Abstract
Purpose
Acneiform rash is frequently observed in patients undergoing cancer treatment with anti-epidermal growth factor receptor (EGFR) antibody drugs and can often necessitate treatment discontinuation. However, the specific changes in skin parameters resulting from anti-EGFR antibody drug administration are poorly understood. Therefore, this study aimed to longitudinally and quantitatively evaluate the changes in skin parameters (transepidermal water loss [TEWL], hydration level, and sebum level) caused by anti-EGFR antibody drugs and investigate their potential as control markers for skin disorders.
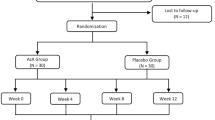
Methods
This prospective study included 12 patients with colorectal cancer who received anti-EGFR antibody drugs for the first time. The assessment items included the grade of acneiform rash and skin parameters (TEWL, hydration level, and sebum level), which were observed for up to 6 weeks after administration of the medication.
Results
The enrolled patients were classified into two groups based on the grade of acneiform rash caused by anti-EGFR antibody drugs: “Grade 1 and lower,” and “Grade 2 and higher.” The skin parameters were compared between these groups. The results showed that in the “Grade 2 and higher” group, TEWL in the face (at week 2 of administration), chest (baseline, weeks 2 and 6 of administration), and back (at week 2 of administration) were significantly higher than those in the “Grade 1 and lower” group. However, the two groups showed no significant differences in hydration or sebum levels at any time point.
Conclusion
TEWL can serve as a marker for acneiform rashes induced by anti-EGFR antibody drugs during cancer treatment.






Similar content being viewed by others
Data Availability Statement
Additional data are available from the authors upon reasonable request.
References
Saltz LB, Clarke S, Díaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, Couture F, Sirzén F, Cassidy J (2008) Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 26:2013–2019. https://doi.org/10.1200/JCO.2007.14.9930
Fuchs CS, Marshall J, Mitchell E, Wierzbicki R, Ganju V, Jeffery M, Schulz J, Richards D, Soufi-Mahjoubi R, Wang B, Barrueco J (2007) Randomized, controlled trial of irinotecan plus infusional, bolus, or oral fluoropyrimidines in first-line treatment of metastatic colorectal cancer: results from the BICC-C Study. J Clin Oncol 25:4779–4786. https://doi.org/10.1200/JCO.2007.11.3357
Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem J, Rivera F, Kocákova I, Ruff P, Błasińska-Morawiec M, Šmakal M, Canon JL, Rother M, Oliner KS, Wolf M, Gansert J (2010) Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol 28:4697–4705. https://doi.org/10.1200/JCO.2009.27.4860
Peeters M, Price TJ, Cervantes A, Sobrero AF, Ducreux M, Hotko Y, André T, Chan E, Lordick F, Punt CJ, Strickland AH, Wilson G, Ciuleanu TE, Roman L, Van Cutsem E, Tzekova V, Collins S, Oliner KS, Rong A, Gansert J (2010) Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol 28:4706–4713. https://doi.org/10.1200/JCO.2009.27.6055
Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM, Tattersall MH (1983) On the receiving end–patient perception of the side-effects of cancer chemotherapy. Eur J Cancer Clin Oncol 19:203–208. https://doi.org/10.1016/0277-5379(83)90418-2
de Boer-Dennert M, de Wit R, Schmitz PI, Djontono J, v Beurden V, Stoter G, Verweij J, (1997) Patient perceptions of the side-effects of chemotherapy: the influence of 5HT3 antagonists. Br J Cancer 76:1055–1061. https://doi.org/10.1038/bjc.1997.507
Carelle N, Piotto E, Bellanger A, Germanaud J, Thuillier A, Khayat D (2002) Changing patient perceptions of the side effects of cancer chemotherapy. Cancer 95:155–163. https://doi.org/10.1002/cncr.10630
Nozawa K, Shimizu C, Kakimoto M, Mizota Y, Yamamoto S, Takahashi Y, Ito A, Izumi H, Fujiwara Y (2013) Quantitative assessment of appearance changes and related distress in cancer patients. Psychooncology 22:2140–2147. https://doi.org/10.1002/pon.3268
Tahara M, Shirao K, Boku N, Yamaguchi K, Komatsu Y, Inaba Y, Arai T, Mizunuma N, Satoh T, Takiuchi H, Nishina T, Sakata Y (2008) Multicenter Phase II study of cetuximab plus irinotecan in metastatic colorectal carcinoma refractory to irinotecan, oxaliplatin and fluoropyrimidines. Jpn J Clin Oncol 38:762–769. https://doi.org/10.1093/jjco/hyn102
Muro K, Yoshino T, Doi T, Shirao K, Takiuchi H, Hamamoto Y, Watanabe H, Yang BB, Asahi D (2009) A Phase 2 clinical trial of panitumumab monotherapy in Japanese patients with metastatic colorectal cancer. Jpn J Clin Oncol 39:321–326. https://doi.org/10.1093/jjco/hyp016
