Abstract
Nurses have become integral members of multidisciplinary teams in managing rheumatic diseases, departing from their traditional patient care roles. This article provides a comprehensive review of nurses’ roles, interventions, and impacts in several rheumatic diseases, including rheumatoid arthritis, osteoarthritis, spondyloarthritis, gout, systemic lupus erythematosus, and polymyalgia rheumatica. It has been demonstrated that care under nursing supervision is effective and safe, with benefits including disease management, quality of life, and treatment adherence. In addition, nurses play a crucial role in promoting health, educating patients, and administering biological disease-modifying anti-rheumatic drugs. The COVID-19 pandemic has highlighted the significance of telehealth services and nurses’ role in delivering remote care. However, nursing education and training challenges persist, particularly in standardization and access to postgraduate education. Efforts to enhance the role of nurses in rheumatology care are necessary to optimize patient outcomes and meet the evolving needs of individuals with rheumatic diseases. Collaboration across healthcare institutions, professional groups, and educational facilities is necessary for promoting the continual growth and advancement of rheumatology nurse practice. By equipping nurses with the requisite knowledge, expertise, and resources to deliver top-notch care, we can enhance the well-being of individuals with rheumatic diseases and foster improved overall health outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nurses in modern health systems have undergone tremendous evolution, surpassing their basic patient care responsibilities [1]. The growth of nursing roles is especially noticeable in fields including Internal Medicine, Geriatrics, Rheumatology, and Rehabilitation, where nurses significantly impact the development and provision of complete healthcare services. An in-depth investigation is necessary to comprehend the extensive range and profound nature of nurses’ responsibilities in these domains [2,3,4,5]. This investigation should encompass the practices followed by institutions and the professional guidelines established by prominent healthcare organizations.
Specialist nurses are registered healthcare professionals who have accumulated experience in a particular area of nursing, obtained further nursing credentials, and have been authorized to work as experts with advanced knowledge in a specific clinical specialty. They have duties for conducting clinical practice, teaching, and consultation [6]. Specialist nurses offer instruction on the significance of nutrition, monitoring, weight management, dietary habits, and consistent use of drugs. They also educate patients on identifying indications of complications and give supportive services to aid patients in self-managing their clinical signs [7].
European League Against Rheumatism (EULAR) encourages rheumatology nurses to engage in close cooperation with the patient (including closest family members), the rheumatologist, and other members of the medical professional team, with a mutual emphasis on healthcare and results [8]. Studies conducted on patients with rheumatoid arthritis (RA) have demonstrated that nurse-led care is widely accepted, similarly efficient, and safe as physician-led care. Additionally, from the patient’s point of view, nurse-led care is convenient and easily reachable [9, 10]. The development and broad adoption of telehealth initiatives have the potential to create new opportunities for rheumatology nurses and improve accessibility [11].
Aim
This article investigates and illuminates nurses’ multifaceted roles in managing rheumatic disorders. It aims to investigate the evolution of nursing roles in rheumatic disease care, in which nurses play vital parts in patient care beyond their typical tasks. The study aims to assess nurses’ contributions to health promotion and patient education in rheumatology, particularly in promoting self-management and enhancing treatment adherence.
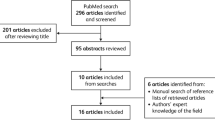
Search strategy
The relevant papers were acquired from Web of Science, Scopus, Medline/PubMed, Scopus, and DOAJ through a search using the terms “nurses” or “nurse specialists” or “physician-nurse relations” or “nurse-patient relations”, and “rheumatic diseases” or “rheumatology” or “arthritis” or “musculoskeletal diseases”. Only articles written in the English language were considered. No precise timeframe was determined. In addition, we thoroughly examined the references mentioned in the articles retrieved through our search methodology and chose the ones that we deemed pertinent. The search methodology was devised based on the criteria outlined by Gasparyan et al. [12].
Nurses involvement in the management of rheumatic diseases
Rheumatoid arthritis
Worldwide, the growing need for rheumatology services has forced the enhanced use of non-physician medical professionals, including rheumatology nurse specialists, to deliver care and support as part of a multidisciplinary team [13]. The current supply of rheumatologists is insufficient to meet the worldwide demand for rheumatology treatments, and this disparity is projected to deteriorate dramatically [14]. One strategy recommended to address the increasing need for rheumatologists is to utilize non-physician professionals, such as specialty nurses, more extensively within nurse-led care management [9].
In a study of active RA patients, participants were randomly assigned to nurse-led or physician-led care groups. Both groups exhibited substantial enhancement in disease activity, and there was no disparity in disease activity. This study demonstrated that nurse-led care is not inferior to traditional approaches for handling RA patients [15]. Dougados et al. [16] showed that the nurse-led approach had beneficial effects on managing comorbidities in RA. This study emphasized the advantages of introducing a program led by nurses to educate patients with RA. This program enhanced the identification and control of simultaneous medical conditions and enabled patients to track the severity of their illness.
Thurah et al. [17] performed a meta-analysis to compare nurse-led follow-up with the traditional strategy in patients with RA. The findings indicated that there was no discernible difference in disease activity after one year between the nurse-led follow-up and the conventional physician-led monitoring. The findings of a meta-analysis indicated that the nurse-led approach was beneficial for managing fatigue [18].
