Abstract
Busulfan and cyclophosphamide (BuCy) is a frequently used myeloablative conditioning regimen for allogeneic hematopoietic cell transplantation (allo-HCT). Theoretical considerations and pharmacological data indicate that application of busulfan prior to subsequent cyclophosphamide (BuCy) may trigger liver toxicity. Reversing the order of application to cyclophosphamide-busulfan (CyBu) might be preferable, a hypothesis supported by animal data and retrospective studies. We performed a prospective randomized trial to determine impact of order of application of Bu and Cy before allo-HCT in 70 patients with hematological malignancy, 33 patients received BuCy and 37 CyBu for conditioning. In the short term, there were minimal differences in liver toxicity favoring CyBu over BuCy, significant only for alanine amino transferase at day 30 (p = 0.03). With longer follow-up at 4 years, non-relapse mortality (6% versus 27%, p = 0.05) was lower and survival (63% versus 43%, p = 0.06) was higher with CyBu compared to BuCy. Other outcomes, such as engraftment (p = 0.21), acute and chronic graft-versus-host disease (p = 0.40; 0.36), and relapse (p = 0.79), were similar in both groups. We prospectively show evidence that the order of application of Cy and Bu in myeloablative conditioning in allo-HCT patients has impact on outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of busulfan and cyclophosphamide (BuCy) is a frequently used established myeloablative conditioning regimen before allogeneic cell transplantation (allo-HCT). Antileukemic effects and myeloablative properties of this regimen in patients with hematological malignancies have been confirmed in multiple studies [1,2,3,4]. Interactions between busulfan (Bu) and cyclophosphamide (Cy) are well described [5, 6]; studies have shown that Bu affects the hepatic metabolism of Cy and may therefore increase liver toxicity when given in this order [7, 8]. The pathophysiology behind this interference is possibly a decrease in levels of glutathione, which is a major player in the breakdown of metabolites of Cy in the hepatocyte [9, 10]. Cy-induced toxicity has been associated with non-relapse mortality (NRM) and decreased survival in clinical studies [11]. The most feared hepatic complication is veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS) described with the BuCy regimen [12,13,14,15]. As suspected in some retrospective clinical and animal studies, reversing the order of application of BuCy to CyBu may decrease liver toxicity without loss in antileukemic activity [6, 16,17,18,19]. In earlier years, when only oral Bu was available, the order of BuCy was preferred because of the emetogenic potential of Cy precluding administration of correct doses of Bu. With the introduction of intravenous Bu, associated with reduced liver complications and mortality [7], these considerations influencing the order of application no longer apply.
With this prospective randomized controlled trial (RCT), we aimed to test the impact of the order of application of BuCy versus CyBu prior to allo-HCT in patients with hematological malignancies.
Patients and methods
Study cohort and design
This is a prospective multicenter (University Hospitals Basel, Zurich, and Geneva) open label 1:1 RCT, comparing the order of application of busulfan followed by cyclophosphamide (BuCy, standard group) versus cyclophosphamide followed by busulfan (CyBu, experimental group) as myeloablative conditioning regimen prior to allo-HCT done between 2013 and 2017. The study was approved by the local ethics committee (EKNZ EKBB179/12), by Swissmedic (2012DR4164) and was registered with ClinicalTrials.gov as NCT01779882. Randomization was centrally at the Clinical Trial Unit (CTU) of the Basel University Hospital.
The primary endpoint, as defined in the protocol, was liver toxicity of BuCy versus CyBu at day 30 after allo-HCT, defined as abnormality in the levels of bilirubin, aspartate amino transferase (ASAT), alanine amino transferase (ALAT), gamma glutamyl transpeptidase (GGT), or alkaline phosphatase (AP). In addition, we used the NCI Common Terminology Criteria for Adverse Events (CTCAE version 4.0) grading of hepatic toxicity [20].
Secondary endpoints were the incidence and severity of VOD, incidence of other organ toxicity before day 30 and at day 100, incidence and severity of acute and chronic GvHD, and overall survival, relapse, and non-relapse mortality incidence at day 100 and at long-term follow-up.
