Abstract
This nationwide, multicenter, open-label, single-arm study evaluated the efficacy and safety of the oral proteasome inhibitor (PI), ixazomib plus lenalidomide (LEN) and dexamethasone (DEX) (IRd) following injectable PI-based therapy for relapsed/refractory multiple myeloma (RRMM). Of 45 patients enrolled, 36 patients received IRd after achieving at least a minor response to 3 cycles of bortezomib or carfilzomib plus LEN + DEX (VRd, n=6; KRd, n=30). At median follow-up of 20.8 months, the 12-month event-free survival rate (primary endpoint) was 49% (90% CI: 35.9−62.0), counting 11 events of progressive disease/death, 8 dropouts and 4 missing response data. The 12-month progression-free survival (PFS) rate by Kaplan-Meier analysis (dropouts as censoring) was 74% (95% CI: 56−86). Median PFS and time to next treatment (95% CI) were 29.0 (21.3−NE) and 32.3 (14.9−35.4) months, respectively; median OS was not evaluable. The overall response rate was 73%, and 42% of patients had a very good partial response or better. Frequent (≥10% incidence) grade ≥3 treatment emergent adverse events were decreased neutrophil and platelet counts (n=7 [16%] each). Two deaths occurred (one during KRd treatment and one during IRd treatment), both due to pneumonia. IRd following injectable PI-based therapy was tolerable and efficacious in RRMM patients.
Trial registration number
NCT03416374; Date of registration: January 31, 2018
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of proteasome inhibitors (PI) has drastically improved the prognosis for transplant-eligible and -ineligible patients with newly diagnosed (NDMM) and relapsed/refractory MM (RRMM) [1,2,3,4]. PI-based therapy has been shown to improve both progression-free survival (PFS) and overall survival (OS) compared with non-PI-based therapy in global phase 3 clinical trials [1,2,3], and several PIs have now been approved and are widely used in routine clinical practice in MM. Recently, there has been a shift in the treatment paradigm towards the use of extended, continuous PI-based therapy, which has delivered superior outcomes compared with shorter, fixed-duration therapy [5].
PI-based triplet regimens comprising the injectable PI, bortezomib (VRd) or carfilzomib (KRd), or the oral PI, ixazomib (IRd), with a lenalidomide and dexamethasone (Rd) backbone are approved and routinely used for the treatment of RRMM in Japan. However, physical, social, and geographic barriers to health service access, burden of repeated administration of injectable drugs, and toxicity may interfere with the long-term delivery of PIs in clinical practice. Both bortezomib and carfilzomib are associated with the development of peripheral neuropathy [6] and cardiotoxicity [7], which are related to cumulative dose. Frequent outpatient visits and hospitalizations may be required during periods of high MM disease activity to control symptoms and manage AEs following initiation of treatment, but once the disease has stabilized, oral treatment options should also be considered [8]. This view is supported by the findings from several studies, which have shown that cancer patients prefer oral over intravenous (IV) administration for reasons including convenience, perceived efficacy, and past experience [8].
The oral PI, ixazomib, is now approved in over 60 countries [9]. In Japan, ixazomib was approved in 2017 [10] in combination with Rd (IRd) for patients with RRMM, and in 2021 as monotherapy for patients with MM as maintenance therapy. A US-based, phase 4, real-world MM-6 study is currently being conducted in patients with NDMM who were previously treated with bortezomib-based therapy prior to enrolment [11]. The purpose of both the MM-6 study and our study is to evaluate the efficacy and safety of switching to oral PI-based treatment, including potential benefits in both patient and health resource burden. It is hoped that switching to IRd will facilitate continuous PI treatment, whilst ensuring clinical outcomes achieved with injectable PI-based treatment are maintained. Although an interim analysis of the ongoing MM-6 study has recently reported the efficacy and safety of switching to IRd in patients with NDMM; to date, the efficacy and safety of switching to IRd following injectable PI-based therapy has not been evaluated in the RRMM setting.
Here, we report the results from a nationwide, multicenter, open-label, single-arm study evaluating the efficacy and safety of treatment with IRd therapy after 3 cycles of injectable PI-based, VRd or KRd, therapy in patients with RRMM from 17 study sites in Japan.
Methods
Study Design and Patients
This was a nationwide, multicenter, open-label, single-arm study conducted in Japanese patients with RRMM in Japan (NCT03416374). Detailed eligibility criteria are provided in Online Resource 1. Briefly, eligible patients were adults aged ≥20 years with RRMM who were not refractory to bortezomib, carfilzomib, or lenalidomide and were considered transplant-ineligible by the investigator, or if considered transplant-eligible, were not planning to undergo stem cell transplantation for ≥12 months. Also, patients must have been planning to start combination therapy with VRd or KRd as second-, third-, or fourth-line therapy, and have an Eastern Cooperative Oncology Group Performance Status (ECOG PS) score of 0−2 (or an ECOG PS of 3 if symptoms were associated with bone lesions only).
