Abstract
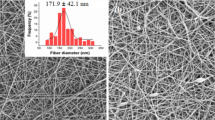
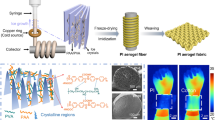
Localized application of drugs at specific wound area has many advantages and less side effects as compared with other drug administrative routes. Burn patients suffer from swear pain, and the major focus of medical practitioners includes pain and infection management. Advancements in material science, especially nanofibers, have gained a lot of attention in various applications such as filtration, nanocomposites, protection and medical sciences. Nanofibers (NFs) loaded with drug, applied on local wound area, can reduce the side effects as well as can provide quick action. This study dealt with the fabrication of drug-loaded NFs for better pain management with controlled drug release. Two layers of NFs were fabricated with different drugs using electrospinning. Contact layer of polyethylene oxide nanofibers was loaded with gabapentin (a nerve pain killer) for quick action followed by second layer of sodium alginate nanofibers with acetaminophen (mild pain killer) for synergizing the effect. The fabricated dressing was characterized using scanning electron microscope, Fourier transform infrared spectroscopy, thermogravimetric analysis, UV–Vis spectroscopy, drug release rate and liquid absorption tests. Different drug release kinetic models were applied to the experimental data, and drug release from the first layer was best followed by first-order kinetic model, while, the second layer was best described by Hixson–Crowell kinetic model. The combination of quick release of strong nerve pain killer followed by slow release of mild pain killer could be a good tool to reduce pain scores in a more professional manner with less side effects in burn patients.












Similar content being viewed by others
Change history
11 January 2021
The original version of this article inadvertently contained mistake.
References
Bhattacharya S (2012) Principles and practice of wound care. In: Indian Journal of Plastic Surgery. Jaypee Brothers Medical Publishers (P) Ltd., pp 167–169
Becker WK, Cioffi WG, McManus AT et al (1991) Fungal burn wound infection. A 10-year experience. Arch Surg 126:44–48
Sarabahi S, Tiwari VK, Arora S et al (2012) Changing pattern of fungal infection in burn patients. Burns 38:520–528. https://doi.org/10.1016/j.burns.2011.09.013
Weber J, McManus A, Nursing Committee of the International Society for Burn Injuries (2004) Infection control in burn patients. Burns 30:A16–A24. https://doi.org/10.1016/j.burns.2004.08.003
Singh R, Chacharkar MP (2011) Dried gamma-irradiated amniotic membrane as dressing in burn wound care. J Tissue Viability 20:49–54. https://doi.org/10.1016/J.JTV.2010.06.001
Thomas J, Slone W, Linton S et al (2011) In vitro antimicrobial efficacy of a silver alginate dressing on burn wound isolates. J Wound Care 20:124–128. https://doi.org/10.12968/jowc.2011.20.3.124
Mir M, Ali MN, Barakullah A et al (2018) Synthetic polymeric biomaterials for wound healing: a review. Prog Biomater 7:1–21. https://doi.org/10.1007/s40204-018-0083-4
Tredget EE, Shankowsky HA, Groeneveld A, Burrell R (1998) A matched-pair, randomized study evaluating the efficacy and safety of acticoat silver-coated dressing for the treatment of burn wounds. J Burn Care Rehabil 19:531–537. https://doi.org/10.1097/00004630-199811000-00013
Leaper DJ (2006) Silver dressings: their role in wound management. Int Wound J 3:282–294. https://doi.org/10.1111/j.1742-481X.2006.00265.x
Munteanu A, Florescu IP, Nitescu C (2016) A modern method of treatment: the role of silver dressings in promoting healing and preventing pathological scarring in patients with burn wounds. J Med Life 9:306–315
de Castro RJA, Leal PC, Sakata RK (2013) Tratamento da dor em queimados. Rev Bras Anestesiol 63:154–158. https://doi.org/10.1590/S0034-70942013000100013
Gray P, Williams B, Cramond T (2008) Successful use of gabapentin in acute pain management following burn injury: a case series. Pain Med 9:371–376. https://doi.org/10.1111/j.1526-4637.2006.00149.x