A randomized controlled clinical trial found that nurse-led care resulted in fewer unexpected hospitalizations and extra clinic appointments in RA patients than the usual strategy. Furthermore, the study discovered that the nurse-led strategy resulted in substantially lower overall expenses for RA treatment, laboratory testing, imaging, corticosteroid injections, and daily care visits [19].
Osteoarthritis
Osteoarthritis (OA) is the most common type of arthritis that is diagnosed on a global scale and is a major contributor to disability and diminished quality of life. Future forecasts indicate a substantial increase in the prevalence of OA as the population ages [20, 21]. Kangeswari et al. [22] assessed the efficacy of a nurse-led intervention in knee OA. The intervention group participants got personalized counseling through the use of cards and presentations in a total of six sessions conducted over six days. Exercise-related sessions were held following all educational counseling meetings. The study indicated that the nurse-led intervention improved the quality of life for patients with knee OA in all subscales. Based on these findings, the researchers conclude that a nurse-led intervention and education, which includes home isometric exercise, enhances the functional level and promotes the quality of life in patients with knee OA. This intervention was self-sufficient, suitable for utilization at home, economically efficient, and simply adjustable for patients with knee OA.
In a randomized controlled study, nurses administered ten sessions of instruction on pain-coping techniques to individuals suffering from chronic pain related to OA, and the control group continued with routine care [23]. The results confirmed the efficacy of pain coping strategies proposed by nurses. Implemented within a practical context, this method had a beneficial effect on pain caused by OA and other symptoms associated with OA.
Kwok et al. [24] examined the efficacy of a 60-minute consultation conducted by a specialized clinical nurse in individuals with hand OA during a rheumatology routine. The findings of this study indicate that a short consultation and phone conversation with a clinical nurse specialist, as a part of regular services, seem to enhance the physical aspect of health-related quality of life in hand OA. The expressed hand pain and disability, as evaluated by a specific indicator of hand function, remained unchanged following the consultation. Following the intervention, there was an observed increase in the utilization of assistive equipment and paracetamol. The majority of participants expressed satisfaction with the education.
Research findings indicate that nurse-led procedures have been shown to benefit individuals with OA. Nevertheless, the absence of standardization among procedures is remarkable. Hence, the establishment of standardized protocols would be more beneficial for OA patients.
Spondyloarthritis
Spondyloarthritis (SpA) is a comprehensive condition with several subtypes. While each subtype of SpA exhibits distinct clinical characteristics, there are shared clinical signs and comorbidities across all subtypes [25]. Different techniques are currently accessible for evaluating the activity of a disease, and the frequency of measures varies depending on the severity of the condition. In instances of significant disease activity, it is advisable to do more frequently scheduled examinations [26]. Nevertheless, conducting frequent assessments might pose challenges for physicians working in clinics with a large number of patients.
Molto et al. [27] assessed a nurse-led intervention for self-management and self-evaluation of disease severity in individuals with axial SpA (axSpA). The researchers developed an intervention that incorporated self-management techniques, a video tutorial with a series of gradually increasing exercises that can be done at home, and self-evaluation using a video that explains the value of closely tracking disease severity utilizing predefined tools. The nurse instructed the participants in the intervention group on how to obtain, compute, and submit the severity of the disorder. The control group was not provided with information regarding the significance of medical condition monitoring and were not given any educational resources on exercising. However, they were educated about the complications linked to comorbidities at the beginning of the study. While the primary endpoint (coping) did not show any statistical significance, there was substantial evidence favoring this program for the change in disease activity, frequency and length of home exercise sessions in the active group, and physical activity levels.
A randomized controlled clinical trial assessed the efficacy of a nurse-led intervention within a multidisciplinary care setting. The intervention group demonstrated superiority in disease activity, functional status, quality of life levels, and hospitalization compared to the control group [28].
Gout
Gout is a condition that involves abnormally high levels of uric acid and the buildup of crystals composed of monosodium urate. The prevalence of gout has been progressively rising in recent years [29]. The randomized controlled trial compared the nurse-led program and the standard outpatient follow-up. The program, guided by nurses, was linked to a significant increase in the acceptance of urate-lowering therapy and compliance with the treatment. A higher proportion of patients who received nurse-led care achieved serum urate levels < 360 µmol/L following two years compared to those who received standard care. The provision of gout care led by nurses was cost-effective compared to standard care [30]. Fuller et al. [31] delivered a questionnaire to follow-up gout patients and gathered data on nurse-led care. Subjects who had previously received nurse-led care for gout reported more satisfaction, increased knowledge about the disease, higher likelihood of receiving urate-lowering medicine, and less flare-ups in the preceding year compared to those who had received care led by physicians. Phang et al. [32] developed a telehealth program led by nurses to increase the dosage of urate-lowering treatment. Telemedicine led by nurses proved to be useful and secure for managing gout. The findings validated the advantage of telemedicine in enhancing healthcare accessibility and diminishing healthcare usage. A systematic review revealed that interventions conducted by nurses, such as education and coaching on lifestyle habits, resulted in enhanced compliance with treatment. In general, nurses are essential members of multidisciplinary groups and can significantly impact collaboration on decisions, objective establishment, patient guidance and education assistance, and the provision of suitable contacts [33].
