Abstract
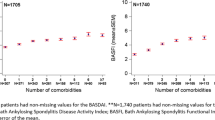
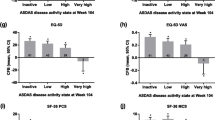
Global health (GH) and health-related quality of life are patient priorities in axial spondyloarthritis (axSpA). Our objective was to assess the relative importance of disease-related factors including disease activity, and patient-related factors including comorbidities, to explain GH in axSpA. Post hoc cross-sectional analyses of 4 sets (COMOSPA, PERSPA, COMEDSPA, and DESIR) of patients fulfilling ASAS criteria for axSpA. GH was assessed through the ASAS Health Index (ASAS-HI) or the EuroQoL-5D-3L (EQ-5D). Disease-related factors included disease activity (ASDAS, psoriasis, arthritis, enthesitis, and CRP), disease duration, diagnostic delay, bamboo spine, and treatment. Non-disease-related factors included sociodemographic characteristics, comorbidities and chronic widespread pain. Multivariable logistic and linear regressions and partial variances (R2) were applied to identify independent determinants of GH. In 6064 patients (range 284–2756 across datasets), mean age ranged 38.9–45.8 years, 51–68% were male. GH was generally moderate: median ASAS-HI ranged 5.0–7.0. GH was explained by ASDAS (range of odds ratios, OR, 2.60–4.48) and chronic widespread pain (range of OR 2.19–8.39); other determinants included comorbidities and sociodemographic characteristics. Only 47–57% of the total variance in GH could be explained by the models; disease activity (partial variance, 16–26%) and chronic widespread pain (partial variance 12–15%) were the key contributing variables. A wide range of disease and non-disease-related variables usually collected in studies could only explain 47–57% of the variability in GH. Among these, disease activity and chronic widespread pain were most relevant and of similar magnitude of importance. These findings will be helpful for shared decision-making.



Similar content being viewed by others
Data availability
Data that underlie the results presented here were shared from the 4 databases’ principal investigators. This data will be shared upon reasonable request while preserving patient anonymity. Researchers willing to use data collected during the study should contact the first author of the main manuscript of each study.
References
Kiltz U, Essers I, Hiligsmann M, Braun J, Maksymowych WP, Taylor WJ, van der Heijde D, Boonen A (2016) Which aspects of health are most important for patients with spondyloarthritis? A Best Worst Scaling based on the ASAS Health Index. Rheumatology (Oxford) 55(10):1771–1776. https://doi.org/10.1093/rheumatology/kew238
Navarro-Compán V, Sepriano A, El-Zorkany B, van der Heijde D (2021) Axial spondyloarthritis. Ann Rheum Dis 80(12):1511–1521. https://doi.org/10.1136/annrheumdis-2021-221035
Puyraimond-Zemmour D, Granger B, Molto A, Gaujoux-Viala C, Guillemin F, Ruyssen-Witrand A, Dougados M, Fautrel B, Gossec L (2019) Similar alteration for mental and physical aspects in health-related quality of life over 5 to 8 years in 1347 patients with early arthritis and early inflammatory back pain. Arthritis Res Ther 21(1):63. https://doi.org/10.1186/s13075-019-1841-y
Dean LE, Macfarlane GJ, Jones GT (2018) Five potentially modifiable factors predict poor quality of life in ankylosing spondylitis: results from the Scotland registry for ankylosing spondylitis. J Rheumatol 45(1):62–69. https://doi.org/10.3899/jrheum.160411