Consenting and included patients were adults planned for myeloablative conditioning allo-HCT to treat acute myeloid leukemia (AML), chronic myeloid leukemia (CML), acute lymphoblastic leukemia (ALL), and myelodysplastic syndrome (MDS) or myeloproliferative neoplasm (MPN). They had an HLA-identical sibling or an allele (10/10) HLA-matched unrelated donor. Patients with preexisting active hepatitis or abnormal pretransplant liver function tests within 2 weeks prior to starting conditioning, such as bilirubin > 3 × upper limit of normal (ULN) or ASAT/ALAT > 5 × ULN, were excluded.
The inclusion goal was set at 72 patients (36 patients in each arm) to ensure 65 evaluable patients considering a drop-out rate of 10%, permitting a difference of 35% in detection of any abnormal liver values between the two groups on days 30 and 100. These assumptions, and hence the accrual goal, were derived from a previous retrospective study comparing CyBu with BuCy [17].
Patient baseline characteristics, such as sex, age, type, and stage of disease, EBMT risk score, hematopoietic cell transplantation-specific comorbidity index (HCT-CI) (Sorror), Karnofsky performance score (KPS), viral serology, specifically hepatitis A, B, and C (HAV, HBV, HCV), cytomegalovirus (CMV) and Ebstein-Barr-virus (EBV), prior autologous or allo-HCT, and transplant characteristics including donor type, sex, age and viral serology, stem cell source, and type of GvHD prophylaxis were recorded.
Liver function tests were measured on the day of enrollment and on days 0, 10, 20, 30, and 100, measuring levels of bilirubin, ASAT, ALAT, GGT, and AP. Outcomes, including time to neutrophil engraftment (defined as the first of 3 consecutive days of an absolute neutrophil count exceeding 0.5 × 109/L), cumulative incidence of VOD, aGvHD, and cGvHD, and grade and treatment, were measured. Survival was defined as time from transplantation to death or last follow-up, relapse was defined as hematologic relapse after allo-HCT, and NRM was death without prior relapse.
Definitions
VOD was defined using the modified Seattle criteria [21] with the occurrence of two of the following events within 20 days of transplantation: hyperbilirubinemia (total serum bilirubin > 34.2 μmol/L (2 mg/dL)), hepatomegaly or right upper quadrant pain of liver origin, and sudden weight gain (> 2% of baseline body weight) because of fluid accumulation.
Acute and chronic GvHD were diagnosed clinically and confirmed histologically when possible. Grading and staging used consensus classifications for acute and chronic GvHD [22, 23]. Acute GvHD was defined as clinically relevant with grade ≥ II.
Treatment
The standard group received the regular conditioning regimen: i.v. Bu (0.8 mg/kg every 6 h, as a 2-h infusion in NaCl 0.9% for a final concentration of 0.5 mg/mL; total 16 doses) from days − 8 to − 4, followed by i.v. Cy (60 mg/kg in 5% glucose) on days − 3 and − 2. Busulfan was started on the evening of day − 8 such that the last dose was given at a time interval of at least 24 h before the first cyclophosphamide dose [8]. The experimental group received i.v. Cy on days − 8 and − 7, and i.v. Bu from days − 5 to − 2, in the same doses but in reversed order (supplementary file study protocol).
Busulfan pharmacokinetic dose adjustment was performed from the fifth dose onward to achieve a target Css from 800 to 1000 ng/mL according to the centers’ guidelines [24]. VOD prophylaxis consisted of intravenous heparin 5000 IU/24 h and ursodeoxycholic acid 250 mg po 3 times daily in two of the centers; one center (7 patients included) did not use VOD prophylaxis. Patients with proven or highly probable VOD were treated with defibrotide i.v. 6.25 mg/kg every 6 h until resolution.
GvHD prophylaxis consisted of cyclosporine A (CsA) (3 mg/kg bw/day i.v.; starting day − 3 over 6 h adjusted to blood trough levels targeting 150-200 μg/L) and methotrexate (MTX) (15 mg/m2 i.v. day + 1; 10 mg/m2 day + 3 and day + 6). In addition, for HCT from unrelated donors and in one center for matched related donors ≥ 40 years [25], ATG (n = 45) or alemtuzumab (n = 3) was used (Table 1). CsA was tapered and discontinued 6 months post-transplant.
Supportive care was as per institutional guidelines and included trimethoprim/sulfamethoxazole, fluconazole, and valacyclovir. Lorazepam was given before Bu to reduce central nervous system adverse reactions.