Other inflammatory rheumatic diseases
A randomized controlled trial in systemic lupus erythematosus (SLE) evaluated the effectiveness of transitional care [34]. The transitional care lasted for 12 weeks. The program included four organized evaluations, associated interventions, and subsequent phone check-ins. Two nurses with a master’s degree and extensive expertise in the nursing field for SLE delivered all interventions. The group receiving transitional care showed considerably larger enhancements in self-care and quality of life compared to the group receiving standard care.
The long-term outcomes of a nurse-led education program in patients with inflammatory arthritis were evaluated. The findings indicated that patients experienced an enhancement in their ability to self-manage their condition during this five-year period; however, there was a slight decline in their physical functionality [35].
Mørk et al. [36] examined the efficacy of a nurse-led prednisolone reduction protocol in comparison to a conventional regimen in polymyalgia rheumatica (PMR) patients. During the first and second-year follow-ups, patients in the nurse-led care group were administered significantly lower dosages of prednisolone. During the second-year follow-up, a greater percentage of patients in the conventional regimen group were still receiving prednisolone treatment. The authors concluded that a rigorous and methodical approach to reducing the dosage of prednisolone was more beneficial than the typical treatment plan.
Health promotion and nurses in rheumatic and musculoskeletal diseases
Prior studies have demonstrated the beneficial impact of multidisciplinary care on patient outcomes in individuals with rheumatic and musculoskeletal disorders [37, 38]. Individuals with systemic rheumatic diseases have numerous obstacles, such as an uncertain disease trajectory, diverse clinical progression, restricted efficacy of therapy, and variety in symptom manifestation [39]. Nurses play various active roles in rheumatology, including monitoring adverse effects, performing disease-specific tools and questionnaires, providing intravenous drugs, and facilitating self-administration [40]. This could enhance health promotion efforts by alleviating the pressure on healthcare services and mitigating economic expenses. Additionally, it may result in favorable outcomes such as improved patient adherence, enhanced quality of life, and better self-management [41]. Another crucial role of nurses in rheumatic and musculoskeletal disorders is to educate patients and their families. In a systematic review, Wojeck et al. [42] investigated the evidence for nurse-led interventions in patients with autoimmune rheumatic diseases. They concluded that these interventions improved patients’ coping mechanisms, quality of life, and mental health.
In conclusion, nurses can contribute substantially to health promotion by assessing unmet needs in rheumatic and musculoskeletal disorders and identifying appropriate interventions, thereby ensuring the continuity and quality of the chronic care pathway.
Nurses and biotherapies
Biologic disease-modifying anti-rheumatic drugs (bDMARDs) have made notable progress in treating rheumatic diseases in recent years. Patients receiving bDMARDs may experience both favorable and adverse effects. A heightened susceptibility to infection is a prominent and well-documented negative consequence [43]. Therefore, EULAR recommends influenza and pneumococcal vaccination for patients using bDMARDs [44, 45]. Krasselt et al. [46] found that vaccination rates in RA patients were considerably lower than in the general population. It was thought that misconceptions about bDMARD use being a contraindication for vaccination may be related to these low vaccination rates. Beauvais et al. [47] conducted a multicentre randomized controlled trial to assess the impact of nurse-led education on safety skills in patients receiving bDMARD treatment. This study showed that the education group performed better in infection-related skills than the control group. Additionally, the education group displayed a higher inclination towards vaccination and exhibited better adherence to treatment protocols.
Another critical issue with biologic agents in clinical practice is adherence. Treatment noncompliance and non-persistence are linked to poor clinical outcomes and greater treatment costs [48, 49]. Rheumatology nurses can assist patients with drug adherence. Nurses can improve medication adherence by identifying plausible reasons for patients’ poor adherence, providing reminders as needed, and discussing negative perceptions about treatments [50].
Borras-Blasco et al. [51] administered a 2-hour educational session to patients with RA, psoriatic arthritis, and SpA, transitioning from utilizing prefilled syringes to auto-injector pens for injecting etanercept. Following the educational intervention, the proportion of patients who self-administered etanercept rose from 66 to 94%, whereas the proportion of patients seeking primary care for injection reduced from 23 to 2%. Larsson et al. [52] reported that switching from one of two annual rheumatologist visits to a nurse-led monitoring visit resulted in a considerable reduction in annual expenses for patients with chronic inflammatory arthritis in remission receiving biologic drugs. This can boost patients’ health by improving clinical outcomes while reducing societal costs by lowering disease economic impact. As a result, education delivered by specialized nurses can enhance treatment adherence while also providing significant cost savings for patients utilizing biological agents.
Nurse functions during the coronavirus disease 2019 (COVID-19) pandemic
The coronavirus disease 2019 (COVID-19) pandemic has not only affected many people around the world but has also severely impacted healthcare. Clinical approaches such as telemedicine were needed throughout the pandemic to prevent transmission and reduce the burden on healthcare systems. While the concept of telehealth services in rheumatology has been a topic of discussion for the past two decades, its utilization has significantly increased due to the COVID-19 pandemic. Several studies in the literature have examined the use of telemedicine in the context of inflammatory rheumatic diseases. In this research, well-planned, customized telerehabilitation regimens were found to have beneficial effects [11, 53]. Although telemedicine experiments during the pandemic time largely engaged physicians, the pandemic experiences revealed that we also need to boost the number and training of specialized rheumatology nurses [54]. In a randomized controlled trial, RA patients with low disease activity or in remission were randomly assigned to patient-reported outcome-based telehealth follow-up by a nurse or rheumatologist or typical outpatient follow-up by a physician. When the patients were evaluated 52 weeks afterward, patient-reported outcome-based telehealth follow-up and traditional outpatient follow-up were found to provide similar disease activity management. The study also found no difference in disease activity between the groups led by nurses and rheumatologists [55].