Elolemy G, Aboughanima A, Ganeb S, Elziat H (2020) Health-related quality of life in patients with ankylosing spondylitis: relationship with disease-related variables. Curr Rheumatol Rev 16(4):311–318. https://doi.org/10.2174/1573397115666191018162606
Kotsis K, Voulgari PV, Drosos AA, Carvalho AF, Hyphantis T (2014) Health-related quality of life in patients with ankylosing spondylitis: a comprehensive review. Expert Rev Pharmacoecon Outcomes Res 14(6):857–872. https://doi.org/10.1586/14737167.2014.957679
Carvalho PD, Ruyssen-Witrand A, Marreiros A, Machado PM (2022) Long-term association between disease activity and disability in early axial spondyloarthritis: results from a prospective observational study of inflammatory back pain. Arthritis Care Res 74(5):768–775. https://doi.org/10.1002/acr.24515
Fernández-Carballido C, Navarro-Compán V, Castillo-Gallego C, Castro-Villegas MC, Collantes-Estévez E, de Miguel E (2017) Disease activity as a major determinant of quality of life and physical function in patients with early axial spondyloarthritis. Arthritis Care Res 69(1):150–155. https://doi.org/10.1002/acr.22908
Kwan YH, Fong W, Leung YY, Lui NL, Tan CS, Malhotra R, Østbye T, Thumboo J (2019) Are extra-spinal symptoms associated with quality of life in patients with axial spondyloarthritis? A 1-year follow-up study. Clin Rheumatol 38(7):1881–1887. https://doi.org/10.1007/s10067-019-04514-4
Marzo-Ortega H, Navarro-Compán V, Akar S, Kiltz U, Clark Z, Nikiphorou E (2022) The impact of gender and sex on diagnosis, treatment outcomes and health-related quality of life in patients with axial spondyloarthritis. Clin Rheumatol 41(11):3573–3581. https://doi.org/10.1007/s10067-022-06228-6
Huang J-C, Qian B-P, Qiu Y, Wang B, Yu Y, Zhu Z-Z, Hu J, Qu Z (2017) Quality of life and correlation with clinical and radiographic variables in patients with ankylosing spondylitis: a retrospective case series study. BMC Musculoskelet Disord 18(1):352. https://doi.org/10.1186/s12891-017-1711-1
van der Meer R, Arends S, Kruidhof S, Bos R, Bootsma H, Wink F, Spoorenberg A (2022) Extraskeletal manifestations in axial spondyloarthritis are associated with worse clinical outcomes despite the use of tumor necrosis factor inhibitor therapy. J Rheumatol 49(2):157–164. https://doi.org/10.3899/jrheum.210308
Macfarlane GJ, Rotariu O, Jones GT, Pathan E, Dean LE (2020) Determining factors related to poor quality of life in patients with axial spondyloarthritis: results from the British Society for Rheumatology Biologics Register (BSRBR-AS). Ann Rheum Dis 79(2):202–208. https://doi.org/10.1136/annrheumdis-2019-216143
Moltó A, Etcheto A, van der Heijde D, Landewé R, van den Bosch F, Bautista Molano W, Burgos-Vargas R, Cheung PP, Collantes-Estevez E, Deodhar A, El-Zorkany B, Erdes S, Gu J, Hajjaj-Hassouni N, Kiltz U, Kim T-H, Kishimoto M, Luo S-F, Machado PM et al (2016) Prevalence of comorbidities and evaluation of their screening in spondyloarthritis: results of the international cross-sectional ASAS-COMOSPA study. Ann Rheumatic Dis 75(6):1016–1023. https://doi.org/10.1136/annrheumdis-2015-208174
Redeker I, Hoffmann F, Callhoff J, Haibel H, Sieper J, Zink A, Poddubnyy D (2018) Determinants of psychological well-being in axial spondyloarthritis: an analysis based on linked claims and patient-reported survey data. Ann Rheum Dis 77(7):1017–1024. https://doi.org/10.1136/annrheumdis-2017-212629