Eligible patients received VRd or KRd therapy for 3 cycles. A standard dose of each drug was recommended as per the package insert; however, dosage adjustments were permitted for select patients at the investigator’s discretion. Patients who achieved at least a minor response (MR) to VRd or KRd transitioned to IRd therapy. After transition, oral administration of IRd therapy at a dosage of 4 mg ixazomib on days 1, 8, and 15 plus 25 mg lenalidomide on days 1 through 21, and 40 mg dexamethasone on days 1, 8, 15, and 22, was recommended in 28-day cycles. Dosage adjustments for lenalidomide were permitted in patients with renal impairment, as per the package insert [12]. Dose interruptions/modifications of all three drugs were permitted for toxicities suspected to be related to the specific drugs.
Study drug administration was discontinued if the patient did not meet criteria for transition to IRd treatment (Online Resource 1), or in the event of withdrawal of consent, progressive disease (PD), unacceptable toxicity, significant protocol deviation, death, dropout or loss to follow-up, or if the investigator deemed it necessary. IRd was continued until PD or unacceptable toxicity.
The trial was designed by the steering committee members and the secondary sponsor (Takeda). The protocol was approved by the Certified Review Board and registered with the Ministry of Health, Labour and Welfare (Japan Registry of Clinical Trials). All patients provided written informed consent to participate in the study.
Endpoints
The primary endpoint was the 12-month event-free survival (EFS) rate from the first dose of injectable PI-based therapy, with dropouts, missing response data, PD, and deaths considered as events. Secondary endpoints included: PFS (defined as the period between the first dose of injectable PI-based therapy until the date of confirmed PD or death due to any cause, whichever occurred first) by Kaplan-Meier analysis, with dropouts treated as censoring; OS (defined as the period between the first dose of injectable PI-based therapy until the date of death due to any cause); rate of minimal residual disease (MRD) negativity in bone marrow (BM) in patients who achieved complete response (CR), with MRD negativity defined as the absence of tumour plasma cell within 100 000 BM cells (i.e. <10-5) by single-tube 8-colour multiparameter flow cytometry (MFC) method (SRL-Flow) [13] or 1 000 000 BM cells (i.e. <10-6) by adaptive next-generation sequencing (NGS) [14]; best response (CR, very good partial response [VGPR], partial response [PR], MR, stable disease, PD); overall response rate (ORR; the proportion of patients achieving ≥PR); the proportion of patients achieving VGPR or better; duration of response (DOR; defined as the period between the date of first PR or better and the earliest date of PD or death due to any cause); time to next treatment (TTNT), defined as the period between the first dose of injectable PI-based therapy to the date of the next antitumor treatment or death due to any cause, whichever occurred first; health-related quality of life (HRQOL) and Quality Adjusted Life Years (QALY); healthcare resource utilization (HCRU), including the length of hospital stay and outpatient visits (per person-month) during the initial 3 cycles of injectable PI-based therapy and following IRd treatment; relative dose intensity (RDI) for each IRd study drug (see Online Resource 2 for full description); and safety.
Assessments
Responses were assessed according to the International Myeloma Working Group Uniform Response Criteria (2016) [14]. M-protein in serum and urine was measured at scheduled study visits, with substitution to serum free light chain permitted. BM aspiration was performed in patients suspected of achieving CR during IRd treatment for evaluation of the presence of MRD. HRQOL was assessed using the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire (QLQ)-C30 (v3.0) and EORTC QLQ-MY-20 questionnaires. Questionnaires were administered at baseline and every 3 cycles during IRd treatment, and at the end of treatment/discontinuation.
Safety was evaluated by assessment of treatment-emergent adverse events (TEAEs), including Grade ≥3 and serious adverse events (SAEs) during both VRd/KRd and IRd treatment periods. TEAEs were evaluated and categorised by system organ class (SOC) and preferred term (PT) using MedDRA/J version 24.0. Severity of TEAEs were graded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.03.
Statistical Analysis
The full analysis set (FAS) and safety analysis set (SAS) was defined as all patients who were enrolled and received ≥1 dose of VRd or KRd therapy, and were used for efficacy and safety analyses, respectively. Safety was further evaluated using the secondary safety analysis set (SSAS), defined as all patients who received ≥1 dose of IRd treatment. A 12-month EFS rate, the primary endpoint, of 36% was set as the efficacy threshold for hypothesis testing based on the phase 2 study of VRd in patients with RRMM, in which the median PFS was 9.5 months and the 12-month PFS rate by Kaplan-Meier analysis was 36% [15]. A sample size of 39 patients was set to reject the null hypothesis with at least 80% power with a one-sided significance level of 0.05 under the assumed 57% PFS rate, based on the results of the phase 3 study of IRd in RRMM [16]. Factoring in a discontinuation rate of <20% before transition to IRd treatment (which was counted as events in the primary endpoint), the target number of patients was set as 47 to include 39 patients initiating IRd.