Lacouture ME, Mitchell EP, Piperdi B, Pillai MV, Shearer H, Iannotti N, Xu F, Yassine M (2010) Skin toxicity evaluation protocol with panitumumab (STEPP), a phase II, open-label, randomized trial evaluating the impact of a pre-emptive Skin treatment regimen on skin toxicities and quality of life in patients with metastatic colorectal cancer. J Clin Oncol 28:1351–1357. https://doi.org/10.1200/JCO.2008.21.7828
Jonker DJ, O’Callaghan CJ, Karapetis CS, Zalcberg JR, Tu D, Au HJ, Berry SR, Krahn M, Price T, Simes RJ, Tebbutt NC, van Hazel G, Wierzbicki R, Langer C, Moore MJ (2007) Cetuximab for the treatment of colorectal cancer. N Engl J Med 357:2040–2048. https://doi.org/10.1056/NEJMoa071834
Van Cutsem E, Peeters M, Siena S, Humblet Y, Hendlisz A, Neyns B, Canon JL, Van Laethem JL, Maurel J, Richardson G, Wolf M, Amado RG (2007) Open-label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy-refractory metastatic colorectal cancer. J Clin Oncol 25:1658–1664. https://doi.org/10.1200/JCO.2006.08.1620
Stintzing S, Kapaun C, Laubender RP, Jung A, Neumann J, Modest DP, Giessen C, Moosmann N, Wollenberg A, Kirchner T, Heinemann V (2013) Prognostic value of cetuximab-related skin toxicity in metastatic colorectal cancer patients and its correlation with parameters of the epidermal growth factor receptor signal transduction pathway: results from a randomized trial of the German AIO CRC study group. Int J Cancer 132:236–245. https://doi.org/10.1002/ijc.27654
Takahashi H, Asaka J, Tairabune T, Ujiie H, Matsuura Y, Nihei S, Kimura T, Chiba T, Kudo K (2021) Analysis of risk factors for skin disorders caused by anti-epidermal growth factor receptor antibody drugs and examination of methods for their avoidance. J Clin Pharm Ther 46:1404–1411. https://doi.org/10.1111/jcpt.13475
Takahashi H, Yaegashi Y, Saito Y, Nihei S, Tairabune T, Ujiie H, Asaka J, Kudo K (2022) Effect of risk factors for acneiform rash induced by anti-epidermal growth factor receptor antibody drugs on survival: a retrospective observational study. J Pharm Health Care Sci 8:22. https://doi.org/10.1186/s40780-022-00253-y
Kikuchi K, Nozawa K, Yamazaki N, Nakai Y, Higashiyama A, Asano M, Fujiwara Y, Kanda S, Ohe Y, Takashima A, Boku N, Inoue A, Takahashi M, Mori T, Taguchi O, Inoue Y, Mizutani H (2019) Instrumental evaluation sensitively detects subclinical skin changes by the epidermal growth factor receptor inhibitors and risk factors for severe acneiform eruption. J Dermatol 46:18–25. https://doi.org/10.1111/1346-8138.14691
Chandra F, Sandiono D, Sugiri U, Suwarsa O, Gunawan H (2017) Cutaneous side effects and transepidermal water loss to gefitinib: a study of 11 patients. Dermatol Ther (Heidelb) 7:133–141. https://doi.org/10.1007/s13555-016-0163-0
Levin J, Maibach H (2005) The correlation between transepidermal water loss and percutaneous absorption: an overview. J Control Release 103:291–299. https://doi.org/10.1016/j.jconrel.2004.11.035
Löffler H, Aramaki JU, Effendy I (2002) The influence of body mass index on skin susceptibility to sodium lauryl sulphate. Skin Res Technol 8:19–22. https://doi.org/10.1046/j.0909-752x
Nakahara T, Moroi Y, Takayama K, Itoh E, Kido-Nakahara M, Nakanishi Y, Furue M (2015) Changes in sebum levels and the development of acneiform rash in patients with non-small cell lung cancer after treatment with EGFR inhibitors. Onco Targets Ther 8:259–263. https://doi.org/10.2147/OTT.S76860
Acknowledgements
The authors would like to thank the patients for participating in the study and the staff of Iwate Medical University for their assistance.
Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI, Grant-in-Aid for Early-Career Scientists [Grant number: 19K16419, Kojimachi, Chiyoda-ku, Tokyo, Japan].
Author information
Authors and Affiliations
Contributions
HT, TT, HU, JA, and KK conceived and designed the study. HT, YS, KS, and MS were involved in the data acquisition, analysis, and interpretation. All the authors critically revised the manuscript, commented on its drafts, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics Approval
The study was conducted in accordance with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Iwate Medical University School of Medicine (approval number: H29-145).
Consent to participate
All eligible patients were provided with sufficient explanation of the study, and written consent was obtained from them before their participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takahashi, H., Saito, Y., Sugawara, K. et al. Quantitative assessment of skin disorders induced by panitumumab: a prospective observational study. Cancer Chemother Pharmacol 93, 319–328 (2024). https://doi.org/10.1007/s00280-023-04619-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-023-04619-3