Abstract
Purpose
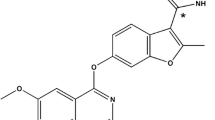
This study evaluated the preclinical pharmacokinetics (PK) and disposition of Fruquintinib (HMPL-013), a small molecule vascular endothelial growth factor receptors inhibitor.
Methods
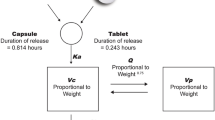
In vitro and in vivo PK/ADME assays were conducted. Allometry and PK modeling/simulation were conducted to predict human PK parameters and the time course profiles.
Results
HMPL-013 has high permeability without efflux. It shows moderate oral bioavailability of 42–53 % and T max < 4 h in mouse, rat, dog and monkey, with exposure-dose linearity proved in rats and dogs. No significant food effect is on dog PK. HMPL-013 has moderately high tissue distribution. It majorly distributes in gastrointestinal tract, liver, kidney, adrenal and adipose. The plasma protein binding fraction is 88–95 % in mouse, rat, dog and human, invariable up to 10 µM. The in vivo clearance of HMPL-013 is low, consistent with the in vitro scaling. Three major oxidative metabolites were identified in liver microsomes of mouse, rat, dog, monkey and human. Dog is mostly similar to human regarding in vitro metabolism. Demethylation, hydroxylation and sequential glucuronidation are the major in vivo metabolic reactions. Direct urinary and biliary excretion of HMPL-013 is negligible. Metabolizing to M1 (demethylation), sequentially glucuronidating, followed by biliary excretion, and to a less extent, by urinary excretion, are important elimination pathways for HMPL-013 in rats. HMPL-013 has low risk of drug–drug interaction. It is predicted to have favorable human PK properties and low efficacious dose.
Conclusion
HMPL-013 demonstrates good preclinical PK and enables successful human PK and dose projection. It is valuable for further clinical development.






Similar content being viewed by others
Abbreviations
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
Vascular endothelial growth factor receptors
- TKI:
-
Tyrosine kinase inhibitors
- PK:
-
Pharmacokinetics
- ADME:
-
Absorption, distribution, metabolism and excretion
- RED:
-
Rapid equilibrium dialysis
- CYP:
-
Cytochrome P450
- API:
-
Active pharmaceutical ingredient
- AUCinf :
-
Area under the concentration–time curve from time zero to infinity
- C max :
-
Maximal concentration
- T max :
-
Time to reach the maximal concentration
- MID:
-
Metabolite identification
- IS:
-
Internal standard
- t 1/2 :
-
Half-lives
- CLR :
-
Renal clearance
- CLB :
-
Biliary clearance
- CL:
-
Plasma total clearance
- V z :
-
Volume of distribution at the terminal phase
- BW:
-
Body weight
- RoE:
-
Rule of exponents
- FIH:
-
First-in-human
- PD:
-
Pharmacodynamic
- CLhep,pred :
-
Predicted hepatic clearance
- CLint :
-
In vitro intrinsic clearance
- BDC:
-
Bile duct cannulated
- MLP:
-
Maximal life span potential
- Tlag:
-
Lag time
- Ka:
-
Absorption rate constant
- DDI:
-
Drug–drug interaction
- f e :
-
Fraction excreted
- f m :
-
Fraction metabolized
- GFR:
-
Glomerular filtration rate
- PBPK:
-
Physiological-based PK
References
Mendel DB, Laird AD, Xin X, Louie SG, Christensen JG, Li G, Schreck RE, Abrams TJ, Ngai TJ, Lee LB (2003) In vivo antitumor activity of SU11248, a novel tyrosine kinase inhibitor targeting vascular endothelial growth factor and platelet-derived growth factor receptors. Clin Cancer Res 9:327–337
Ferrara N (2002) VEGF and the quest for tumour angiogenesis factors. Nat Rev Cancer 2:795–803