Telehealth can also be used to improve drug adherence via reminder texts or phone calls, as well as for patient education and counseling [56]. Nurses can conduct telephone or video calls to ensure patients’ active engagement in their care procedures and boost their treatment compliance. In their preliminary investigation, Ozkaraman et al. [57] documented that 37.5% of patients were not provided with information before receiving anti-TNF-α treatment. They also found that telephone nursing consultation did not alleviate the challenges faced by the patients, although it contributed to a partial improvement in treatment adherence. The small sample size is likely responsible for these results [50].
In conclusion, additional rigorous studies are required to expand nurses’ roles in rheumatology by including telehealth. As health systems gain valuable insights from these extraordinary situations, nurses should promptly develop innovative strategies by utilizing health technologies effectively. Telehealth should be integrated into the current curriculum to allow nurses to acquire the necessary expertise to provide secure and proficient healthcare.
Education of nurses
Establishing a multidisciplinary team in chronic rheumatic diseases is crucial for addressing the diverse requirements of patients, enhancing therapeutic efficacy, and improving treatment adherence. Rheumatology nurses play a crucial role in this multidisciplinary team. Specialized rheumatology nurses are responsible for performing intricate tasks such as evaluating disease activity, administering injections, and monitoring patient progress [58]. Nurses need access to continuing education to develop and maintain their knowledge and skills. However, standardization of education becomes difficult due to the differences in curricula in nursing education in different countries. In some countries, postgraduate education is planned so that rheumatology nurses can take a more active role in the follow-up and treatment of patients. Ryan et al. [59], in their study with nurses who received postgraduate education in rheumatology, reported that receiving postgraduate education increased self-confidence and new clinical and critical evaluation skills. Obtaining postgraduate education in rheumatology poses several challenges. Vlieland et al. [60] demonstrated that the primary obstacles to engaging in postgraduate education are limitations in time and financial resources. While the advantages of specialist rheumatology nurses in terms of clinical and economic gains are recognized, there are issues regarding education. A survey revealed that most rheumatology nurses participated in audits, but less than 25% had presented a poster, and even fewer had published research. The percentage of nurses authorized to write prescriptions is limited to 29%. Less than 20% of nurses received training in administering intra-articular injections or acquired proficiency in performing musculoskeletal ultrasonography [61].
To summarise, the prevalence and standardization of rheumatology nurses’ specialty training appear insufficient for the time being. Nurses should be encouraged to pursue postgraduate and extended education to achieve conformity with national standards and overcome any obstacles they face in doing so.
EULAR recommendations and perspectives
The current recommendations from EULAR emphasize the importance of rheumatology nurses working with patients, their families, rheumatologists, and other multidisciplinary team members. The goal is to provide comprehensive care and achieve positive outcomes. Patients should have access to a nurse to improve their knowledge and get needs-based education. Patients should have prompt access to a nurse for personalized assistance, which may include telemedicine services. The significance of nurses’ participation in complete disease care to regulate disease activity, mitigate signs, and enhance patient-preferred consequences has been underscored. This strategy is known to result in economical healthcare. Nurses need to address psychological issues and implement procedures to enhance self-management abilities [8].
The volatile characteristics of rheumatic conditions and emerging treatment alternatives occasionally necessitate prompt access to healthcare. Simultaneously, online consultations can facilitate distant care, providing opportunities for novel communication, support, and disease monitoring methods to be utilized [62]. Patients perceive telemedicine presented by nurses and online discussions as providing them with a sense of individualized assistance from a knowledgeable healthcare provider. The service’s quality is comparable to a physician’s typical follow-up to track disease activity [11, 63].
Patients have reported that the care nurses deliver can enhance their quality of life and boost healthcare satisfaction via extended and more comprehensive consultations [64]. Nurse-provided care has the potential to lower hospital admissions and reduce the overall cost of treatment while also improving team collaboration within the health system [65]. Patients highly value the proficiency of nurses, whereas the level of trust patients have in their physicians is the primary factor influencing their assessment of the significance of the care delivered by nurses [66].
Nurse-led interventions necessitate the self-sufficient execution of disease activity evaluations, health instruction, psychological care, and medical support. Hence, the incorporation of structured education and hands-on training in clinical settings is expected to bolster the responsibilities and skills of rheumatology nurses. Education regarding rheumatic disease handling should encompass theoretical and practical components [67]. The main roles of specialized nurses are visualized in Fig. 1.
Studies have demonstrated that interventions led by nurses in rheumatic diseases have yielded favorable outcomes in terms of treatment, clinical results, and healthcare expenses. However, there is a scarcity of rheumatology nurses in low-middle-income countries, as evidenced in Africa and Middle Eastern countries [13]. Hence, it would be beneficial to formulate innovative strategies and collaborative endeavors for countries under this category.