Macfarlane GJ, Barnish MS, Pathan E, Martin KR, Haywood KL, Siebert S, Packham J, Atzeni F, Jones GT (2017) Co-occurrence and characteristics of patients with axial spondyloarthritis who meet criteria for fibromyalgia: results from a UK National Register. Arthritis Rheumatol (Hoboken, NJ) 69(11):2144–2150. https://doi.org/10.1002/art.40185
Duffield SJ, Miller N, Zhao S, Goodson NJ (2018) Concomitant fibromyalgia complicating chronic inflammatory arthritis: a systematic review and meta-analysis. Rheumatology (Oxford) 57(8):1453–1460. https://doi.org/10.1093/rheumatology/key112
Tournadre A, Pereira B, Lhoste A, Dubost JJ, Ristori JM, Claudepierre P, Dougados M, Soubrier M (2013) Differences between women and men with recent-onset axial spondyloarthritis: results from a prospective multicenter French cohort. Arthritis Care Res 65(9):1482–1489. https://doi.org/10.1002/acr.22001
Hollick RJ, Stelfox K, Dean LE, Shim J, Walker-Bone K, Macfarlane GJ (2020) Outcomes and treatment responses, including work productivity, among people with axial spondyloarthritis living in urban and rural areas: a mixed-methods study within a national register. Ann Rheum Dis 79(8):1055–1062. https://doi.org/10.1136/annrheumdis-2020-216988
Machado P, Landewé R, Braun J, Hermann K-GA, Baraliakos X, Baker D, Hsu B, van der Heijde D (2011) A stratified model for health outcomes in ankylosing spondylitis. Ann Rheum Dis 70(10):1758–1764. https://doi.org/10.1136/ard.2011.150037
López-Medina C, Garrido-Castro JL, Castro-Jiménez J, González-Navas C, Calvo-Gutiérrez J, Castro-Villegas MC, Ortega-Castro R, Escudero-Contreras A, Font-Ugalde P, Collantes-Estévez E (2018) Evaluation of quality of life in patients with axial spondyloarthritis and its association with disease activity, functionality, mobility, and structural damage. Clin Rheumatol 37(6):1581–1588. https://doi.org/10.1007/s10067-018-4112-4
Dougados M, Etcheto A, Molto A, Alonso S, Bouvet S, Daurès J-P, Landais P, d’Agostino M-A, Berenbaum F, Breban M, Claudepierre P, Combe B, Fautrel B, Feydy A, Goupille P, Richette P, Pham T, Roux C, Treluyer J-M et al (2015) Clinical presentation of patients suffering from recent onset chronic inflammatory back pain suggestive of spondyloarthritis: the DESIR cohort. Joint Bone Spine 82(5):345–351. https://doi.org/10.1016/j.jbspin.2015.02.006
Molto A, Gossec L, Poiraudeau S, Claudepierre P, Soubrier M, Fayet F, Wendling D, Gaudin P, Dernis E, Guis S, Pouplin S, Ruyssen-Witrand A, Chales G, Mariette X, Beauvais C, Combe B, Flipo R-M, Richette P, Chary-Valckenaere I et al (2021) Evaluation of the impact of a nurse-led program of patient self-assessment and self-management in axial spondyloarthritis: results of a prospective, multicentre, randomized, controlled trial (COMEDSPA). Rheumatology (Oxford) 60(2):888–895. https://doi.org/10.1093/rheumatology/keaa480
López-Medina C, Molto A, Sieper J, Duruöz T, Kiltz U, Elzorkany B, Hajjaj-Hassouni N, Burgos-Vargas R, Maldonado-Cocco J, Ziade N, Gavali M, Navarro-Compan V, Luo S-F, Monti S, Tae-Jong K, Kishimoto M, Pimentel-Santos FM, Gu J, Schiotis R et al (2021) Prevalence and distribution of peripheral musculoskeletal manifestations in spondyloarthritis including psoriatic arthritis: results of the worldwide, cross-sectional ASAS-PerSpA study. RMD Open 7(1):e001450. https://doi.org/10.1136/rmdopen-2020-001450