Lui TH, Lam CS (2012) Gabapentin for pain control in burn patients for surgical debridement: pharmacokinetic properties consideration. Arch Trauma Res 1:137–138. https://doi.org/10.5812/atr.7068
Sheppard N (2014) Gabapentin in burns. Arch Trauma Res 3:e6471. https://doi.org/10.5812/ATR.6471
Jirsák O, Dao TA (2009) Production, Properties and End-Uses of Nanofibres. Nanotechnology in Construction 3. Springer, Berlin, Heidelberg, pp 95–99
Rafiq M, Hussain T, Abid S et al (2018) Development of sodium alginate/PVA antibacterial nanofibers by the incorporation of essential oils. Mater Res Express 5:035007. https://doi.org/10.1088/2053-1591/aab0b4
Sridhar R, Venugopal JR, Sundarrajan S et al (2011) Electrospun nanofibers for pharmaceutical and medical applications. J Drug Deliv Sci Technol 21:451–468. https://doi.org/10.1016/S1773-2247(11)50075-9
Shan X, Liu C, Li F et al (2015) Nanoparticles vs. nanofibers: a comparison of two drug delivery systems on assessing drug release performance in vitro. Des Monomers Polym 18:678–689. https://doi.org/10.1080/15685551.2015.1070500
Nataraj SK, Yang KS, Aminabhavi TM (2012) Polyacrylonitrile-based nanofibers—a state-of-the-art review. Prog Polym Sci 37:487–513. https://doi.org/10.1016/j.progpolymsci.2011.07.001
Haider A, Haider S, Kang I-K (2018) A comprehensive review summarizing the effect of electrospinning parameters and potential applications of nanofibers in biomedical and biotechnology. Arab J Chem 11:1165–1188. https://doi.org/10.1016/J.ARABJC.2015.11.015
Beachley V, Wen X (2009) Effect of electrospinning parameters on the nanofiber diameter and length. Mater Sci Eng C Mater Biol Appl 29:663–668. https://doi.org/10.1016/j.msec.2008.10.037
Ma L, Deng L, Chen J (2014) Applications of poly(ethylene oxide) in controlled release tablet systems: a review. Drug Dev Ind Pharm 40:845–851. https://doi.org/10.3109/03639045.2013.831438
Upadhye SB, Rajabi-Siahboomi AR (2013) Properties and applications of polyethylene oxide and ethylcellulose for tamper resistance and controlled drug delivery. Springer, New York, pp 145–158
Peinado I, Mason M, Romano A et al (2016) Stability of β-carotene in polyethylene oxide electrospun nanofibers. Appl Surf Sci 370:111–116. https://doi.org/10.1016/J.APSUSC.2016.02.150
Agyemang FO, Li F, Momade FWY, Kim H (2016) Effect of poly(ethylene oxide) and water on electrospun poly(vinylidene fluoride) nanofibers with enhanced mechanical properties as pre-filter for oil-in-water filtration. Mater Chem Phys 182:208–218. https://doi.org/10.1016/J.MATCHEMPHYS.2016.07.025
Pinto NJ, Johnson AT, MacDiarmid AG et al (2003) Electrospun polyaniline/polyethylene oxide nanofiber field-effect transistor. Appl Phys Lett 83:4244–4246. https://doi.org/10.1063/1.1627484
Esmaeili A, Haseli M (2017) Electrospinning of thermoplastic carboxymethyl cellulose/poly(ethylene oxide) nanofibers for use in drug-release systems. Mater Sci Eng C 77:1117–1127. https://doi.org/10.1016/j.msec.2017.03.252
Cho E, Kim J, Park CW et al (2018) Chemically bound Prussian blue in sodium alginate hydrogel for enhanced removal of Cs ions. J Hazard Mater 360:243–249. https://doi.org/10.1016/J.JHAZMAT.2018.08.031
Shen W, Hsieh Y-L (2014) Biocompatible sodium alginate fibers by aqueous processing and physical crosslinking. Carbohydr Polym 102:893–900. https://doi.org/10.1016/j.carbpol.2013.10.066
Miraftab M, Masood R (2011) Antimicrobial properties of alginate-chitosan (alchite) fibers developed for wound care applications development of polysaccharide based wound dressings. Artic J Ind Text, View project. https://doi.org/10.1177/1528083710376985
de Etchepare M A, Barin JS, Cichoski AJ et al (2015) Microencapsulation of probiotics using sodium alginate. Ciência Rural 45:1319–1326. https://doi.org/10.1590/0103-8478cr20140938
Nasajpour A, Ansari S, Rinoldi C et al (2018) A multifunctional polymeric periodontal membrane with osteogenic and antibacterial characteristics. Adv Funct Mater 28:1703437. https://doi.org/10.1002/adfm.201703437