Conclusion
Nurses have advanced beyond traditional patient care roles to become essential to multidisciplinary teams, making major contributions to patient education, treatment adherence, and overall health care service. The evidence shows that nurse-led interventions enhance patient outcomes involving disease management, quality of life, and medication adherence across the rheumatic disease spectrum. Furthermore, nurses’ participation in health promotion and bDMARD treatment has been linked to improved patient safety, treatment adherence, and overall clinical results. The COVID-19 pandemic has highlighted the need for telehealth services, with nurses playing a pivotal role in remote care, disease monitoring, and patient support. As healthcare systems advance, it is critical to address nurse education and training issues to maintain consistent, high-quality care delivery across various environments and communities.
References
Hines ME (2017) Turning words into action: advancing the role of Advanced holistic nurses. J Holist Nurs 35:316–317. https://doi.org/10.1177/0898010117740067
Zhu Y, Zhang H, Xi Y, Zhu H, Lu Y, Luo X, Tang Z, Lei H (2024) The implication of diabetes-specialized nurses in Aiming for the Better Treatment and Management of Patients with Diabetes Mellitus: a brief narrative review. Diabetes Ther. https://doi.org/10.1007/s13300-024-01558-x
Woo BFY, Ng WM, Tan IF, Zhou W (2024) Practice patterns, role and impact of advanced practice nurses in stroke care: a mixed-methods systematic review. J Clin Nurs 33:1306–1319. https://doi.org/10.1111/jocn.16970
von der Lühe V, Roos M, Löbberding M et al (2023) Expanded nursing roles to promote person-centred care for people with cognitive impairment in acute care (ENROLE-acute): study protocol for a controlled clinical trial, process and economic evaluation. BMC Geriatr 23:858. https://doi.org/10.1186/s12877-023-04560-3
Hong C, Yan Q, Qi H, Zhang Y, Yu L, Dong L, Wang J (2024) Acceptability, Preferred Medium, and components of nurse-led Cardiac Telerehabilitation: a cross-sectional study. Clin Nurs Res 33:146–156. https://doi.org/10.1177/10547738241228634
Kerr H, Donovan M, McSorley O (2021) Evaluation of the role of the clinical nurse specialist in cancer care: an integrative literature review. Eur J Cancer Care (Engl) 30:e13415. https://doi.org/10.1111/ecc.13415
Happell B, Platania-Phung C, Watkins A, Scholz B, Curtis J, Goss J, Niyonsenga T, Stanton R (2019) Developing an evidence-based specialist nursing role to improve the Physical Health Care of people with Mental Illness. Issues Ment Health Nurs 40:832–838. https://doi.org/10.1080/01612840.2019.1584655
Bech B, Primdahl J, van Tubergen A et al (2020) 2018 update of the EULAR recommendations for the role of the nurse in the management of chronic inflammatory arthritis. Ann Rheum Dis 79:61–68. https://doi.org/10.1136/annrheumdis-2019-215458
Garner S, Lopatina E, Rankin JA, Marshall DA (2017) Nurse-led care for patients with rheumatoid arthritis: a systematic review of the Effect on Quality of Care. J Rheumatol 44:757–765. https://doi.org/10.3899/jrheum.160535
Vivienne L, Michael S (2018) Nurses’ roles in the management of chronic inflammatory arthritis: a systematic review. Rheumatol Int 38:2027–2036. https://doi.org/10.1007/s00296-018-4135-9
de Thurah A, Stengaard-Pedersen K, Axelsen M et al (2018) Tele-Health follow-up strategy for tight control of Disease Activity in Rheumatoid Arthritis: results of a Randomized Controlled Trial. Arthritis Care Res (Hoboken) 70:353–360. https://doi.org/10.1002/acr.23280
Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD (2011) Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 31:1409–1417. https://doi.org/10.1007/s00296-011-1999-3
Uthman I, Almoallim H, Buckley CD et al (2021) Nurse-led care for the management of rheumatoid arthritis: a review of the global literature and proposed strategies for implementation in Africa and the Middle East. Rheumatol Int 41:529–542. https://doi.org/10.1007/s00296-020-04682-6
Battafarano DF, Ditmyer M, Bolster MB et al (2018) 2015 American College of Rheumatology Workforce Study: supply and demand projections of adult rheumatology workforce, 2015–2030. Arthritis Care Res (Hoboken) 70:617–626. https://doi.org/10.1002/acr.23518
Hoeper JR, Zeidler J, Meyer SE et al (2021) Effect of nurse-led care on outcomes in patients with ACPA/RF-positive rheumatoid arthritis with active disease undergoing treat-to-target: a multicentre randomised controlled trial. RMD Open 7:e001627. https://doi.org/10.1136/rmdopen-2021-001627