Statistical analysis
Data are reported as mean or median with standard deviation (SD) or with interquartile range (IQR) as appropriate. Differences among groups were analyzed using Chi-square or Fisher’s exact test for categorical variables, and Student’s t or Mann-Whitney U test for continuous variables, depending on data distributions. Variables significantly associated with outcome in univariate analysis were included in multivariate Cox proportional hazards regression models. All p values were two-sided and statistical significance was determined by a p value < 0.05. Cumulative incidence function of NRM and relapse was performed using death of other causes as competing event, with Fine and Gray to test for differences. The Kaplan-Meier estimator and the log-rank test were used for overall survival. Statistical analysis was performed using the SPSS (version 22; IBM, Chicago, IL, USA) and STATA SE (version 15; StataCorp LLC, College Station, TX, USA) software.
Results
Patient baseline characteristics
Of 114 patients screened, 72 were eligible. Screening failures were mainly because of preexisting liver abnormalities. A total of 72 patients were randomized from 2013 to 2017, and 2 were excluded because of delayed identification of preexisting hepatitis and for donor problems leaving 70 evaluable patients in the trial. Of the 70 evaluable patients, 56 (80%) were treated in center A, 9 (13%) in center B, and 5 (7%) in center C (Table 1). Median age was 47 years and 57% were male. Transplants were from HLA-identical siblings (n = 34, 49%) or from matched unrelated donors (n = 36, 51%). Nine patients had a prior HCT (2 allogeneic and 7 autologous). Median follow-up of surviving patients was 1092 (IQR 730-1364) days. Disease was AML (n = 52, 74%), MDS/MPN (n = 14, 20%), CML (n = 3, 4%), and ALL (n = 1, 2%). Early disease stage (CR (complete remission) or first chronic phase) was in 49 (70%) patients, intermediate (second CR or treated upfront) in 11 (16%), and advanced (no CR) in 10 (14%) patients. A total of 33 patients were randomized to the standard group (BuCy) and 37 to the experimental group (CyBu). Distribution of patient, disease, and transplant characteristics is shown in Table 1 and did not differ significantly among groups.
Liver toxicity and outcomes
Liver function tests measured as bilirubin, ASAT, ALAT, GGT, and AP were not different between groups at baseline (Table 2). The only significant difference was higher levels of ALAT (median 27 versus 22 IU/L, p = 0.03) in the BuCy as compared to the CyBu group on day 30. All other liver function tests did not differ among groups; on day 100, no significant differences were seen.
Slightly more patients in the BuCy as compared to the CyBu group had any grade of CTCAE liver toxicity criteria on day 30 or day 100 (mostly grade 1 toxicity). Even when combining all CTCAE toxicity criteria, differences did not reach statistical significance (p = 0.08).
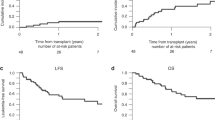
One fatal VOD episode occurred in the BuCy group versus none with CyBu; the frequency of patients fulfilling at least one of the predefined VOD criteria, but not being formally diagnosed with VOD, was significantly higher in BuCy versus CyBu groups (17 versus 10 patients; p = 0.05). Median AUC and Css showed no significant differences between the two groups: AUC (1126 (630-1595) versus 1006 (582-2477) μmol/L*min, p = 0.42) and Css (793 (430-1091) versus 689 (398-1693) ng/mL, p = 0.54) in BuCy versus CyBu in 66 of 70 patients. The cumulative incidence of NRM at 4 years was higher in the BuCy compared to CyBu (27 (15-49)% versus 6 [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]%; p = 0.049, Fig. 1a). Cause of death in patients with NRM did not differ among groups (p = 0.32, see Table 3). The survival probability at 4 years in the BuCy group tended to be lower (43 ± 19% versus 63 ± 17%; p = 0.06, Fig. 1b).
In multivariate analysis adjusting for Karnofsky performance score and hematopoietic cell transplantation-specific comorbidity index, RR of death in the BuCy group compared to CyBu was 2.270 (0.98-5.27), p = 0.056 and corresponding risk of NRM was 4.76 (1.01-22.42), p = 0.049 confirming results of univariate analysis.