Wedge SR, Kendrew J, Hennequin LF, Valentine PJ, Barry ST, Brave SR, Smith NR, James NH, Dukes M, Curwen JO (2005) AZD2171: a highly potent, orally bioavailable, vascular endothelial growth factor receptor-2 tyrosine kinase inhibitor for the treatment of cancer. Cancer Res 65:4389–4400
Morabito A, De Maio E, Di Maio M, Normanno N, Perrone F (2006) Tyrosine kinase inhibitors of vascular endothelial growth factor receptors in clinical trials: current status and future directions. Oncologist 11:753–764
Cook KM, Figg WD (2010) Angiogenesis inhibitors: current strategies and future prospects. CA Cancer J Clin 60:222–243
Chow LQM, Eckhardt SG (2007) Sunitinib: from rational design to clinical efficacy. J Clin Oncol 25:884–896
Iyer R, Fetterly G, Lugade A, Thanavala Y (2010) Sorafenib: a clinical and pharmacologic review. Expert Opin Pharmacother 11:1943–1955
Bhargava P, Robinson MO (2011) Development of second-generation VEGFR tyrosine kinase inhibitors: current status. Curr Oncol Rep 13:103–111
Azmi AS, Wang Z, Philip PA, Mohammad RM, Sarkar FH (2010) Proof of concept: network and systems biology approaches aid in the discovery of potent anticancer drug combinations. Mol Cancer Ther 9:3137–3144
Hellström M, Gerhardt H, Kalén M, Li X, Eriksson U, Wolburg H, Betsholtz C (2001) Lack of pericytes leads to endothelial hyperplasia and abnormal vascular morphogenesis. J Cell Biol 153:543–553
Hu-Lowe DD, Zou HY, Grazzini ML, Hallin ME, Wickman GR, Amundson K, Chen JH, Rewolinski DA, Yamazaki S, Wu EY (2008) Nonclinical antiangiogenesis and antitumor activities of axitinib (AG-013736), an oral, potent, and selective inhibitor of vascular endothelial growth factor receptor tyrosine kinases 1, 2, 3. Clin Cancer Res 14:7272–7283
Patson B, Cohen BR, Olszanski AJ (2012) Pharmacokinetic evaluation of axitinib. Expert Opin Drug Metab Toxicol 8:259–270
Gu Y, Wang GJ, Wu XL, Zheng YT, Zhang JW, Ai H, Sun JG, Jia YW (2010) Intestinal absorption mechanisms of ginsenoside Rh2: stereoselectivity and involvement of ABC transporters. Xenobiotica 40:602–612
Kuhnz W, Gieschen H (1998) Predicting the oral bioavailability of 19-nortestosterone progestins in vivo from their metabolic stability in human liver microsomal preparations in vitro. Drug Metab Dispos 26:1120–1127
Obach RS (1999) Prediction of human clearance of twenty-nine drugs from hepatic microsomal intrinsic clearance data: an examination of in vitro half-life approach and nonspecific binding to microsomes. Drug Metab Dispos 27:1350–1359
Obach RS, Baxter JG, Liston TE, Silber BM, Jones BC, Macintyre F, Rance DJ, Wastall P (1997) The prediction of human pharmacokinetic parameters from preclinical and in vitro metabolism data. J Pharmacol Exp Ther 283:46–58
Center for Drug Evaluation and Research FaDA (2001) Guidance for industry: bioanalytical method validation
Fura A, Vyas V, Humphreys W, Chimalokonda A, Rodrigues D (2008) Prediction of human oral pharmacokinetics using nonclinical data: examples involving four proprietary compounds. Biopharm Drug Dispos 29:455–468
Mahmood I, Balian JD (1996) Interspecies scaling: predicting clearance of drugs in humans. Three different approaches. Xenobiotica 26:887–895
Davies B, Morris T (1993) Physiological parameters in laboratory animals and humans. Pharm Res 10:1093–1095
Wilkinson GR, Shand DG (1975) Commentary: a physiological approach to hepatic drug clearance. Clin Pharmacol Ther 18:377–390
