Abstract
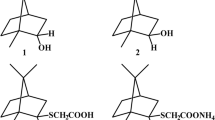
Pathogenic fungi, as an increasing global threat to human health, represent a sizable risk. However, significant attention should also be paid to the yeast biofilms. One promising strategy for combating resistant microbes, as well as fungal biofilms, is to extend the lifespan and efficacy of our currently employed drugs by using combination therapy. Since the application of combined therapy of fungal infections is currently accepted, we have decided to verify the efficacy of derivative H in combination with fluconazole on C. albicans biofilm. The main advantage of synergy over monotherapy lies in reducing or even completely preventing the induction of resistance of fungal cells. We have decided to verify the derivative H (1,4-dihydropyridine-2,3,5-tricarboxylate), an intermediate of nilvadipine synthesis, in the resistance of C. albicans to fluconazole. Therefore, we have focused on the influence of derivative H on the gene expression of the main C. albicans adhesin (ALS3), which is important for the tissue colonization during the infection process. Our results show that the newly synthesized derivative H had an impact on biofilm eradication. The effect of biofilm diminution could, therefore, be explained as derivative H preventing the adherence of C. albicans cells. This study supports even more the attractiveness of this substance as a potential agent that could be used in synergy with commonly used azoles to treat various fungal infections.

Similar content being viewed by others
References
Shapiro RS, Robbins N, Cowen LE (2011) Regulatory circuitry governing fungal development, drug resistance, and disease. Microbiol Mol Biol Rev 75(2):213–267. https://doi.org/10.1128/MMBR.00045-10
Brown ED, Wright GD (2016) Antibacterial drug discovery in the resistance era. Nature 529(7586):336–343. https://doi.org/10.1038/nature17042
Zimmermann GR, Lehár J, Keith CT (2007) Multi-target therapeutics: when the whole is greater than the sum of the parts. Drug Discov Today 12(1–2):34–42
Hill JA, Cowen LE (2015) Using combination therapy to thwart drug resistance. Future Microbiol 10(11):1719–1726. https://doi.org/10.2217/fmb.15.68
Chudík L, Marchalín Š, Daïch A, Decroix B (2000) New synthesis of the calcium antagonist Nilvadipine. Res Adv Synth Org Chem 1:1–7
Ježíková Z, Pagáč T, Pfeiferová B, Bujdáková H, Dižová S, Jančíková I, Gášková D, Olejníková P (2017) Synergy between azoles and 1,4-dihydropyridine derivative as an option to control fungal infections. Antonie Van Leeuwenhoek 110(9):1219–1226. https://doi.org/10.1007/s10482-017-0895-6
EUCAST (2017) European committee on antimicrobial susceptibility testing. http://www.eucast.org. Accessed Aug 2018
Sherry L, Rajendran R, Lappin DF, Borghi E, Perdoni F, Falleni M, Tosi D, Smith K, Williams C, Jones B et al (2014) Biofilms formed by Candida albicans bloodstream isolates display phenotypic and transcriptional heterogeneity that are associated with resistance and pathogenicity. BMC Microbiol 14:182. https://doi.org/10.1186/1471-2180-14-182
Gullapalli S, Ramarao P (2002) L-type Ca2 + channel modulation by dihydropyridines potentiates kappa-opioid receptor agonist induced acute analgesia and inhibits development of tolerance in rats. Neuropharmacology 42(4):467–475. https://doi.org/10.1016/S0028-3908(01)00200-3
Whaley SG, Berkow EL, Rybak JM, Nishimoto AT, Barker KS, Rogers PD (2016) Azole antifungal resistance in Candida albicans and emerging non-albicans Candida species. Front Microbiol 7:2173. https://doi.org/10.3389/fmicb.2016.02173
Hoyer LL (2001) The ALS gene family of Candida albicans. Trends Microbiol 9(4):176–180
Zhao X, Daniels KJ, Oh SH, Green CB, Yeater KM, Soll DR, Hoyer LL (2006) Candida albicans Als3p is required for wild-type biofilm formation on silicone elastomer surfaces. Microbiology 152(8):2287–2299
Nobile CJ, Mitchell AP (2006) Genetics and genomics of Candida albicans biofilm formation. Cell Microbiol 8(9):1382–1391
Nett JE, Lepak AJ, Marchillo K, Andes DR (2009) Time course global gene expression analysis of an in vivo Candida biofilm. J Infect Dis 200(2):307–313. https://doi.org/10.1086/599838
Fanning S, Mitchell AP (2012) Fungal Biofilms. PLoS Pathog 8(4):e1002585. https://doi.org/10.1371/journal.ppat.1002585
Acknowledgements
This work was supported by the Project APVV-0719-12 and VEGA Project 1/0697/18.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ježíková, Z., Pagáč, T., Víglaš, J. et al. Synergy Over Monotherapy. Curr Microbiol 76, 673–677 (2019). https://doi.org/10.1007/s00284-019-01678-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-019-01678-9