Median time to engraftment was similar in both groups (15 [14,15,16] days versus 16 [15,16,17] days, p = 0.27). The cumulative incidence for aGvHD grade ≥ II and cGvHD was similar in BuCy (27 (16-48)% and 39 (25-60)%) compared to CyBu 14 ( [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]%; and 52 (38-72)% respectively; p = 0.20 for aGvHD and p = 0.36 for cGvHD). Relapse at 4 years was observed in a total of 24 patients (12 in BuCy and 12 in CyBu). In both groups, the cumulative incidence of relapse was similar (34 (21-55)% versus 34 (22-55)%; p = 0.79).
Discussion
In this RCT, we compared the order of application of busulfan and cyclophosphamide for myeloablative conditioning before allogeneic cell transplantation in patients with hematological malignancy. Results of this trial support prior hypotheses that the order of application of Cy and Bu may have an impact on short- and long-term toxicity and outcome after allo-HCT. Our study is in line with previous retrospective and animal studies [6, 7, 16,17,18], by showing a somewhat lower early hepatic toxicity and a lower NRM (p = 0.49) at long-term follow-up after transplantation with CyBu compared to BuCy.
Among two retrospective studies, Cantoni et al. described increased liver toxicity at day 30, + higher VOD incidence and higher NRM in BuCy patients compared to CyBu [17]. Rezvani et al. conducted a similar study comparing CyBu to historic BuCy controls, reporting a lower incidence of VOD and a decreased day 100 mortality with CyBu in patients with myelofibrosis. In patients with AML or MDS, NRM differences were not significant [19]. The study discussed here included mainly patients with AML, the study by Rezvani et al., mainly MDS/MPN possibly explaining some differences. As incidence of acute and chronic GvHD and relapse was similar when comparing the CyBu to the BuCy arm in our study, the difference in NRM is not explained by the immunological complication of GvHD or by an impact on malignancy. The difference in long-term NRM is not fully explained by small differences in short-term hepatic toxicity.
Busulfan followed by cyclophosphamide (mostly in that order) is one of the most commonly used myeloablative regimens before allo-HCT; e.g., in patients with AML in the same time period as this trial (2013-2017), 41% of patients reported to the EBMT registry had BuCy as their conditioning regimen (personal communication, M. Labopin). Hassan et al. [8] had shown in a study that the time interval between busulfan and cyclophosphamide was of importance for toxicity. In our trial, this time interval was respected meticulously. In the study by Hassan et al., busulfan had been administered orally and not intravenously.
The hepatotoxicity of BuCy regimen is well described [12,13,14, 26]; one of the pathomechanism of the hepatotoxicity of Bu and Cy is the depletion in glutathione levels, which plays a central role in the metabolism of the toxic metabolites of Cy in hepatocytes [9, 10]. Glutathione depletion as a mechanism of hepatic toxicity had been studied extensively [27,28,29]. The precise pathomechanism remains speculative as we do not have data on glutathione metabolism and other explanations are possible.
While the incidence of VOD has decreased over the years, mortality of established VOD remains high [30]. It is known that inter-individual discrepancy of pharmacokinetics of busulfan impacts on toxicity outcomes [31,32,33]. The introduction of busulfan therapeutic drug monitoring between 2000 and 2010 led to a reduction in adverse outcomes regarding liver toxicity, highlighted by a reduction in the VOD incidence from 15% in the late 1990s to 3% after 2010 after dose adjustment of busulfan during this time period [26, 31]. In our trial, the incidence of severe VOD is 1.4% (one case in 70 patients) and this is comparable to the literature, where incidence of 2-5% has been described [26, 34]. We have to take into account that patients with preexisting liver problems were excluded. Furthermore, when using VOD criteria as defined by Mohty et al. [35], more patients in the BuCy arm had fulfilled at least one criterion than the CyBu arm.
Despite the power of a prospective randomized trial, we acknowledge limitations of this trial: Sample size is limited, and the clinical trial unit did not allow for randomization of a larger patient number, given published differences in retrospective studies [18]. Screening failure was 39% excluding patients with preexisting liver abnormalities, thus assuring the inclusion of patients with normal liver function, best suited to test the study hypothesis. Patient accrual was low because of a general tendency to increasingly use reduced intensity regimens. Randomization was not blinded; however, bias in measuring liver function tests or NRM is unlikely. Furthermore, we saw some heterogeneity based on center’s specific transplant procedures, such as GvHD and other prophylaxis (e.g., ATG use to prevent GvHD, heparin use to prevent VOD), and in diseases of patients randomized.
