Abstract
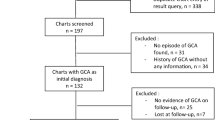
Prompt initiation of pulse glucocorticoid treatment is recommended in case of visual symptoms and suspected or proven giant cell arteritis (GCA). Pulse treatment in most cases prevents involvement of an initially unaffected fellow eye. We present the case of a biopsy-proven GCA in a 79-year-old man, complicated by sequential bilateral blindness. Initial unilateral vision loss was treated by 1 g methylprednisolone intravenously for 3 days, followed by 1 g/kg prednisone daily. Despite treatment, the second eye went completely blind 11 days after the initial vision loss. We performed a systematic search on Medline and Scopus aiming at identifying all cases of GCA complicated with loss of vision in a previously unaffected eye under pulse treatment for initially monocular vision loss. We identified 11 articles reporting 21 patients that met our inclusion criteria. Contralateral vision loss occurred 1–12 days following treatment initiation, with a median of 2 days. Treatment initiation was delayed up to 8 days since the initial vision loss, with a median delay of 2 days. Anterior ischemic optic neuropathy was the dominant mechanism of vision loss. Sequential involvement of the fellow eye in case of unilateral vision loss in GCA is rare. With 12-day interval being the longest reported, we conclude that even though the first 2 days are the most critical for the visual outcome, blindness in the initially unaffected eye may rarely occur later. Nonetheless, immediate initiation of pulse treatment remains of vital importance to preserve vision in the contralateral eye.



Similar content being viewed by others
Abbreviations
- AAION:
-
Arteritic anterior ischemic optic neuropathy
- ACR:
-
American College of Rheumatology
- AION:
-
Anterior ischemic optic neuropathy
- BCVA:
-
Best corrected visual acuity
- BSR:
-
British Society of Rheumatology
- CRAO:
-
Central retinal artery occlusion
- CRP:
-
C-reactive protein
- CVA:
-
Cerebrovascular accident
- ESR:
-
Erythrocyte segmentation rate
- EULAR:
-
European League against Rheumatism
- GCA:
-
Giant cell arteritis
- ION:
-
Ischemic optic neuropathy
- MP:
-
Methylprednisolone
- NAAION:
-
Non-arteritic anterior ischemic optic neuropathy
- NLP:
-
No light perception
- OIS:
-
Ocular ischemic syndrome
- PION:
-
Posterior ischemic optic neuropathy
- TAB:
-
Temporal artery biopsy
- TCZ:
-
Tocilizumab
References
Weyang C, Goronzy J (2003) Mechanisms of disease medium and large vessel vasculitis. N Eng J Med 349:160–169
Weyang C, Goronzy J (2003) Giant-cell arteritis and polymyalgia rheumatica. Ann Intern Med 39:505–515
Soriano A, Muratore F, Pipitone N, Boiardi L, Cimino L, Salvarani C (2017) Visual loss and other cranial ischaemic complications in giant cell arteritis. Nat Rev Rheumatol [Internet] 13(8):476–484
Buttgereit F, Dejaco C, Matteson EL, Dasgupta B (2016) Polymyalgia rheumatica and giant cell arteritis a systematic review. JAMA - J Am Med Assoc 315(22):2442–2458
Salvarani C, Pipitone N, Versari A, Hunder GG (2012) Clinical features of polymyalgia rheumatica and giant cell arteritis. Nat Rev Rheumatol [Internet] 8(9):509–521
Salvarani C, Cantini F, Boiardi L, Hunder G (2002) Polymyalgia rheumatica and giant-cell arteritis. N Engl J Med 347(4):261–271
Liozon E, Dalmay F, Lalloue F, Gondran G, Bezanahary H, Fauchais AL et al (2016) Risk factors for permanent visual loss in biopsy-proven giant cell arteritis: a study of 339 patients. J Rheumatol 43(7):1393–1399
Saleh M, Turesson C, Englund M, Merkel PA, Mohammad AJ (2016) Visual complications in patients with biopsy-proven giant cell arteritis: a population-based study. J Rheumatol 43(8):1559–1565
Hernández-Rodríguez J, Segarra M, Vilardell C, Sánchez M, García-Martínez A, Esteban MJ et al (2003) Elevated production of interleukin-6 is associated with a lower incidence of disease-related ischemic events in patients with giant-cell arteritis: angiogenic activity of interleukin-6 as a potential protective mechanism. Circulation 107(19):2428–2434