Kiltz U, van der Heijde D, Boonen A, Akkoc N, Bautista-Molano W, Burgos-Vargas R, Wei JC-C, Chiowchanwisawakit P, Dougados M, Duruoz MT, Elzorkany BK, Gaydukova I, Gensler LS, Gilio M, Grazio S, Gu J, Inman RD, Kim T-J, Navarro-Compan V et al (2018) Measurement properties of the ASAS Health Index: results of a global study in patients with axial and peripheral spondyloarthritis. Ann Rheum Dis 77(9):1311–1317. https://doi.org/10.1136/annrheumdis-2017-212076
Euroqol User Guide https://www.euroqol.org/publications/user-guides
Kiltz U, van der Heijde D, Boonen A, Cieza A, Stucki G, Khan MA, Maksymowych WP, Marzo-Ortega H, Reveille J, Stebbings S, Bostan C, Braun J (2015) Development of a health index in patients with ankylosing spondylitis (ASAS HI): final result of a global initiative based on the ICF guided by ASAS. Ann Rheum Dis 74(5):830–835. https://doi.org/10.1136/annrheumdis-2013-203967
Boonen A, Braun J, van der Horst Bruinsma IE, Huang F, Maksymowych W, Kostanjsek N, Cieza A, Stucki G, van der Heijde D (2010) ASAS/WHO ICF Core Sets for ankylosing spondylitis (AS): how to classify the impact of AS on functioning and health. Ann Rheum Dis 69(1):102–107. https://doi.org/10.1136/ard.2008.104117
Atagündüz P, Kiraz S, Akar S, Küçükşahin O, Erden A, Aksoy A, Coşkun BN, Yağiz B, Bes C, Alpay Kanitez N, Kilic L, Karadağ Ö, Kaşifoğlu T, Emmungil H, Cinar M, Kimyon G, Yazisiz V, Ateş A, Ersözlü D et al (2023) Clinical and laboratory factors associated with bamboo spine in patients with axial spondyloarthritis: are there clues for bamboo spine. Clin Exp Rheumatol 41(3):620–627. https://doi.org/10.55563/clinexprheumatol/eb1zpo
Navarro-Compán V, Boel A, Boonen A, Mease P, Landewé R, Kiltz U, Dougados M, Baraliakos X, Bautista-Molano W, Carlier H, Chiowchanwisawakit P, Dagfinrud H, de Peyrecave N, El-Zorkany B, Fallon L, Gaffney K, Garrido-Cumbrera M, Gensler LS, Haroon N et al (2021) The ASAS-OMERACT core domain set for axial spondyloarthritis. Semin Arthritis Rheum 51(6):1342–1349. https://doi.org/10.1016/j.semarthrit.2021.07.021
Stolwijk C, Essers I, van den Bosch F, Dougados M, Etcheto A, van der Heijde D, Landewé R, Molto A, van Tubergen A, Boonen A, ASAS-COMOSPA study group (2020) Validation of the self-administered comorbidity questionnaire adjusted for spondyloarthritis: results from the ASAS-COMOSPA study. Rheumatology (Oxford) 59(7):1632–1639. https://doi.org/10.1093/rheumatology/kez482
England BR, Sayles H, Mikuls TR, Johnson DS, Michaud K (2015) Validation of the rheumatic disease comorbidity index. Arthritis Care Res 67(6):865–872. https://doi.org/10.1002/acr.22456
Santos-Faria D, Dougados M, Gossec L, Perrot S, Moltó A (2019) Evaluation of the performance of extreme patient-reported outcomes as surrogate markers for fibromyalgia in axial spondyloarthritis. Rheumatol Int 39(1):141–146. https://doi.org/10.1007/s00296-018-4200-4
Drouet J, López Medina C, Molto A, Granger B, Fautrel B, Gaujoux Viala C, Kiltz U, Dougados M, Gossec L (2023) Defining poor global functioning and health in axial spondyloarthritis, using the EQ-5D-3L questionnaire, when the ASAS-health index is not available is feasible. An analysis of 2651 patients from the PERSPA Study [abstract]. Arthritis Rheumatol 75 (suppl 9). https://www.acrabstracts.org/abstract/defining-poor-global-functioning-and-health-in-axial-spondyloarthritis-using-the-eq-5d-3l-questionnaire-when-the-asas-health-index-is-not-available-is-feasible-an-analysis-of-2651-patients-from-the/. Accessed February 22, 2024