We found some limited differences in the hepatic toxicity, although the differences are not large and we do not know if they are clinically meaningful. Factors other than the conditioning regimen may impact liver function tests early after HCT. Differences in long-term survival and NRM had not been pre-specified in the study protocol. Causes of death did not differ significantly between groups. It appears that infectious death is more frequent in the ByCy group. Of the 4 infectious deaths, one patient had ATG, one had alemtuzumab, and two had no T cell depletion. Therefore, T cell depletion does not appear to explain small differences in infectious mortality.
Conclusions
In conclusion, we demonstrate that order of application of cyclophosphamide and busulfan may influence outcome when used in myeloablative conditioning for hematological malignancy. Additional data need to be generated on pharmacology of drugs used in conditioning to achieve safer individualized chemotherapeutic treatment.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Socié G, Clift RA, Blaise D, Devergie A, Ringden O, Martin PJ et al (2001) Busulfan plus cyclophosphamide compared with total-body irradiation plus cyclophosphamide before marrow transplantation for myeloid leukemia: long-term follow-up of 4 randomized studies. Blood. 98(13):3569–3574
Ruutu T, van der Werf S, van Biezen A, Backman JT, Peczynski C, Kröger N, Mohty M, Nagler A, Montoto S, Langebrake C, Niederwieser D, Peric Z, Koenecke C, Duarte RF, Basak G (2019) Use of busulfan in conditioning for allogeneic hematopoietic stem cell transplantation in adults: a survey by the Transplant Complications Working Party of the EBMT. Bone Marrow Transplant 54(12):2013–2019
Hassan M (1999) The role of busulfan in bone marrow transplantation. Med Oncol Northwood Lond Engl 16(3):166–176
Clift RA, Buckner CD, Thomas ED, Bensinger WI, Bowden R, Bryant E, Deeg HJ, Doney KC, Fisher LD, Hansen JA (1994) Marrow transplantation for chronic myeloid leukemia: a randomized study comparing cyclophosphamide and total body irradiation with busulfan and cyclophosphamide. Blood. 84(6):2036–2043
Nilsson C, Aschan J, Hentschke P, Ringdén O, Ljungman P, Hassan M (2003) The effect of metronidazole on busulfan pharmacokinetics in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 31(6):429–435
Méresse V, Hartmann O, Vassal G, Benhamou E, Valteau-Couanet D, Brugieres L, Lemerle J (1992) Risk factors for hepatic veno-occlusive disease after high-dose busulfan-containing regimens followed by autologous bone marrow transplantation: a study in 136 children. Bone Marrow Transplant 10(2):135–141
McCune JS, Batchelder A, Deeg HJ, Gooley T, Cole S, Phillips B et al (2007) Cyclophosphamide following targeted oral busulfan as conditioning for hematopoietic cell transplantation: pharmacokinetics, liver toxicity, and mortality. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 13(7):853–862
Hassan M, Ljungman P, Ringdén O, Hassan Z, Oberg G, Nilsson C et al (2000) The effect of busulphan on the pharmacokinetics of cyclophosphamide and its 4-hydroxy metabolite: time interval influence on therapeutic efficacy and therapy-related toxicity. Bone Marrow Transplant 25(9):915–924
DeLeve LD, Wang X (2000) Role of oxidative stress and glutathione in busulfan toxicity in cultured murine hepatocytes. Pharmacology. 60(3):143–154
Hassan Z, Hellström-Lindberg E, Alsadi S, Edgren M, Hägglund H, Hassan M (2002) The effect of modulation of glutathione cellular content on busulphan-induced cytotoxicity on hematopoietic cells in vitro and in vivo. Bone Marrow Transplant 30(3):141–147
McDonald GB, Slattery JT, Bouvier ME, Ren S, Batchelder AL, Kalhorn TF et al (2003) Cyclophosphamide metabolism, liver toxicity, and mortality following hematopoietic stem cell transplantation. Blood. 101(5):2043–2048
Brodsky R, Topolsky D, Crilley P, Bulova S, Brodsky I (1990) Frequency of veno-occlusive disease of the liver in bone marrow transplantation with a modified busulfan/cyclophosphamide preparative regimen. Am J Clin Oncol 13(3):221–225