The 12-month EFS rate was compared with 36% using the exact binomial test with one-sided significance level of 5% and the corresponding 90% confidence interval (CI) was estimated. Time-to-event analyses of secondary endpoints (PFS, OS, TTNT, and DOR) were performed using the Kaplan-Meier method, with their 95% CIs.
The modified QALY was calculated by converting the global health/QOL scale score from the EORTC-QLQ-C30 during treatment into a utility value ranging from 0 to 1 and multiplying it by the duration of the treatment effect. Baseline demographics and other secondary endpoints (safety data, best response, HCRU, QOL variables) were summarized using descriptive statistics. The mean, standard deviation (SD), and median (min, max) were calculated for continuous variables, and the frequency number and proportion were calculated for categorical variables.
All statistical analyses were performed using SAS® software version 9.4 (SAS Institute, Cary, NC, USA).
Results
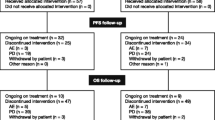
Between Feb 28, 2018 and May 28, 2021, 45 patients were enrolled and received ≥1 dose of VRd or KRd and comprised the FAS and SAS, respectively. Of the 45 patients enrolled, 9 patients discontinued during VRd or KRd therapy because of AEs (n=3), death (n=1), and other reasons (n=5) (Fig. 1). Thirty-six patients (VRd, n=6; KRd, n=30) were eligible to transition to IRd treatment and received ≥1 dose of IRd.
Patient demographics and baseline characteristics are presented in Table 1. Of the 45 patients in the FAS, the mean (SD) age was 70.7 (9.2) years, the median (min, max) number of prior therapies was 2 (1, 4), and 73% and 22% of patients had an ECOG PS of 0 and 1, respectively (Table 1). The numbers of patients previously exposed to bortezomib, carfilzomib, lenalidomide and pomalidomide prior to this study were 32 (71%), 4 (9%), 32 (71%), and 6 (13%), respectively. Four (9%) and 2 (4%) patients had received prior antibody therapy with elotuzumab and daratumumab, respectively.
The median duration of follow-up was 20.8 (95% CI: 17.4−23.7) months.
Efficacy
Primary Endpoint
The 12-month EFS rate was 49% (90% CI: 35.9−62.0) (22/45 patients), which exceeded the threshold of 36%, but the p value (p=0.0518) did not reach the pre-determined level of significance (p=0.05). The counted events were 9 events of PD, 2 deaths, 8 dropouts (discontinuation due to AEs, n=5; not achieving ≥MR during injectable PI treatment, n=1; and other reasons n=2), and 4 patients with missing response data.
Secondary Endpoints
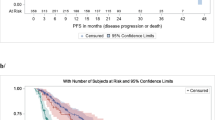
The 12-month PFS rate by Kaplan-Meier analysis (dropouts as censoring) was 74% (95% CI: 56−86) and the median PFS was 29.0 (95% CI: 21.3−NE) months; the median OS was not estimable. The median TTNT and DOR were 32.3 (95% CI: 14.9−35.4) months and 28.0 (95% CI: 20.4−NE) months, respectively. Figure 2 presents PFS and OS in the FAS. A swimmer plot summarizing treatment outcomes for all 45 patients is shown in Fig. 3. The ORR was 73% (95% CI: 58.1−85.4) and the rate of VGPR or better was 42% (95% CI: 27.7−57.8). The best overall response to study treatment was CR in 11 (24%) patients, VGPR in 8 (18%) patients, PR in 14 (31%) patients, MR in 4 (9%) patients, stable disease in 2 (4%) patients, and not evaluable in 6 (13%). Further, the number of patients achieving CR or VGPR increased during IRd treatment (Fig. 4; Online Resource 3).
Of the 11 patients who achieved CR, 7 patients were MRD negative by the SRL-flow method (<10-5) and 3 patients were MRD negative by the NGS method (<10-6). MRD was not measurable by the NGS method in 2 patients. The length of hospital stay, and outpatient visits during the initial 3 cycles of injectable PI-based treatment and following IRd treatment were 5.3 vs 1.0 days per person-month, and 4.2 vs 1.9 visits per person-month, respectively.
The median duration of treatment was 12.4 (95% CI: 8.86−24.79) months. The mean (SD) RDI of ixazomib, lenalidomide, and dexamethasone treatment during IRd therapy was 81% (16.4), 53% (30.5), and 43% (31.8), respectively (Online Resource 4). HRQOL was maintained for the duration of the study treatment (Online Resource 5). With the exception of diarrhea, disease symptoms scores were also maintained. The QALY was 0.518 at 12 months after the start of the study.