Song Y, Chen H (2021) Predictors of health-related quality of life in patients with ankylosing spondylitis in Southwest China. Patient Prefer Adherence 15:1887–1894. https://doi.org/10.2147/PPA.S324097
Kwan YH, Fong W, Tan VIC, Lui NL, Malhotra R, Østbye T, Thumboo J (2017) A systematic review of quality-of-life domains and items relevant to patients with spondyloarthritis. Semin Arthritis Rheum 47(2):175–182. https://doi.org/10.1016/j.semarthrit.2017.04.002
Kiltz U, van der Heijde D, Boonen A, Bautista-Molano W, Burgos-Vargas R, Chiowchanwisawakit P, Duruoz T, El-Zorkany B, Essers I, Gaydukova I, Géher P, Gossec L, Grazio S, Gu J, Khan MA, Kim TJ, Maksymowych WP, Marzo-Ortega H, Navarro-Compán V et al (2016) Measuring impairments of functioning and health in patients with axial spondyloarthritis by using the ASAS Health Index and the Environmental Item Set: translation and cross-cultural adaptation into 15 languages. RMD Open 2(2):e000311. https://doi.org/10.1136/rmdopen-2016-000311
Landewé RBM, van der Heijde D (2021) Use of multidimensional composite scores in rheumatology: parsimony versus subtlety. Ann Rheum Dis 80(3):280–285. https://doi.org/10.1136/annrheumdis-2020-216999
Kiltz U, Wiatr T, Redeker I, Baraliakos X, Fedorov K, Braun J (2022) Effects of patient and disease characteristics on global functioning in patients with axial spondyloarthritis in routine care. Semin Arthritis Rheum 55:152006. https://doi.org/10.1016/j.semarthrit.2022.152006
Ramiro S, Nikiphorou E, Sepriano A, Ortolan A, Webers C, Baraliakos X, Landewé RBM, Van den Bosch FE, Boteva B, Bremander A, Carron P, Ciurea A, van Gaalen FA, Géher P, Gensler L, Hermann J, de Hooge M, Husakova M, Kiltz U et al (2022) ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis. https://doi.org/10.1136/ard-2022-223296
Carvalho PD, Vieira-Sousa E, Hmamouchi I, Marreiros A, Machado PM (2022) Determinants of health-related quality of life in spondyloarthritis and rheumatoid arthritis—data from the COMOSPA and COMORA studies. Semin Arthritis Rheum 57:152086. https://doi.org/10.1016/j.semarthrit.2022.152086
Soni A, Nishtala R, Ng S, Barnett R, Chyou T-Y, Cavill C, Sengupta R (2022) The natural history of chronic widespread pain in patients with axial spondyloarthritis: a cohort study with clinical and self-tracking data. Rheumatology (Oxford). https://doi.org/10.1093/rheumatology/keac679
Fan A, Tournadre A, Pereira B, Tatar Z, Couderc M, Malochet-Guinamand S, Mathieu S, Soubrier M, Dubost J-J (2016) Performance of Fibromyalgia Rapid Screening Tool (FiRST) to detect fibromyalgia syndrome in rheumatic diseases. Rheumatology (Oxford) 55(10):1746–1750. https://doi.org/10.1093/rheumatology/kew244
Desthieux C, Molto A, Granger B, Saraux A, Fautrel B, Gossec L (2016) Patient-physician discordance in global assessment in early spondyloarthritis and its change over time: the DESIR cohort. Ann Rheum Dis 75(9):1661–1666. https://doi.org/10.1136/annrheumdis-2015-208251
Lu Y, Dai Z, Lu Y, Chang F (2022) Effects of bDMARDs on quality of life in patients with psoriatic arthritis: meta-analysis. BMJ Open 12(4):e058497. https://doi.org/10.1136/bmjopen-2021-058497
Benavent D, Capelusnik D, Ramiro S, Molto A, López-Medina C, Dougados M, Navarro-Compán V (2022) Does gender influence outcome measures similarly in patients with spondyloarthritis? Results from the ASAS-perSpA study. RMD Open 8(2):e002514. https://doi.org/10.1136/rmdopen-2022-002514