Maz M, Chung SA, Abril A, Langford CA, Gorelik M, Guyatt G et al (2021) American College of Rheumatology/Vasculitis Foundation guideline for the management of giant cell arteritis and Takayasu arteritis. Arthritis Care Res 73(8):1071–1087
Hellmich B, Agueda A, Monti S, Buttgereit F, De Boysson H, Brouwer E et al (2020) 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 79(1):19–130
MacKie SL, Dejaco C, Appenzeller S, Camellino D, Duftner C, Gonzalez-Chiappe S et al (2020) British society for rheumatology guideline on diagnosis and treatment of giant cell arteritis. Rheumatol (UK) 59(3):E1–E23
Vodopivec I, Rizzo JF (2018) Ophthalmic manifestations of giant cell arteritis. Rheumatol (UK) 57(Suppl_2):ii63–ii72
Biousse V, Newman NJ (2015) Ischemic optic neuropathies. N Engl J Med [Internet] 372(25):2428–2436
Mendrinos E, Machinis TG, Pournaras CJ (2010) Ocular ischemic syndrome. Surv Ophthalmol [Internet] 55(1):2–34
Hayreh SS, Podhansky P, Zimmerman B (1998) Ocular manifestations of giant cell arteritis. Am J Opthalmology 125(4):509–520
Cornblath WT, Eggenberger ER (1997) Progressive visual loss from giant cell arteritis despite high-dose intravenous methylprednisolone. Ophthalmology [Internet] 104(5):854–858
Hwang JM, Girkin CA, Perry JD, Lai JC, Miller NR, Hellmann DB (1999) Bilateral ocular ischemic syndrome secondary to giant cell arteritis progressing despite corticosteroid treatment. Am J Ophthalmol 127(1):102–104
Chan CCK, Paine M, O’Day J (2001) Steroid management in giant cell arteritis. Br J Ophthalmol 85(9):1061–1064
Wenkel H (2001) Bilaterale amaurose bei 11 patienten mit histologisch gesicherter riesenzellarteriitis. Klin Monbl Augenheilkd 218(10):658–661
Hayreh SS, Zimmerman B (2003) Visual deterioration in giant cell arteritis patients while on high doses of corticosteroid therapy. Ophthalmology 110(6):1204–1215
Danesh-Meyer H, Savino PJ, Gamble GG (2005) Poor prognosis of visual outcome after visual loss from giant cell arteritis. Ophthalmology 112(6):1098–1103
Loddenkemper T, Sharma P, Katzan I, Plant GT (2007) Risk factors for early visual deterioration in temporal arteritis. J Neurol Neurosurg Psychiatry 78(11):1255–1259
Sheldon CA, White VA, Holland SP (2011) Giant cell arteritis presenting with bilateral loss of vision and jaw pain: reminder of a potentially devastating condition. Journal Can Dental Assoc 77:b55
Wagner S, Jain S (2016) Sequential vision loss in a patient with headache. BMJ 353:8–10
Dumont A, Lecannuet A, Boutemy J, Maigné G, Martin-Silva N, Deshayes S et al (2020) Characteristics and outcomes of patients with ophthalmologic involvement in giant-cell arteritis: a case-control study. Semin Arthritis Rheum 50(2):335–341
Vionnet J, Buss G, Mayer C, Sokolov AA, Borruat FX, Spertini F (2017) Tocilizumab for giant cell arteritis with corticosteroid-resistant progressive anterior ischemic optic neuropathy. Jt Bone Spine 84(5):615–619
Le Goueff A, Peters J, Willcocks L, Jayne D (2019) Visual loss in giant cell arteritis 3 weeks after steroid initiation. BMJ Case Rep 12(3):12–15
Stone JH, Tuckwell K, Dimonaco S, Klearman M, Aringer M, Blockmans D et al (2017) Trial of tocilizumab in giant-cell arteritis. N Engl J Med 377(4):317–328
Stone JH, Han J, Aringer M, Blockmans D, Brouwer E, Cid MC et al (2021) Long-term effect of tocilizumab in patients with giant cell arteritis: open-label extension phase of the giant cell arteritis actemra (GiACTA) trial. Lancet Rheumatol 3(5):e328–e336
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
IK: performed the systematic search and drafted the manuscript. SA: performed the systematic search and assisted in manuscript drafting. OM: assessed the patient and assisted in manuscript drafting. DD: conceived the idea of the review, assisted in manuscript drafting and supervised the project.
Corresponding author
Ethics declarations
Conflict of interest
All the co-authors take full responsibility for the accuracy and integrity of all aspects of the work. The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kokloni, I.N., Aligianni, S.I., Makri, O. et al. Vision loss in giant cell arteritis: case-based review. Rheumatol Int 42, 1855–1862 (2022). https://doi.org/10.1007/s00296-022-05160-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05160-x