Safety
Safety was analysed in 45 patients in the SAS and 36 patients in the SSAS. An overview of the safety profile during IRd therapy (SSAS) and overall from the start of injectable PI-based therapy (SAS) is presented in Table 2. The incidence of common (with an incidence of ≥5%) all grade TEAEs and grade ≥3 TEAEs are presented in Table 3. TEAEs occurred in 41 of 45 patients (91%) in the SAS and in 28 of 36 patients (78.0%) in the SSAS. The most common (≥5 patients) TEAEs of any grade in the SSAS were diarrhea (n=11 [31%]), white blood cell count decreased (n=9 [25%]), and pneumonia (n=5 [14%]). Grade ≥3 TEAEs occurred in 15 of 36 patients (42%) in the SSAS, including white blood cell count decreased, pneumonia and platelet count decreased which were the most common (n=4 [11%] each).
Serious TEAEs occurred in 17 of 45 patients (38%) in the SAS. Of these, events that occurred in ≥2 patient were pneumonia (n=5 [11%]), acute kidney injury and influenza (n=2 [4%] each). Two patients died from TEAEs in the SAS. One died due to pneumonia during IRd treatment and it was considered related to study treatment. The other died of bacterial pneumonia, which was not considered to be related to study treatment. During IRd therapy, 6 of 36 patients (17%) developed TEAEs that led to treatment discontinuation. Five patients discontinued due to diarrhea, gastroenteritis, pneumonia, tibia fracture and interstitial lung disease, respectively. One patient discontinued because of both decreased appetite and taste disorder. Peripheral neuropathy occurred in 3 (8%) patients during IRd treatment. Two (6%) of which were considered related to study treatment; both of these events were grade ≤2.
Discussion
This nationwide, multicenter, open-label, single-arm study was designed to control patients' disease early in treatment with three cycles of injected PI, reduce side effects such as peripheral neuropathy and cardiotoxicity, and reduce the burden of long-term parenteral therapy. Using this approach, the favourable efficacy of IRd therapy following VRd or KRd therapy in patients with RRMM was demonstrated in the real-world setting. The median PFS was 29.0 months, the estimated 12 month PFS rate was 74% when analysed by the Kaplan-Meier method regarding dropouts as censoring, and the ORR was 73%.
The PFS benefit and ORR observed in our study were comparable with those reported with PI-based therapies in other clinical trials in RRMM (Table 4), including the phase 3 study of KRd (median PFS, 26.3 months; ORR: 87.1%),[17] the phase 3 study of IRd (median PFS, 20.6 months; ORR: 78%) [16], and the phase 2 study of IRd (median PFS, 22.0 months; ORR: 84.4%) in Japanese patients [18], despite differences in patient demographics and other background factors. For example, the median age (70.0 years) and proportion of elderly patients (>65 years: 77.8%) in our study was higher than in the phase 3 KRd study [17] (median age: 64.0 years; ≥65 years: 46.7%), and phase 3 [16] (median age: 66 years; >65yr: 53.3%) and Japanese phase 2 [18] (median age: 67 years; >65 years: not reported) IRd studies. There was also a trend towards a higher number of regimens in our study (1 regimen: 49%; 2 regimens: 31%; 3 regimens: 18%; ≥4 regimens: 2%), compared with the phase 3 KRd study [17] (1 regimen: 46.5%; 2 or 3 regimens: 53.3%) and phase 3 [16] (1 regimen: 62.2%; 2 regimens: 26.9%; 3 regimens: 10.8%) and Japanese phase 2 [18] (1 regimen: 61.8%; 2 regimens: 35.3%; 3 regimens: 2.9%) IRd studies. Nevertheless, the PFS and ORR benefits were comparable.
On the other hand, based on the conservative analysis method which counted discontinuation due to AEs and missing response data at 12 months as events, the 12-month EFS rate was 49% (22/45) (primary endpoint). The discrepancy between EFS rates observed for the primary and PFS rate for secondary endpoint mainly derived from the 12 events (discontinuation due to AE [n=5], not achieving ≥MR [n=1], other reasons [n=2], and missing response data [n=4]) other than PD and death. Although it had been taken into account in this study’s design, these discontinuations showed the difficulties with management in the early phase of treatment for RRMM. Nevertheless, the 12-month EFS rate exceeded the pre-specified threshold and suggested the effectiveness of IRd treatment after response was achieved and the disease status was stable. That was also supported by the positive findings for the remaining secondary efficacy endpoints, including TTNT (median 32.3 months), DOR (median, 28.0 months), ORR (73%) and proportion of patients with VGPR or better (42%).