Dougados M, Soubrier M, Perrodeau E et al (2015) Impact of a nurse-led programme on comorbidity management and impact of a patient self-assessment of disease activity on the management of rheumatoid arthritis: results of a prospective, multicentre, randomised, controlled trial (COMEDRA). Ann Rheum Dis 74:1725–1733. https://doi.org/10.1136/annrheumdis-2013-204733
de Thurah A, Esbensen BA, Roelsgaard IK, Frandsen TF, Primdahl J (2017) Efficacy of embedded nurse-led versus conventional physician-led follow-up in rheumatoid arthritis: a systematic review and meta-analysis. RMD Open 3:e000481. https://doi.org/10.1136/rmdopen-2017-000481
Sezgin MG, Bektas H (2022) The effect of nurse-led care on fatigue in patients with rheumatoid arthritis: a systematic review and meta-analysis of randomized controlled studies. J Clin Nurs 31:832–842. https://doi.org/10.1111/jocn.16003
Wang J, Zou X, Cong L, Liu H (2018) Clinical effectiveness and cost-effectiveness of nurse-led care in Chinese patients with rheumatoid arthritis: a randomized trial comparing with rheumatologist-led care. Int J Nurs Pract 24. https://doi.org/10.1111/ijn.12605
Kopec JA, Heath AJ, Sayre EC, Cibere J, Li LC, Marra CA, Liu RR, Esdaile JM (2022) Prevalence of joint-specific osteoarthritis and joint pain in British Columbia, Canada. Rheumatol Int 42:1623–1628. https://doi.org/10.1007/s00296-021-05031-x
Zhang W, Qiu Q, Sun B, Xu W (2021) A four-genes based diagnostic signature for osteoarthritis. Rheumatol Int 41:1815–1823. https://doi.org/10.1007/s00296-021-04795-6
Kangeswari P, Arulappan J (2022) Effectiveness of nurse-led intervention on quality of life of patients with knee osteoarthritis. J Patient Exp 9:23743735221098254. https://doi.org/10.1177/23743735221098254
Broderick JE, Keefe FJ, Bruckenthal P et al (2014) Nurse practitioners can effectively deliver pain coping skills training to osteoarthritis patients with chronic pain: a randomized, controlled trial. Pain 155:1743–1754. https://doi.org/10.1016/j.pain.2014.05.024
Kwok WY, Kloppenburg M, Beaart-van de Voorde LJ, Huizinga TW, Vliet Vlieland TP (2011) Role of rheumatology clinical nurse specialists in optimizing management of hand osteoarthritis during daily practice in secondary care: an observational study. J Multidiscip Healthc 4:403–411. https://doi.org/10.2147/JMDH.S25269
Duruöz MT, Bodur H, Ataman Ş et al (2024) Cross-sectional analysis of cardiovascular disease and risk factors in patients with spondyloarthritis: a real-life evidence from Biostar nationwide registry. Rheumatol Int 44:631–642. https://doi.org/10.1007/s00296-023-05523-y
Braun J, Krause D, Kiltz U (2021) The efficacy of a nurse-led interventional program to improve the health of patients with axial spondyloarthritis. Rheumatology (Oxford) 60:487–488. https://doi.org/10.1093/rheumatology/keaa639
Molto A, Gossec L, Poiraudeau S et al (2021) Evaluation of the impact of a nurse-led program of patient self-assessment and self-management in axial spondyloarthritis: results of a prospective, multicentre, randomized, controlled trial (COMEDSPA). Rheumatology (Oxford) 60:888–895. https://doi.org/10.1093/rheumatology/keaa480
Liang L, Pan Y, Wu D, Pang Y, Xie Y, Fang H (2019) Effects of Multidisciplinary Team-based nurse-led Transitional Care on clinical outcomes and quality of life in patients with Ankylosing Spondylitis. Asian Nurs Res (Korean Soc Nurs Sci) 13:107–114. https://doi.org/10.1016/j.anr.2019.02.004
Cox P, Gupta S, Zhao SS, Hughes DM (2021) The incidence and prevalence of cardiovascular diseases in gout: a systematic review and meta-analysis. Rheumatol Int 41:1209–1219. https://doi.org/10.1007/s00296-021-04876-6
Doherty M, Jenkins W, Richardson H et al (2018) Efficacy and cost-effectiveness of nurse-led care involving education and engagement of patients and a treat-to-target urate-lowering strategy versus usual care for gout: a randomized controlled trial. Lancet 392:1403–1412. https://doi.org/10.1016/S0140-6736(18)32158-5
Fuller A, Jenkins W, Doherty M, Abhishek (2020) Nurse-led care is preferred over GP-led care of gout and improves gout outcomes: results of Nottingham gout treatment trial follow-up study. Rheumatology (Oxford) 59:575–579. https://doi.org/10.1093/rheumatology/kez333
Phang KF, Santosa A, Low BPL, Tan PSH, Khong ZW, Lim AYN, Teng GG, Tay SH (2020) A nurse-led, rheumatologist-assisted telemedicine intervention for dose escalation of urate-lowering therapy in gout. Int J Rheum Dis 23:1136–1144. https://doi.org/10.1111/1756-185X.13855
Tsiamalou P, Brotis AG, Vrekou E et al (2023) The nurse’s role in managing gout in the modern era: a systematic review of the literature. Med Int (Lond) 3:40. https://doi.org/10.3892/mi.2023.100
Xie X, Song Y, Yang H, Nie A, Chen H, Li JP (2018) Effects of transitional care on self-care, readmission rates, and quality of life in adult patients with systemic lupus erythematosus: a randomized controlled trial. Arthritis Res Ther 20:184. https://doi.org/10.1186/s13075-018-1670-4