Acknowledgements
The first author (JD) has received a Master Grant from Société Française de Rhumatologie (n° 4281) for the present analyses. The 4 datasets were available without financial compensation. The ASAS PERSPA study was conducted under the umbrella of ASAS with unrestricted grants from AbbVie, Pfizer, Lilly, Novartis, UCB, Janssen and Merck. The COMOSPA study was conducted under the umbrella of ASAS, with unrestricted grants from Abbvie, Pfizer and UCB. The COMEDSPA trial was conducted with an unrestricted grant from Abbvie. The DESIR cohort is conducted with Assistance Publique-Hopitaux de Paris (AP-HP, Paris France) as the sponsor, with the support of unrestricted grants from Pfizer France. The DESIR cohort is conducted under the control of Assistance publique Hopitaux de Paris via the Clinical Research Unit Paris Centre and under the umbrella of the French Society of Rheumatology and Institut national de la sante et de la recherche medicale (Inserm). Database management was performed within the Department of Epidemiology and Biostatistics (Dr Pascale FABBRO-PERAY, D.I.M., and Nımes, France). We also thank the investigators: Pr Maxime Dougados, Pr André Kahan, Dr Julien Wipff and Dr Anna Molto (Paris-Cochin), Pr Olivier Meyer, Pr Philippe Dieudé (Paris-Bichat), Pr Pierre Bourgeois, Pr Laure Gossec (Paris-La Pitie-Salpétriere), Pr Francis Berenbaum (Paris-Saint-Antoine), Pr Pascal Claudepierre (Creteil), Pr Maxime Breban, Pr Maria-Antonietta D’Agostino, Pr Félicie Costantino (Boulogne-Billancourt), Pr Michel De Bandt, Dr Bernadette Saint-Marcoux (Aulnay-sous-Bois), Pr Philippe Goupille (Tours), Pr Jean-Françis Maillefert (Dijon), Pr Xavier Puechal, Dr Emmanuelle Dernis (Le Mans), Pr Daniel Wendling, Pr Clément Prati (Besançon), Pr Bernard Combe, Pr Cédric Lukas (Montpellier), Pr Liana Euller-Ziegler, Pr Véronique Breuil (Nice), Pr Pascal Richette (Paris Lariboisière), Pr Pierre Lafforgue, Pr Thao Pham (Marseille), Pr Patrice Fardellone, Dr Patrick Boumier, Dr Pauline Lasselin (Amiens), Pr Jean-Michel Ristori, Pr Martin Soubrier, Pr Anne Tournadre (Clermont-Ferrand), Dr Nadia Mehsen (Bordeaux), Pr Damien Loeuille (Nancy), Pr Rene-Marc Flipo (Lille), Pr Alain Saraux (Brest), Pr Corinne Miceli, Dr Stephan Pavy (Le Kremlin-Bicêtre), Pr Alain Cantagrel, Pr Adeline Ruyssen-Witrand (Toulouse), Pr Olivier Vittecoq, Pr Thierry Lequerre (Rouen).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
JD, CLM, BF, MD, CGV declare that they have no competing interests relevant to this study. Benjamin Granger has received consultancy fees from MSD, and Boston scientific. Robert Landewé: Speaker fees/honoraria or research support from AbbVie, Eli-Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer and UCB. Anna Molto: Speaker honoraria/participated in advisory boards for AbbVie, Biogen, Janssen, Lilly, Gilead, Galapagos, Pfizer and UCB; Research grants from Pfizer and UCB. Uta Kiltz: Dr. Kiltz has received grant and research support and consultancy fees from AbbVie, Amgen, Biocad, Biogen, BMS, Chugai, Eli Lilly, Fresenius, Gilead, Grünenthal, GSK, Hexal, Janssen, MSD, Novartis, onkowissen.de, Pfizer, Roche, UCB and Viatris. Laure Gossec: research grants: AbbVie, Biogen, Lilly, Novartis, UCB; consulting fees: AbbVie, Amgen, BMS, Celltrion, Galapagos, Janssen, Lilly, MSD, Novartis, Pfizer, Sandoz, UCB.