A deepening of response was observed with IRd therapy after injectable PI-based induction. Nine (20.0%) patients achieved VGPR or better and 3 (6.7%) patients achieved a CR with VRd or KRd therapy. Following transition to IRd therapy, 19 (42.2%) patients achieved VGPR or better and 11 (24.4%) patients achieved CR. Of these, 7 (15.6%) patients were MRD negative by the SRL-flow method (<10-5) and the MRD negativity rate was 19.4% (7/36) by this method, which is considered promising for PI-based rescue chemotherapy that does not target CD38 [19].
The results of our study provide data that can be used as a reference for treatment options for patients with RRMM who have a sufficient response to short-term injectable PIs but desire oral drug management. In global phase 3 clinical trials, PI-based therapy has been shown to improve both PFS and OS compared with non-PI-based therapy [1,2,3]. However, real-world outcomes with PI-based therapies have rarely matched those achieved under clinical trial conditions in patients with RRMM [13, 20, 21].
The reason for the discrepancy between clinical trial efficacy and real-world effectiveness is most likely due to differences in patient characteristics as a result of the strict eligibility criteria employed for randomized controlled trials (RCTs). This view is supported by data from the US-based Connect-MM registry and other real-world studies in MM, which show that between 22 and 70% of patients with MM would be considered ineligible for participation in RCTs [22,23,24]. In contrast to RCTs, the patient population seen in clinical practice is typically heterogeneous, with a broader age range, including older and frail patients who are particularly susceptible to toxicities [22].
Importantly, outcomes achieved following transition from injectable PI-based therapies and immunomodulatory drugs under real-world conditions were similar to those achieved in phase 3 clinical studies, including PFS and TTNT (19.2−27.6 vs 17.5−20.6 months, respectively) [20]. Based on the real-world evidence of our study and others [11, 25], transition to ixazomib-based therapy represents an attractive alternative to current regimens for long-term PI-based therapy and may afford patients the similar effectiveness in clinical practice as those seen in RCTs. The length of hospitalization and the number of outpatient visits after changing to oral PI-based therapy were numerically low, which may represent an advantage over injectable PI-based therapy. Treatment strategies such as this study may be useful for patients who may want to reduce their number of hospital visits or for whom hospital visits are an added burden. In addition, QOL was not notably affected throughout the treatment period from injectable PI-based therapy to IRd, and it was confirmed that PI-based treatment was continued. Transition from injectable PI-based therapy to oral PI-based therapy was tolerable in clinical practice, and the safety profile of IRd was similar to, and consistent with previous clinical trial data [16, 18, 26, 27]. TEAEs reported in this study were similar to those reported in the global phase 3 IRd study [16], and no previously unknown safety concerns were identified in this study [28].
This study must also be considered in light of its limitations. Firstly, this was a single-arm study, precluding direct comparisons from being made. The number of patients receiving ixazomib-based therapy in our study was also relatively small, and thus further study in a larger patient population is required to confirm these findings.
In conclusion, this study demonstrated that IRd therapy after injectable PI-based therapy was tolerable and effective for patients with RRMM in the real-world setting. Transition to oral PI-based therapy may be a good option to allow prolonged administration of PI-based therapies, resulting in better outcomes. Our findings add to the evolving body of evidence related to ixazomib and provide additional support for its use.
Change history
11 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00277-023-05355-7
References
Durie BGM, Hoering A, Abidi MH, Rajkumar SV, Epstein J, Kahanic SP, Thakuri M, Reu F, Reynolds CM, Sexton R, Orlowski RZ, Barlogie B, Dispenzieri A (2017) Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOG S0777): a randomised, open-label, phase 3 trial. Lancet 389(10068):519–527. https://doi.org/10.1016/S0140-6736(16)31594-X
San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M, Spicka I, Petrucci MT, Palumbo A, Samoilova OS, Dmoszynska A, Abdulkadyrov KM, Schots R, Jiang B, Mateos MV, Anderson KC, Esseltine DL, Liu K, Cakana A et al (2008) Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med 359(9):906–917. https://doi.org/10.1056/NEJMoa0801479
