea syndrome: a preliminary study. J Sleep Res 12:305–311. https://doi.org/10.1111/j.1365-2869.2003.00361.x
Ye J, Liu H, Zhang G et al (2012) The treg/th17 imbalance in patients with obstructive sleep apnoea syndrome. Mediators Inflamm 2012:815308. https://doi.org/10.1155/2012/815308
Shen T-C, Hang L-W, Liang S-J et al (2016) Risk of obstructive sleep apnoea in patients with rheumatoid arthritis: a nationwide population-based retrospective cohort study. BMJ Open 6:e013151. https://doi.org/10.1136/bmjopen-2016-013151
Winter L, Skowasch D, Weber M, AB0380 PREVALENCE OF SLEEP-RELATED BREATHING DISORDERS IN PATIENTS WITH RHEUMATOID ARTHRITIS, PSORIATIC ARTHRITIS, AND PERIPHERAL SPONDYLOARTHRITIS (062023). In: Scientific Abstracts. BMJ Publishing Group Ltd and European League Against Rheumatism, 1374.1–1374
Acknowledgements
None.
Funding
This is an independent, investigator-initiated study supported by Boehringer Ingelheim, Germany. Boehringer Ingelheim has no role in the design, analysis or interpretation of the results in this study; Boehringer Ingelheim was given the opportunity to review the manuscript for medical and scientific accuracy.
Patient and public involvement.
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conceptualization: SMP, LW, DS, VSS. Methodology: SMP, LW, DS, CB, VSS. Validation: SMP, LW, DS, CP, MW, DK, CB, CJB, VSS, Formal analysis: SMP, LW, CB, VSS. Investigation: SMP, LW, DS, CP, MW, DK, CJB, VSS. Resources: DS, MW, VSS. Data curation: SMP, LW, CB. Writing - Original Draft: SMP, LW, VSS. Writing - Review & Editing: SMP, LW, DS, CP, MW, DK, CB, CJB, VSS. Visualization: SMP, LW, DK, VSS. Supervision: DS, VSS. Project administration: DS, VSS. Funding acquisition: VSS.
Corresponding author
Ethics declarations
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and has been reviewed and approved by the ethics committee of the University Hospital Bonn, Germany (reference number: 209/18, approval date 06/18).
Statements and Declarations/ Competing interest:
All authors take full responsibility for the accuracy and integrity of all aspects of the work. The authors report no disclosures relevant to the manuscript.
Consent to participate
Informed consent was obtained from all subjects before enrollment.
Patient consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Petzinna, S.M., Winter, L., Skowasch, D. et al. Assessing sleep-related breathing disorders among newly diagnosed rheumatoid and psoriatic arthritis patients: a cross-sectional study. Rheumatol Int 44, 1025–1034 (2024). https://doi.org/10.1007/s00296-024-05610-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-024-05610-8