Grønning K, Lim S, Bratås O (2019) Health status and self-management in patients with inflammatory arthritis-A five-year follow-up study after nurse-led patient education. Nurs Open 7:326–333. https://doi.org/10.1002/nop2.394
Mørk C, Dam MY, Callsen MG, Keller KK (2021) The effect of a nurse-led prednisolone tapering regimen in polymyalgia rheumatica: a retrospective cohort study. Rheumatol Int 41:605–610. https://doi.org/10.1007/s00296-020-04654-w
Whittaker GA, Hill CL, Bradbury LA, Millner JR, Cliffe H, Bonanno DR, Kazantzis S, Menz HB (2024) Nursing and allied health workforce in Australian public rheumatology departments is inadequate: a cross-sectional observational study. Rheumatol Int 44:901–908. https://doi.org/10.1007/s00296-024-05547-y
Ndosi M, Ferguson R, Backhouse MR, Bearne L, Ainsworth P, Roach A, Dennison E, Cherry L (2017) National variation in the composition of rheumatology multidisciplinary teams: a cross-sectional study. Rheumatol Int 37:1453–1459. https://doi.org/10.1007/s00296-017-3751-0
Dollinger J, Neville C, Pineau CA, Vinet E, Hazel E, Lee JLF, Bernatsky S (2020) Challenges to optimal rheumatology care: a patient-centered focus group study. Clin Rheumatol 39:3083–3090. https://doi.org/10.1007/s10067-020-05091-7
Candelas G, Villaverde V, García S, Guerra M, León MJ, Cañete JD (2016) Benefit of health education by a training nurse in patients with axial and/or peripheral psoriatic arthritis: a systematic literature review. Rheumatol Int 36:1493–1506. https://doi.org/10.1007/s00296-016-3549-5
Kemppainen V, Tossavainen K, Turunen H (2013) Nurses’ roles in health promotion practice: an integrative review. Health Promot Int 28:490–501. https://doi.org/10.1093/heapro/das034
Wojeck RK, Arcoleo K, Hathaway EC, Somers TJ (2023) Nurse-led interventions in systemic autoimmune rheumatic diseases: a systematic review. BMC Nurs 22:232. https://doi.org/10.1186/s12912-023-01393-8
Konttinen L, Honkanen V, Uotila T et al (2006) Biological treatment in rheumatic diseases: results from a longitudinal surveillance: adverse events. Rheumatol Int 26:916–922. https://doi.org/10.1007/s00296-005-0097-9
Furer V, Rondaan C, Heijstek MW et al (2020) 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 79:39–52. https://doi.org/10.1136/annrheumdis-2019-215882
Luque Ramos A, Hoffmann F, Callhoff J, Zink A, Albrecht K (2016) Influenza and pneumococcal vaccination in patients with rheumatoid arthritis in comparison with age- and sex-matched controls: results of a claims data analysis. Rheumatol Int 36:1255–1263. https://doi.org/10.1007/s00296-016-3516-1
Krasselt M, Ivanov JP, Baerwald C, Seifert O (2017) Low vaccination rates among patients with rheumatoid arthritis in a German outpatient clinic. Rheumatol Int 37:229–237. https://doi.org/10.1007/s00296-016-3608-y
Beauvais C, Fayet F, Rousseau A et al (2022) Efficacy of a nurse-led patient education intervention in promoting safety skills of patients with inflammatory arthritis treated with biologics: a multicentre randomised clinical trial. RMD Open 8:e001828. https://doi.org/10.1136/rmdopen-2021-001828
Neycheva S, Naseva E, Batalov Z, Karalilova R, Batalov A (2023) Adherence to biological therapies in patients with rheumatoid arthritis: a retrospective cohort study. Rheumatol Int 43:1287–1296. https://doi.org/10.1007/s00296-023-05327-0
Maniadakis N, Toth E, Schiff M et al (2018) A targeted literature review examining Biologic Therapy Compliance and Persistence in Chronic Inflammatory diseases to identify the Associated Unmet needs, driving factors, and consequences. Adv Ther 35:1333–1355. https://doi.org/10.1007/s12325-018-0759-0
Melis MR, El Aoufy K, Bambi S et al (2023) Nursing interventions for patients with rheumatic and musculoskeletal diseases on biological therapies: a systematic literature review. Clin Rheumatol 42:1521–1535. https://doi.org/10.1007/s10067-023-06520-z
Borrás-Blasco J, Gracia-Pérez A, Casterá MD, Rosique-Robles JD, Abad J (2013) Educational session as a tool to increase patient satisfaction of switching etanercept from the prefilled syringe to the autoinjection pen. Expert Opin Biol Ther 13:1103–1108. https://doi.org/10.1517/14712598.2013.795942
Larsson I, Fridlund B, Arvidsson B, Teleman A, Svedberg P, Bergman S (2015) A nurse-led rheumatology clinic versus rheumatologist-led clinic in monitoring of patients with chronic inflammatory arthritis undergoing biological therapy: a cost comparison study in a randomised controlled trial. BMC Musculoskelet Disord 16:354. https://doi.org/10.1186/s12891-015-0817-6