Vassal G, Hartmann O, Benhamou E (1990) Busulfan and veno-occlusive disease of the liver. Ann Intern Med 112(11):881
Ljungman P, Hassan M, Békássy AN, Ringdén O, Oberg G (1997) High busulfan concentrations are associated with increased transplant-related mortality in allogeneic bone marrow transplant patients. Bone Marrow Transplant 20(11):909–913
Tsakiris DA, Tichelli A (2009) Thrombotic complications after haematopoietic stem cell transplantation: early and late effects. Best Pract Res Clin Haematol 22(1):137–145
Sadeghi B, Jansson M, Hassan Z, Mints M, Hägglund H, Abedi-Valugerdi M, Hassan M (2008) The effect of administration order of BU and CY on engraftment and toxicity in HSCT mouse model. Bone Marrow Transplant 41(10):895–904
Cantoni N, Gerull S, Heim D, Halter J, Bucher C, Buser A, Tsakiris DA, Passweg J, Tichelli A, Stern M, Gratwohl A (2011) Order of application and liver toxicity in patients given BU and CY containing conditioning regimens for allogeneic hematopoietic SCT. Bone Marrow Transplant 46(3):344–349
Nilsson C, Forsman J, Hassan Z, Abedi-Valugerdi M, O’Connor C, Concha H et al (2005) Effect of altering administration order of busulphan and cyclophosphamide on the myeloablative and immunosuppressive properties of the conditioning regimen in mice. Exp Hematol 33(3):380–387
Rezvani AR, McCune JS, Storer BE, Batchelder A, Kida A, Deeg HJ et al (2013) Cyclophosphamide followed by intravenous targeted busulfan for allogeneic hematopoietic cell transplantation: pharmacokinetics and clinical outcomes. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 19(7):1033–1039
Common Terminology Criteria for Adverse Events (CTCAE) (2009) 79.
McDonald GB, Hinds MS, Fisher LD, Schoch HG, Wolford JL, Banaji M, Hardin BJ, Shulman HM, Clift RA (1993) Veno-occlusive disease of the liver and multiorgan failure after bone marrow transplantation: a cohort study of 355 patients. Ann Intern Med 118(4):255–267
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, Thomas ED (1995) 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 15(6):825–828
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, Martin P, Chien J, Przepiorka D, Couriel D, Cowen EW, Dinndorf P, Farrell A, Hartzman R, Henslee-Downey J, Jacobsohn D, McDonald G, Mittleman B, Rizzo JD, Robinson M, Schubert M, Schultz K, Shulman H, Turner M, Vogelsang G, Flowers MED (2005) National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant 11:945–956
Yeh RF, Pawlikowski MA, Blough DK, McDonald GB, O’Donnell PV, Rezvani A, Deeg HJ, McCune JS (2012) Accurate targeting of daily intravenous busulfan with 8-hour blood sampling in hospitalized adult hematopoietic cell transplant recipients. Biol Blood Marrow Transplant 18(2):265–272
Binkert L, Medinger M, Halter JP, Heim D, Gerull S, Holbro A, Lengerke C, Weisser M, Passweg JR (2015) Lower dose anti-thymocyte globulin for GvHD prophylaxis results in improved survival after allogeneic stem cell transplantation. Bone Marrow Transplant 50(10):1331–1336
El-Serafi I, Remberger M, Ringdèn O, Törlén J, Sundin M, Björklund A et al (2020) Reduced risk of sinusoidal obstruction syndrome of the liver after busulfan-cyclophosphamide conditioning prior to allogeneic hematopoietic stem cell transplantation. Clin Transl Sci 13(2):293–300
Ansari M, Curtis PH-D, Uppugunduri CRS, Rezgui MA, Nava T, Mlakar V, Lesne L, Théoret Y, Chalandon Y, Dupuis LL, Schechter T, Bartelink IH, Boelens JJ, Bredius R, Dalle JH, Azarnoush S, Sedlacek P, Lewis V, Champagne M, Peters C, Bittencourt H, Krajinovic M (2017) GSTA1 diplotypes affect busulfan clearance and toxicity in children undergoing allogeneic hematopoietic stem cell transplantation: a multicenter study. Oncotarget. 8(53):90852–90867