Ethical approval
Ethical approvals were obtained from CPP Ile de France III for DESIR (2007, number P070302), COMEDSPA (2014, number 2014-A01215-42), and COMOSPA (2012, number 2012-A01357-36). For PERSPA, ethics approvals were obtained from local ethical committees. Argentina: Comité de Docencia e Investigaciones Hospital de Clinicas Dr. Nicolás Avellaneda; Canada: Health Reserach Ethics Board University of Alberta and Alberta Health Services; Chile: Comité ético-Científico Servicio Salud Metropolitano Sur Oriente; China: Ethics committee Third Affiliated Hospital of Sun Yat-sen University; Colombia: Comité de Ética en Investigación del Hospital Militar Central; Egypt: Research Ethics Committee Cairo University Faculty of Medicine; France: Comité de protection des personnes Ile de France III; Germany: Ethics Committee from the medical council Westphalia-Lippe and the Westphalian Wilhelms University; Hungary: Ethics Committee Semmelweis Egyetem Hospital; India: NHL Institutional Review Board (NHLIRB). SMT NHL Municipal Medical College; Italy: Comitato Etico Pavia; Japan: Ethics Committee St Luke’s International University; Lebanon: Comité d’éthique Hotel-Dieu de France; Mexico: Comité de Investigación Hospital General de México Eduardo Liceaga; Morocco: Comité d’Éthique pour la Recherche Biomédicale de Rabat; The Netherlands: Commissie Medische Ethiek Leids Universitair Medisch Centrum; Portugal: Comissão de Ética para a Saúde do Centro Hospitalar de Lisboa Ocidental; Romania: Comisia de Etica UMF Iuliu Hatieganu Cluj Napoca; South Korea: Ethics Committee Chonnam National University Medical School from Gwangju; Spain: Comité de Ética de la Investigación con Medicamentos, Hospital Universitario La Paz; Taiwan: Chang Gung Medical Foundation Institutional Review Board; Turkey: Marmara University School of Medicine Clinical Research Ethics Committee; USA: Metrohealth Institutional Revew Board. Written informed consent was obtained from all subjects before enrollment in all studies.
Related congress abstract
This work was previously presented in the ACR congress in 2023: Drouet J, López Medina C, Granger B, Fautrel B, Molto A, Gaujoux Viala C, Kiltz U, Dougados M, Gossec L. Disease Activity and Widespread Pain Are the 2 Key Drivers of Global Health in Axial Spondyloarthritis, with Similar Findings in Different Patient Populations: An Analysis of 4 Databases and 6064 Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/disease-activity-and-widespread-pain-are-the-2-key-drivers-of-global-health-in-axial-spondyloarthritis-with-similar-findings-in-different-patient-populations-an-analysis-of-4-databases-and-6064-pati/. Accessed February 22, 2024.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Drouet, J., López-Medina, C., Granger, B. et al. Disease activity and widespread pain are main contributors to patient-reported global health in axial spondyloarthritis: an analysis of 6064 patients. Rheumatol Int (2024). https://doi.org/10.1007/s00296-024-05576-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00296-024-05576-7