San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M, Spicka I, Petrucci MT, Palumbo A, Samoilova OS, Dmoszynska A, Abdulkadyrov KM, Delforge M, Jiang B, Mateos MV, Anderson KC, Esseltine DL, Liu K, Deraedt W et al (2013) Persistent overall survival benefit and no increased risk of second malignancies with bortezomib-melphalan-prednisone versus melphalan-prednisone in patients with previously untreated multiple myeloma. J Clin Oncol 31(4):448–455. https://doi.org/10.1200/jco.2012.41.6180
Dimopoulos MA, Moreau P, Palumbo A, Joshua D, Pour L, Hájek R, Facon T, Ludwig H, Oriol A, Goldschmidt H, Rosiñol L, Straub J, Suvorov A, Araujo C, Rimashevskaya E, Pika T, Gaidano G, Weisel K, Goranova-Marinova V et al (2016) Carfilzomib and dexamethasone versus bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma (ENDEAVOR): a randomised, phase 3, open-label, multicentre study. Lancet Oncol 17(1):27–38. https://doi.org/10.1016/s1470-2045(15)00464-7
Ludwig H, Zojer N (2017) Fixed duration vs continuous therapy in multiple myeloma. Hematol Am Soc Hematol 2017(1):212–222. https://doi.org/10.1182/asheducation-2017.1.212
Mauermann M, Dispenzieri A, Staff N (2012) The clinical spectrum of bortezomib-induced peripheral neuropathy (P06.140). Neurol 78(1 Supplement):P06.140–P106.140
Zhai Y, Ye X, Hu F, Xu J, Guo X, Cao Y, Lin Z, Zhou X, Guo Z, He J (2021) Cardiovascular toxicity of carfilzomib: The real-world evidence based on the adverse event reporting system database of the FDA, the United States. Front Cardiovasc Med 8:735466. https://doi.org/10.3389/fcvm.2021.735466
Eek D, Krohe M, Mazar I, Horsfield A, Pompilus F, Friebe R, Shields AL (2016) Patient-reported preferences for oral versus intravenous administration for the treatment of cancer: a review of the literature. Patient Prefer Adherence 10:1609–1621. https://doi.org/10.2147/PPA.S106629
Kumar SK, Berdeja JG, Niesvizky R, Lonial S, Laubach JP, Hamadani M, Stewart AK, Hari P, Roy V, Vescio R, Kaufman JL, Berg D, Liao E, Rajkumar SV, Richardson PG (2019) Ixazomib, lenalidomide, and dexamethasone in patients with newly diagnosed multiple myeloma: long-term follow-up including ixazomib maintenance. Leukemia 33(7):1736–1746. https://doi.org/10.1038/s41375-019-0384-1
Ministry of Health, Labor and Welfare. Ixazomib: Report on the deliberation results. Available from: https://www.pmda.go.jp/files/000225743.pdf. Date Accessed: Jan 18, 2022.
Manda S, Yimer HA, Noga SJ, Girnius S, Yasenchak CA, Charu V, Lyons R, Aiello J, Bogard K, Ferrari RH, Cherepanov D, Demers B, Lu V, Whidden P, Kambhampati S, Birhiray RE, Jhangiani HS, Boccia R, Rifkin RM (2020) Feasibility of long-term proteasome inhibition in multiple myeloma by in-class transition from bortezomib to ixazomib. Clin Lymphoma Myeloma Leuk 20(11):e910–e925. https://doi.org/10.1016/j.clml.2020.06.024
Ning S, Zeller MP (2019) Management of iron deficiency. Hematol 2019(1):315–322. https://doi.org/10.1182/hematology.2019000034
Takamatsu H (2020) Clinical value of measurable residual disease testing for multiple myeloma and implementation in Japan. Int J Hematol 111(4):519–529. https://doi.org/10.1007/s12185-020-02828-7
Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, Munshi N, Lonial S, Bladé J, Mateos MV, Dimopoulos M, Kastritis E, Boccadoro M, Orlowski R, Goldschmidt H, Spencer A, Hou J, Chng WJ, Usmani SZ et al (2016) International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol 17(8):e328–e346. https://doi.org/10.1016/s1470-2045(16)30206-6
Richardson PG, Xie W, Jagannath S, Jakubowiak A, Lonial S, Raje NS, Alsina M, Ghobrial IM, Schlossman RL, Munshi NC, Mazumder A, Vesole DH, Kaufman JL, Colson K, McKenney M, Lunde LE, Feather J, Maglio ME, Warren D et al (2014) A phase 2 trial of lenalidomide, bortezomib, and dexamethasone in patients with relapsed and relapsed/refractory myeloma. Blood 123(10):1461–1469. https://doi.org/10.1182/blood-2013-07-517276
Moreau P, Masszi T, Grzasko N, Bahlis NJ, Hansson M, Pour L, Sandhu I, Ganly P, Baker BW, Jackson SR, Stoppa A-M, Simpson DR, Gimsing P, Palumbo A, Garderet L, Cavo M, Kumar S, Touzeau C, Buadi FK et al (2016) Oral Ixazomib, lenalidomide, and dexamethasone for multiple myeloma. New Engl J Med 374(17):1621–1634. https://doi.org/10.1056/NEJMoa1516282
Stewart AK, Rajkumar SV, Dimopoulos MA, Masszi T, Špička I, Oriol A, Hájek R, Rosiñol L, Siegel DS, Mihaylov GG, Goranova-Marinova V, Rajnics P, Suvorov A, Niesvizky R, Jakubowiak AJ, San-Miguel JF, Ludwig H, Wang M, Maisnar V et al (2014) Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. New Engl J Med 372(2):142–152. https://doi.org/10.1056/NEJMoa1411321