Lee KY, Mooney DJ (2012) Alginate: properties and biomedical applications. Prog Polym Sci 37:106–126. https://doi.org/10.1016/j.progpolymsci.2011.06.003
Szekalska M, Puciłowska A, Szymańska E et al (2016) Alginate: current use and future perspectives in pharmaceutical and biomedical applications. Int J Polym Sci 2016:1–17. https://doi.org/10.1155/2016/7697031
Saquing CD, Tang C, Monian B et al (2013) Alginate-polyethylene oxide blend nanofibers and the role of the carrier polymer in electrospinning. Ind Eng Chem Res 52:8692–8704. https://doi.org/10.1021/ie302385b
Hu C, Gong RH, Zhou FL (2015) Electrospun sodium alginate/polyethylene oxide fibers and nanocoated yarns. Int J Polym Sci 2015:1–12. https://doi.org/10.1155/2015/126041
Nasajpour A, Mandla S, Shree S et al (2017) Nanostructured fibrous membranes with rose spike-like architecture. Nano Lett 17:6235–6240. https://doi.org/10.1021/acs.nanolett.7b02929
Abid S, Hussain T, Raza ZA, Nazir A (2018) Current applications of electrospun polymeric nanofibers in cancer therapy. Mater Sci Eng C. https://doi.org/10.1016/J.MSEC.2018.12.105
Dantas MDM, Cavalcante DRR, Araújo FEN et al (2011) Improvement of dermal burn healing by combining sodium alginate/chitosan-based films and low level laser therapy. J Photochem Photobiol B Biol 105:51–59. https://doi.org/10.1016/j.jphotobiol.2011.06.009
Abid S, Raza ZA, Rehman A (2016) Synthesis of poly(3-hydroxybutyrate) nanospheres and deposition thereof into porous thin film. Mater Res Express. https://doi.org/10.1088/2053-1591/3/10/105042
Safi S, Morshed M, Hosseini Ravandi SA, Ghiaci M (2007) Study of electrospinning of sodium alginate, blended solutions of sodium alginate/poly(vinyl alcohol) and sodium alginate/poly(ethylene oxide). J Appl Polym Sci 104:3245–3255. https://doi.org/10.1002/app.25696
Dhawan S, Dhawan K, Varma M, Sinha VR (2005) Applications of poly (ethylene oxide) in drug delivery systems. Pharm Technol 29:82–96
Jensen BEB, Dávila I, Zelikin AN (2016) Poly(vinyl alcohol) physical hydrogels: matrix-mediated drug delivery using spontaneously eroding substrate. J Phys Chem B 120:5916–5926. https://doi.org/10.1021/acs.jpcb.6b01381
Tønnesen HH, Karlsen J (2002) Alginate in drug delivery systems. Drug Dev Ind Pharm 28:621–630. https://doi.org/10.1081/DDC-120003853
Thomas S (2000) Alginate dressings in surgery and wound management—part 1. J Wound Care 9:56–60. https://doi.org/10.12968/jowc.2000.9.2.26338
Abid S, Hussain T, Nazir A et al (2018) Acetaminophen loaded nanofibers as a potential contact layer for pain management in burn wounds. Mater Res Express 5:085017. https://doi.org/10.1088/2053-1591/aad2eb
Abid S, Hussain T, Nazir A et al (2018) Development of nanofibers based neuropathic patch loaded with Lidocaine to deal with nerve pain in burn patients. IOP Conf Ser Mater Sci Eng 414:012019. https://doi.org/10.1088/1757-899X/414/1/012019
Mendham JE (2004) Gabapentin for the treatment of itching produced by burns and wound healing in children: a pilot study. Burns 30:851–853. https://doi.org/10.1016/J.BURNS.2004.05.009
Malenfant A, Forget R, Papillon J et al (1996) Prevalence and characteristics of chronic sensory problems in burn patients. Pain 67:493–500
Mbah CJ, Nnadi CO (2014) Transdermal delivery of gabapentin: effect of cosolvent and microemulsion on permeation through the rat skin. Pharmacol Pharm 05:471–478. https://doi.org/10.4236/pp.2014.55057
Dhasmana S, Singh V, Pal US (2009) The combined analgesic effect of gabapentin and transdermal fentanyl patch on acute and chronic pain after maxillary cancer surgeries. J Maxillofac Oral Surg 8:55–59. https://doi.org/10.1007/s12663-009-0014-y
Predescu O, Fish J, Smith T, Ward L (2007) Role of gabapentin in burned patients. Burns 33:S133. https://doi.org/10.1016/j.burns.2006.10.309
Sintov AC, Krymberk I, Gavrilov V, Gorodischer R (2003) Transdermal delivery of paracetamol for paediatric use: effects of vehicle formulations on the percutaneous penetration. J Pharm Pharmacol 55:911–919. https://doi.org/10.1211/0022357021486