Toutain PL, Bousquet-Melou A (2004) Plasma clearance. J Vet Pharmacol Ther 27:415–425
Rowland M, Tozer T (2011) Clinical pharmacokinetics and pharmacodynamics: concepts and application, 4th edn. Lippincott Williams & Wilkins, a Wolters Kluwer business, New York
Toutain PL, Bousquet-Melou A (2004) Volumes of distribution. J Vet Pharmacol Ther 27:441–453
Berezhkovskiy LM (2008) Prediction of the possibility of the second peak of drug plasma concentration time curve after iv bolus administration from the standpoint of the traditional multi-compartmental linear pharmacokinetics. J Pharm Sci 97:2385–2393
Rolan PE (1994) Plasma-protein binding displacement interactions—why are they still regarded as clinically important. Br J Clin Pharmacol 37:125–128
Benet LZ, Hoener BA (2002) Changes in plasma protein binding have little clinical relevance. Clin Pharmacol Ther 71:115–121
Tillement JP, Urien S, Chaumet-Riffaud P, Riant P, Bree F, Morin D, Albengres E, Barre J (1988) Blood binding and tissue uptake of drugs. recent advances and perspectives. Fundam Clin Pharmacol 2:223–238
Toutain PL, Bousquet-Melou A (2004) Plasma terminal half-life. J Vet Pharmacol Ther 27:427–439
Poulin P, Jones RDO, Jones HM, Gibson CR, Rowland M, Chien JY, Ring BJ, Adkison KK, Ku MS, He H, Vuppugalla R, Marathe P, Fischer V, Dutta S, Sinha VK, Bjornsson T, Lave T, Yates JWT (2011) PHRMA CPCDC initiative on predictive models of human pharmacokinetics, Part 5: prediction of plasma concentration-time profiles in human by using the physiologically-based pharmacokinetic modeling approach. J Pharm Sci 100:4127–4157
Rowland M, Peck C, Tucker G (2011) Physiologically-based pharmacokinetics in drug development and regulatory science. Annu Rev Pharmacol Toxicol 51:45–73
Huang W, Lee SL, Yu LX (2009) Mechanistic approaches to predicting oral drug absorption. AAPS J 11:217–224
Lee KJ, Mower R, Hollenbeck T, Castelo J, Johnson N, Gordon P, Sinko PJ, Holme K, Lee YH (2003) Modulation of nonspecific binding in ultrafiltration protein binding studies. Pharm Res 20:1015–1021
Niggebrugge AE, MacLauchlin C, Dai D, Ford LA, Menendez AT, Chilton AS (2002) A high throughput protein binding assay by cohesive turbulent flow liquid chromatography mass spectrometry to support drug discovery. In: The 50th ASMS conference on mass spectrometry and allied topics, Orlando, Florida
Acknowledgments
The authors are sincerely thankful for the great contributions of Prof. Dafang Zhong and Prof. Xiaoyan Chen from Shanghai Institute of Materia Medica to the rat and dog’s studies, Prof. Zhuohan Hu from Research Institute for Liver Diseases (Shanghai) Co. Ltd. to the human hepatocyte study and Dr. Renke Dai from Zhongshan PharmaSS Corporation to the hPXR study. Appreciations are also given to all the colleagues in Hutchison MediPharma who contributed to the HMPL-013 project.
Conflict of interest
The authors were all employees of Hutchison MediPharma Limited when the study was conducted and are alone responsible for the content and writing of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gu, Y., Wang, J., Li, K. et al. Preclinical pharmacokinetics and disposition of a novel selective VEGFR inhibitor Fruquintinib (HMPL-013) and the prediction of its human pharmacokinetics. Cancer Chemother Pharmacol 74, 95–115 (2014). https://doi.org/10.1007/s00280-014-2471-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2471-3