Iida S, Izumi T, Komeno T, Terui Y, Chou T, Ikeda T, Berg D, Fukunaga S, Sugiura K, Sasaki M (2022) A phase 2, open-label, multicenter study of ixazomib plus lenalidomide and dexamethasone in adult Japanese patients with relapsed and/or refractory multiple myeloma. Int J Clin Oncol 27(1):224–233. https://doi.org/10.1007/s10147-021-02030-7
Avet-Loiseau H, Casneuf T, Chiu C, Laubach JP, Lee J-J, Moreau P, Plesner T, Nahi H, Khokhar NZ, Qi M, Schecter J, Carlton V, Qin X, Liu K, Wu K, Zhuang SH, Ahmadi T, Sasser AK, San-Miguel J (2016) Evaluation of Minimal Residual Disease (MRD) in relapsed/refractory multiple myeloma (RRMM) patients treated with daratumumab in combination with lenalidomide plus dexamethasone or bortezomib plus dexamethasone. Blood 128(22):246–246. https://doi.org/10.1182/blood.V128.22.246.246
Richardson PG, San Miguel JF, Moreau P, Hajek R, Dimopoulos MA, Laubach JP, Palumbo A, Luptakova K, Romanus D, Skacel T, Kumar SK, Anderson KC (2018) Interpreting clinical trial data in multiple myeloma: translating findings to the real-world setting. Blood Cancer J 8(11):109. https://doi.org/10.1038/s41408-018-0141-0
Chari A, Richardson PG, Romanus D, Dimopoulos MA, Sonneveld P, Terpos E, Hajek R, Raju A, Palumbo A, Cain LE, Blazer M, Huang H, Farrelly E, Ailawadhi S (2020) Real-world outcomes and factors impacting treatment choice in relapsed and/or refractory multiple myeloma (RRMM): a comparison of VRd, KRd, and IRd. Expert Rev Hematol 13(4):421–433. https://doi.org/10.1080/17474086.2020.1729734
Shah JJ, Abonour R, Gasparetto C, Hardin JW, Toomey K, Narang M, Srinivasan S, Kitali A, Zafar F, Flick ED, Rifkin RM (2017) Analysis of common eligibility criteria of randomized controlled trials in newly diagnosed multiple myeloma patients and extrapolating outcomes. Clin Lymphoma Myeloma Leuk 17(9):575–583.e572. https://doi.org/10.1016/j.clml.2017.06.013
Fiala M, Dukeman J, Stockerl-Goldstein K, Tomasson M, Wildes T, Vij R (2017) The real-world characteristics and outcomes of newly diagnosed myeloma patients ineligible for clinical trials. Clin Lymphoma Myeloma Leuk 17(S1):e55–e56. https://doi.org/10.1016/j.clml.2017.03.101
Hungria VTM, Lee HC, Abonour R, Rifkin RM, Terpos E, Leleu X, Costello CL, van Rhee F, Weisel KC, Puig N, Berdeja JG, Cook G, Usmani SZ, Thompson MA, Boccadoro M, Zonder JA, Spencer A, Hajek R, Fanning SR et al (2019) Real-world (RW) multiple myeloma (MM) patients (Pts) remain under-represented in clinical trials based on standard laboratory parameters and baseline characteristics: Analysis of over 3,000 pts from the Insight MM global, prospective, observational study. Blood 134:1887. https://doi.org/10.1182/blood-2019-125749
Terpos E, Ramasamy K, Maouche N, Minarik J, Ntanasis-Stathopoulos I, Katodritou E, Jenner MW, Plonkova H, Gavriatopoulou M, Vallance GD, Pika T, Kotsopoulou M, Kothari J, Jelinek T, Kastritis E, Aitchison R, Dimopoulos MA, Zomas A, Hajek R (2020) Real-world effectiveness and safety of ixazomib-lenalidomide-dexamethasone in relapsed/refractory multiple myeloma. Ann Hematol 99(5):1049–1061. https://doi.org/10.1007/s00277-020-03981-z
Hou J, Jin J, Xu Y, Wu D, Ke X, Zhou D, Lu J, Du X, Chen X, Li J, Liu J, Gupta N, Hanley MJ, Li H, Hua Z, Wang B, Zhang X, Wang H, van de Velde H et al (2017) Randomized, double-blind, placebo-controlled phase III study of ixazomib plus lenalidomide-dexamethasone in patients with relapsed/refractory multiple myeloma: China Continuation study. J Hematol Oncol 10(1):137. https://doi.org/10.1186/s13045-017-0501-4
Facon T, Venner CP, Bahlis NJ, Offner F, White DJ, Karlin L, Benboubker L, Rigaudeau S, Rodon P, Voog E, Yoon SS, Suzuki K, Shibayama H, Zhang X, Twumasi-Ankrah P, Yung G, Rifkin RM, Moreau P, Lonial S et al (2021) Oral ixazomib, lenalidomide, and dexamethasone for transplant-ineligible patients with newly diagnosed multiple myeloma. Blood 137(26):3616–3628. https://doi.org/10.1182/blood.2020008787
Ninlaro [prescribing information]. Takeda Pharmaceutical Co., Ltd., 2020. Available from: https://www.takeda.com/siteassets/en-ca/home/what-we-do/our-medicines/product-monographs/ninlaro/ninlaro-pm-en.pdf Date Accessed: 25 Jan 2022
Acknowledgments
The authors thank all clinicians for their involvement and contribution to the study. Medical writing support was provided by Jordana Campbell, BSc, CMPP of inScience Communications, Springer Healthcare. This medical writing assistance was funded by Takeda Pharmaceutical Co., Ltd.