Hormaza-Jaramillo A, Arredondo A, Forero E et al (2022) Effectiveness of Telemedicine compared with Standard Care for patients with rheumatic diseases: a systematic review. Telemed J E Health 28:1852–1860. https://doi.org/10.1089/tmj.2022.0098
Kocyigit BF, Assylbek MI, Yessirkepov M (2024) Telerehabilitation: lessons from the COVID-19 pandemic and future perspectives. Rheumatol Int 44:577–582. https://doi.org/10.1007/s00296-024-05537-0
El Aoufy K, Melis MR, Bellando Randone S et al (2022) The positive side of the coin: Sars-Cov-2 pandemic has taught us how much Telemedicine is useful as standard of care procedure in real life. Clin Rheumatol 41:573–579. https://doi.org/10.1007/s10067-021-05975-2
Song Y, Reifsnider E, Zhao S, Xie X, Chen H (2020) A randomized controlled trial of the effects of a telehealth educational intervention on medication adherence and disease activity in rheumatoid arthritis patients. J Adv Nurs 76:1172–1181. https://doi.org/10.1111/jan.14319
Ozkaraman A, Alparslan GB, Babadağ B, Kaşifoğlu T, Baydemir C (2018) Effect of education and telephone counseling on adherence to treatment and challenges experienced in anti-TNF-α treatment: a pilot study. Contemp Nurse 54:108–119. https://doi.org/10.1080/10376178.2017.1422776
Gall S, Kiltz U, Kobylinski T, Andreica I, Vaupel K, Waldecker C, Baraliakos X, Braun J (2022) Patient knowledge about biosimilars and satisfaction with the education provided by rheumatologists or nurse specialists in a biosimilar multiswitch scenario - the perception study. Semin Arthritis Rheum 57:152119. https://doi.org/10.1016/j.semarthrit.2022.152119
Ryan S, Hassell A, Paskins Z, Rule K, Brooks M, Tajuria G (2023) Rheumatology nurses’ perceptions of undertaking a postgraduate education programme: a phenomenological study. Musculoskelet Care 21:1571–1577. https://doi.org/10.1002/msc.1832
Vliet Vlieland TP, van den Ende CH, Alliot-Launois F et al (2016) Educational needs of health professionals working in rheumatology in Europe. RMD Open 2:e000337. https://doi.org/10.1136/rmdopen-2016-000337
Begum J, Nisar MK (2017) Training rheumatology nurse specialists: are we doing the job right? Eur J Rheumatol 4:234–235. https://doi.org/10.5152/eurjrheum.2017.16110
Grønning K, Skomsvoll JF, Rannestad T, Steinsbekk A (2012) The effect of an educational programme consisting of group and individual arthritis education for patients with polyarthritis–a randomised controlled trial. Patient Educ Couns 88:113–120. https://doi.org/10.1016/j.pec.2011.12.011
Primdahl J, Sørensen J, Horn HC, Petersen R, Hørslev-Petersen K (2014) Shared care or nursing consultations as an alternative to rheumatologist follow-up for rheumatoid arthritis outpatients with low disease activity–patient outcomes from a 2-year, randomized controlled trial. Ann Rheum Dis 73:357–364. https://doi.org/10.1136/annrheumdis-2012-202695
Grønning K, Midttun L, Steinsbekk A (2016) Patients’ confidence in coping with arthritis after nurse-led education; a qualitative study. BMC Nurs 15:28. https://doi.org/10.1186/s12912-016-0150-x
Morgan S, Yoder LH (2012) A concept analysis of person-centered care. J Holist Nurs 30:6–15. https://doi.org/10.1177/0898010111412189
Bednarek A, Klepacz R, Bodys-Cupak IE (2023) The role of the nurse in the care and management of patients with rheumatic diseases arising from the current EULAR recommendations: a Literature Review. Healthc (Basel) 11:2434. https://doi.org/10.3390/healthcare11172434
Wang Y, Chen Y, Liu H, Chen H, Liang Y (2024) Evaluation of nurse practitioners’ roles and competencies among rheumatology nurses: results of a national survey. Med (Baltim) 103:e36842. https://doi.org/10.1097/MD.0000000000036842
Funding
Not applicable.
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
Conceptualization: Dana Auyezkhankyzy, Umida Khojakulova, Marlen Yessirkepov, Ainur B. Qumar, Olena Zimba, Burhan Fatih Kocyigit, and Mazlum Serdar Akaltun; Data acquisition and review of the literature: Burhan Fatih Kocyigit, and Mazlum Serdar Akaltun; Interpretations: Dana Auyezkhankyzy, Umida Khojakulova, Marlen Yessirkepov, Ainur B. Qumar, Olena Zimba, Burhan Fatih Kocyigit, and Mazlum Serdar Akaltun; Writing – review and editing: Dana Auyezkhankyzy, Umida Khojakulova, Marlen Yessirkepov, Ainur B. Qumar, Olena Zimba, Burhan Fatih Kocyigit, and Mazlum Serdar Akaltun; Final approval: Dana Auyezkhankyzy, Umida Khojakulova, Marlen Yessirkepov, Ainur B. Qumar, Olena Zimba, Burhan Fatih Kocyigit, and Mazlum Serdar Akaltun.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Auyezkhankyzy, D., Khojakulova, U., Yessirkepov, M. et al. Nurses’ roles, interventions, and implications for management of rheumatic diseases. Rheumatol Int 44, 975–983 (2024). https://doi.org/10.1007/s00296-024-05603-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-024-05603-7