Ravula R, Herwadkar AK, Abla MJ et al (2016) Formulation optimization of a drug in adhesive transdermal analgesic patch. Drug Dev Ind Pharm 42:862–870. https://doi.org/10.3109/03639045.2015.1071832
Conaghan PG, O’Brien CM, Wilson M, Schofield JP (2011) Transdermal buprenorphine plus oral paracetamol vs an oral codeine-paracetamol combination for osteoarthritis of hip and/or knee: a randomised trial. Osteoarthr Cartil 19:930–938. https://doi.org/10.1016/j.joca.2011.03.011
Bonino CA, Krebs MD, Saquing CD et al (2011) Electrospinning alginate-based nanofibers: From blends to crosslinked low molecular weight alginate-only systems. Carbohydr Polym 85:111–119. https://doi.org/10.1016/j.carbpol.2011.02.002
Park SA, Park KE, Kim WD (2010) Preparation of sodium alginate/poly(ethylene oxide) blend nanofibers with lecithin. Macromol Res 18:891–896. https://doi.org/10.1007/s13233-010-0909-y
Kataria K, Gupta A, Rath G et al (2014) In vivo wound healing performance of drug loaded electrospun composite nanofibers transdermal patch. Int J Pharm 469:102–110. https://doi.org/10.1016/j.ijpharm.2014.04.047
Barzegar-Jalali M, Adibkia K, Valizadeh H et al (2008) Kinetic analysis of drug release from nanoparticles. J Pharm Pharm Sci 11:167–177
Shoaib MH, Tazeen J, Merchant HA (2006) Original article evaluation of drug release kinetics from ibuprofen matrix tablets using HPMC. Pak J Pharm Sci 19:119–124
Siepmann J, Peppas NA (2011) Higuchi equation: derivation, applications, use and misuse. Int J Pharm 418:6–12. https://doi.org/10.1016/j.ijpharm.2011.03.051
Ka R (2014) Mathematical models of drug dissolution: a review. Sch Acad J Pharm 3:388–396
Zahir A, Aslam Z, Kamal MS et al (2017) Development of novel cross-linked chitosan for the removal of anionic Congo red dye. J Mol Liq 244:211–218. https://doi.org/10.1016/J.MOLLIQ.2017.09.006
Wang T, Gu Q, Zhao J et al (2015) Calcium alginate enhances wound healing by up-regulating the ratio of collagen types I/III in diabetic rats. Int J Clin Exp Pathol 8:6636–6645
Boateng JS, Matthews KH, Stevens HNE, Eccleston GM (2008) Wound healing dressings and drug delivery systems: a review. J Pharm Sci 97:2892–2923. https://doi.org/10.1002/jps.21210
Lansdown ABG (2002) Calcium: a potential central regulator in wound healing in the skin. Wound Repair Regen 10:271–285. https://doi.org/10.1046/j.1524-475X.2002.10502.x
Pucić I, Jurkin T (2012) FTIR assessment of poly(ethylene oxide) irradiated in solid state, melt and aqueous solution. Radiat Phys Chem 81:1426–1429. https://doi.org/10.1016/j.radphyschem.2011.12.005
Baishya H (2017) Application of mathematical models in drug release kinetics of carbidopa and levodopa ER tablets. J Dev Drugs 06:1–8. https://doi.org/10.4172/2329-6631.1000171
Conti S, Gaisford S, Buckton G, Conte U (2006) Solution calorimetry to monitor swelling and dissolution of polymers and polymer blends. Thermochim Acta 450:56–60. https://doi.org/10.1016/J.TCA.2006.07.017
Maver T, Kurečič M, Smrke DM et al (2016) Electrospun nanofibrous CMC/PEO as a part of an effective pain-relieving wound dressing. J Sol-Gel Sci Technol 79:475–486. https://doi.org/10.1007/s10971-015-3888-9
Siepmann J (2012) Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC). Adv Drug Deliv Rev 64:163–174. https://doi.org/10.1016/J.ADDR.2012.09.028
Caccavo D, Cascone S, Lamberti G, Barba AA (2015) Modeling the drug release from hydrogel-based matrices. Mol Pharm 12:474–483. https://doi.org/10.1021/mp500563n
Kajjari PB, Manjeshwar LS, Aminabhavi TM (2011) Novel interpenetrating polymer network hydrogel microspheres of chitosan and poly(acrylamide)- grafted -guar gum for controlled release of ciprofloxacin. Ind Eng Chem Res 50:13280–13287. https://doi.org/10.1021/ie2012856
Holte Ø, Onsøyen E, Myrvold R, Karlsen J (2003) Sustained release of water-soluble drug from directly compressed alginate tablets. Eur J Pharm Sci 20:403–407. https://doi.org/10.1016/J.EJPS.2003.09.003
Streubel A, Siepmann J, Dashevsky A, Bodmeier R (2000) pH-independent release of a weakly basic drug from water-insoluble and -soluble matrix tablets. J Control Release 67:101–110. https://doi.org/10.1016/S0168-3659(00)00200-5