Funding
This study was funded by Takeda Pharmaceutical Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data-sharing statement
The datasets, including the redacted study protocol, redacted statistical analysis plan, and individual participants’ data supporting the results reported in this article, will be made available within three months from initial request, to researchers who provide a methodologically sound proposal. The data will be provided after its de-identification, in compliance with applicable privacy laws, data protection and requirements for consent and anonymization.
Authorship contributions
Study design: Yu ABE, Makoto SASAKI, Naoki TAKEZAKO, Takaaki CHOU, Takahiro YOSHIDA, Ikuo MORI, Tomohiro SHINOZAKI, Kenshi SUZUKI; Data acquisition: Yu ABE, Makoto SASAKI, Naoki TAKEZAKO, Shigeki ITO, Kazuhito SUZUKI, Hiroshi HANDA, Takaaki CHOU, Kenshi SUZUKI; Analyses (including statistical): Takahiro YOSHIDA, Ikuo MORI, Tomohiro SHINOZAKI; Interpretation of data: all; Manuscript writing, feedback, and revisions: all.
Ethics approval
The trial was designed by the steering committee members and the secondary sponsor (Takeda). The protocol was approved by the Certified Review Board and registered with the Ministry of Health, Labour and Welfare (Japan Registry of Clinical Trials). The trial was performed in accordance with the ethical standards specified in the 1964 Declaration of Helsinki and its later amendments. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. All patients provided written informed consent to participate in the study.
Competing interests
YA: No conflict/s of interest to disclose.
MS: Payment or honoraria was received from Janssen Pharmaceutical K.K., Takeda Pharmaceutical Co., and Sanofi for lectures, presentations, speaker’s bureaus, manuscript writing or educational events.
NT: No conflict/s of interest to disclose.
SI: Payment or honoraria was received from Takeda Pharmaceutical Co., Janssen, Sanofi, BMS, and Ono Pharmaceutical.
KS: Honoraria for lectures was received from Takeda Pharmaceutical Co., Janssen Pharmaceutical K.K., and Sanofi
HH: Support for the presentation of the manuscript (e.g. funding, provision of study materials, medical writing, article processing charges etc.) was received from Takeda Pharmaceutical Co. Funding for grants was received from Takeda Pharmaceutical Co., BMS, Kyowa-Kirin, Chugai, and Nihon-Shinyaku. Consulting fees were received from Takeda Pharmaceutical Co., Janssen, BMS, Sanofi, and AbbVie. Payment or honoraria was received from Takeda Pharmaceutical Co., Janssen, BMS, Ezai, Sanofi, Ono Pharmaceutical, AbbVie, and Novartis.
TC: No conflict/s of interest to disclose.
TY: Employee of Takeda Pharmaceutical Co.
IM: Employee of Takeda Pharmaceutical Co.
TS: Consulting fees (statistical analyses review), and support for attending a steering committee meeting, were received from Takeda Pharmaceutical Co.
KS: Consulting fees were received from Amgen, Takeda Pharmaceutical Co., and BMS. Payment or honoraria was received from Takeda Pharmaceutical Co., Ono Pharmaceutical, Amgen, Novartis, Sanofi, BMS, AbbVie and Janssen.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: This article was originally published with a needed enhancement on figure 4.
Supplementary Information
Supplementary file 1
(DOCX 2.93 mb)
Supplementary file 2
(DOCX 78.7 kb)
Supplementary file 3
(DOCX 220 kb)
Supplementary file 4
(DOCX 3.19 mb)
Supplementary file 5
(DOCX 9.76 mb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abe, Y., Sasaki, M., Takezako, N. et al. Efficacy and Safety of Ixazomib Plus Lenalidomide and Dexamethasone Following Injectable PI-Based Therapy in Relapsed/Refractory Multiple Myeloma. Ann Hematol 102, 2493–2504 (2023). https://doi.org/10.1007/s00277-023-05212-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05212-7