Bonifazi F, Storci G, Bandini G, Marasco E, Dan E, Zani E, Albani F, Bertoni S, Bontadini A, de Carolis S, Sapienza MR, Rizzi S, Motta MR, Ferioli M, Garagnani P, Cavo M, Mantovani V, Bonafe M (2014) Glutathione transferase-A2 S112T polymorphism predicts survival, transplant-related mortality, busulfan and bilirubin blood levels after allogeneic stem cell transplantation. Haematologica. 99(1):172–179
Terakura S, Onizuka M, Fukumoto M, Kuwatsuka Y, Kohno A, Ozawa Y et al (2020) Analysis of glutathione S-transferase and cytochrome P450 gene polymorphism in recipients of dose-adjusted busulfan-cyclophosphamide conditioning. Int J Hematol 111(1):84–92
Coppell JA, Richardson PG, Soiffer R, Martin PL, Kernan NA, Chen A, Guinan E, Vogelsang G, Krishnan A, Giralt S, Revta C, Carreau NA, Iacobelli M, Carreras E, Ruutu T, Barbui T, Antin JH, Niederwieser D (2010) Hepatic veno-occlusive disease following stem cell transplantation: incidence, clinical course, and outcome. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 16(2):157–168
Bleyzac N, Souillet G, Magron P, Janoly A, Martin P, Bertrand Y, Galambrun C, Dai Q, Maire P, Jelliffe RW, Aulagner G (2001) Improved clinical outcome of paediatric bone marrow recipients using a test dose and Bayesian pharmacokinetic individualization of busulfan dosage regimens. Bone Marrow Transplant 28(8):743–751
Copelan EA, Bechtel TP, Avalos BR, Elder PJ, Ezzone SA, Scholl MD, Penza SL (2001) Busulfan levels are influenced by prior treatment and are associated with hepatic veno-occlusive disease and early mortality but not with delayed complications following marrow transplantation. Bone Marrow Transplant 27(11):1121–1124
Masson E, Zamboni WC (1997) Pharmacokinetic optimisation of cancer chemotherapy. Effect on outcomes. Clin Pharmacokinet 32(4):324–343
McCune JS, Gibbs JP, Slattery JT (2000) Plasma concentration monitoring of busulfan: does it improve clinical outcome? Clin Pharmacokinet 39(2):155–165
Mohty M, Malard F, Abecassis M, Aerts E, Alaskar AS, Aljurf M, Arat M, Bader P, Baron F, Bazarbachi A, Blaise D, Ciceri F, Corbacioglu S, Dalle JH, Dignan F, Fukuda T, Huynh A, Masszi T, Michallet M, Nagler A, NiChonghaile M, Okamoto S, Pagliuca A, Peters C, Petersen FB, Richardson PG, Ruutu T, Savani BN, Wallhult E, Yakoub-Agha I, Duarte RF, Carreras E (2016) Revised diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a new classification from the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant 51(7):906–912
Acknowledgments
The authors acknowledge the clinicians and nurses at associated transplant centers who treated the patients and also the patients who participated in this study.
Funding
Open access funding provided by University of Basel. This work was financially supported by Baxter SA and Robapharm/Pierre Fabre SA with unrestricted funding for the administrative costs.
Author information
Authors and Affiliations
Contributions
CS, MM, and JRP analyzed the date and wrote the paper. NC, MA, JRP, and SG reviewed the literature and designed the study. SG, JH, DH, MM, YC, SML, US, and GN performed the trial. JRP and PS performed the statistical analysis. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was approved by the local ethics committee (EKNZ EKBB179/12), by Swissmedic (2012DR4164) and was registered with ClinicalTrials.gov as NCT01779882.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All of the authors have agreed with the publication.
Code availability
Statistical analysis was performed using the SPSS (version 22; IBM, Chicago, IL, USA) and STATA SE (version 15; StataCorp LLC, College Station, TX, USA) software.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 1551 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seydoux, C., Medinger, M., Gerull, S. et al. Busulfan-cyclophosphamide versus cyclophosphamide-busulfan as conditioning regimen before allogeneic hematopoietic cell transplantation: a prospective randomized trial. Ann Hematol 100, 209–216 (2021). https://doi.org/10.1007/s00277-020-04312-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-020-04312-y