Dïnç CO, Kïbarer G, Güner A (2010) Solubility profiles of poly(ethylene glycol)/solvent systems. II. Comparison of thermodynamic parameters from viscosity measurements. J Appl Polym Sci 117:1100–1119. https://doi.org/10.1002/app.31829
Fu Y, Kao WJ (2010) Drug release kinetics and transport mechanisms of non-degradable and degradable polymeric delivery systems. Expert Opin Drug Deliv 7:429–444. https://doi.org/10.1517/17425241003602259
Rehage G, Ernst O, Fuhrmann J (1970) Fickian and non-Fickian diffusion in high polymer systems. Discuss Faraday Soc 49:208. https://doi.org/10.1039/df9704900208
Karimi M (2017) Diffusion in polymer solids and solutions. In: Markos J (ed) Mass transfer in chemical engineering processes. Scitus Academics, New York, p 260
JacquesH CHM, Hopfenberg B, Stannett V (1974) Super case II transport of organic vapors in glassy polymers. Permeability of plastic films and coatings. Polymer science and technology. Springer, Bostan, pp 73–86
Dash S, Murthy PN, Nath L, Chowdhury P (2010) Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm 67:217–223. https://doi.org/10.1016/S0928-0987(01)00095-1
Sullad AG, Manjeshwar LS, Aminabhavi TM (2009) Controlled release of theophylline from interpenetrating blend microspheres of poly(vinyl alcohol) and methyl cellulose. J Appl Polym Sci. https://doi.org/10.1002/app.29625
Kajjari PB, Manjeshwar LS, Aminabhavi TM (2011) Semi-interpenetrating polymer network hydrogel blend microspheres of gelatin and hydroxyethyl cellulose for controlled release of theophylline. Ind Eng Chem Res 50:7833–7840. https://doi.org/10.1021/ie200516k
Sullad AG, Manjeshwar LS, Aminabhavi TM (2010) Novel pH-sensitive hydrogels prepared from the blends of poly(vinyl alcohol) with acrylic acid- graft -guar gum matrixes for isoniazid delivery. Ind Eng Chem Res 49:7323–7329. https://doi.org/10.1021/ie100389v
Gaabour LH (2015) Thermal spectroscopy and kinetic studies of PEO/PVDF loaded by carbon nanotubes. J Mater 2015:1–8. https://doi.org/10.1155/2015/824859
Theodosopoulos G, Zisis C, Charalambidis G et al (2017) Synthesis, characterization and thermal properties of poly(ethylene oxide), PEO, polymacromonomers via anionic and ring opening metathesis polymerization. Polymers (Basel) 9:145. https://doi.org/10.3390/polym9040145
Kragović M, Daković A, Marković M (2016) Kinetic of thermal degradation of alginate-zeolite composites. Zast Mater 57:559–564. https://doi.org/10.5937/ZasMat1604559K
Yulong Z, Huang Z, Zhang J, et al (2010) Thermal degradation of sodium alginate-incorporated soy protein isolate/glycerol composite membranes. In: 17th IAPRI world conference on packaging, pp 402–405
Ahmadinegad M, Lashkarizadeh MR, Ghahreman M et al (2014) Efficacy of dressing with absorbent foam versus dressing with gauze in prevention of tracheostomy site infection. Tanaffos 13:13–19
Bredow J, Hoffmann K, Oppermann J et al (2018) Evaluation of absorbent versus conventional wound dressing. Dtsch Arztebl Int 115:213–219. https://doi.org/10.3238/arztebl.2018.0213
Li T-T, Lou C-W, Chen A-P et al (2016) Highly absorbent antibacterial hemostatic dressing for healing severe hemorrhagic wounds. Materials (Basel) 9:793. https://doi.org/10.3390/ma9090793
Sullad AG, Manjeshwar LS, Aminabhavi TM (2010) Polymeric blend microspheres for controlled release of theophylline. J Appl Polym Sci. https://doi.org/10.1002/app.31866
Acknowledgements
Authors acknowledge National Textile Research Center, National Textile University, Faisalabad (NTU), Pakistan, for testing, characterization and the supervisory panel for kind support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest with anyone.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abid, S., Hussain, T., Nazir, A. et al. A novel double-layered polymeric nanofiber-based dressing with controlled drug delivery for pain management in burn wounds. Polym. Bull. 76, 6387–6411 (2019). https://doi.org/10.1007/s00289-019-02727-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-019-02727-w