Abstract
Purpose
This study aimed to elucidate whether immediate angiography within 30 min is associated with lower in-hospital mortality compared with non-immediate angiography.
Materials and Methods
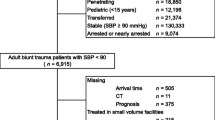
We conducted a retrospective cohort study using a nationwide trauma databank (2019–2020). Adult trauma patients who underwent emergency angiography within 12 h after hospital arrival were included. Patients who underwent surgery before angiography were excluded. Immediate angiography was defined as one performed within 30 min after arrival (door-to-angio time ≤ 30 min). In-hospital mortality and non-operative management (NOM) failure were compared between patients with immediate and non-immediate angiography. Inverse probability weighting with propensity scores was conducted to adjust patient demographics, injury mechanism and severity, vital signs on hospital arrival, and resuscitative procedures. A restricted cubic spline curve was drawn to reveal survival benefits by door-to-angio time.
Results
Among 1,455 patients eligible for this study, 92 underwent immediate angiography. Angiography ≤ 30 min was associated with decreased in-hospital mortality (5.0% vs 11.1%; adjusted odds ratio [OR], 0.42 [95% CI, 0.31–0.56]; p < 0.001), as well as lower frequency of NOM failure: thoracotomy and laparotomy after angiography (0.8% vs. 1.8%; OR, 0.44 [0.22–0.89] and 2.6% vs. 6.5%; OR, 0.38 [0.26–0.56], respectively). The spline curve showed a linear association between increasing mortality and prolonged door-to-angio time in the initial 100 min after arrival.
Conclusion
In trauma patients, immediate angiography ≤ 30 min was associated with lower in-hospital mortality and fewer NOM failures.
Level of Evidence
Level 3b, non randomized controlled cohort/follow up study.
Graphical Abstract



Similar content being viewed by others
References
Matsushima K, Hogen R, Piccinini A, et al. Adjunctive use of hepatic angioembolization following hemorrhage control laparotomy. J Trauma Acute Care Surg. 2020;88(5):636–43.
Zarzaur BL, Kozar R, Myers JG, et al. The splenic injury outcomes trial: an American association for the surgery of trauma multi-institutional study. J Trauma Acute Care Surg. 2015;79(3):335–42.
Sabe AA, Claridge JA, Rosenblum DI, Lie K, Malangoni MA. The effects of splenic artery embolization on nonoperative management of blunt splenic injury: a 16-year experience. J Trauma Acute Care Surg. 2009;67(3):565–72.
Shapiro M, McDonald AA, Knight D, Johannigman JA, Cuschieri J. The role of repeat angiography in the management of pelvic fractures. J Trauma Acute Care Surg. 2005;58(2):227–31.
Miller PR, Chang MC, Hoth JJ, et al. Prospective trial of angiography and embolization for all grade III to V blunt splenic injuries: nonoperative management success rate is significantly improved. J Am Coll Surg. 2014;218(4):644–8.
Virdis F, Reccia I, Di Saverio S, et al. Clinical outcomes of primary arterial embolization in severe hepatic trauma: a systematic review. Diagn Interv Imaging. 2019;100(2):65–75.
Matsushima K, Piccinini A, Schellenberg M, et al. Effect of door-to-angioembolization time on mortality in pelvic fracture: every hour of delay counts. J Trauma Acute Care Surg. 2018;84(5):685–92.
Tanizaki S, Maeda S, Matano H, Sera M, Nagai H, Ishida H. Time to pelvic embolization for hemodynamically unstable pelvic fractures may affect the survival for delays up to 60 min. Injury. 2014;45(4):738–41.
American College of Surgeon. Resources for Optimal Care of the Injured Patient (2022 Standards). Available at: https://www.facs.org/quality-programs/trauma/quality/verification-review-and-consultation-program/standards/. Accessed 2022.
Jarvis S, Orlando A, Blondeau B, et al. Variability in the timeliness of interventional radiology availability for angioembolization of hemodynamically unstable pelvic fractures: a prospective survey among U.S. level I trauma centers. Patient Saf Surg. 2019;13:23.
Cannon JW, Khan MA, Raja AS, et al. Damage control resuscitation in patients with severe traumatic hemorrhage: a practice management guideline from the Eastern Association for the surgery of trauma. J Trauma Acute Care Surg. 2017;82(3):605–17.
Yamamoto R, Cestero RF, Muir MT, et al. Delays in surgical intervention and temporary hemostasis using resuscitative endovascular balloon occlusion of the aorta (REBOA): influence of time to operating room on mortality. Am J Surg. 2020;220(6):1485–91.
Yamamoto R, Cestero RF, Yoshizawa J, Maeshima K, Sasaki J. Emergency angiography for trauma patients and potential association with acute kidney injury. World J Emerg Surg. 2021;16(1):56.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424.
Austin PC, Stuart EA. The performance of inverse probability of treatment weighting and full matching on the propensity score in the presence of model misspecification when estimating the effect of treatment on survival outcomes. Stat Methods Med Res. 2017;26(4):1654–70.
Rubin DB, Schenker N. Multiple imputation in health-are databases: an overview and some applications. Stat Med. 1991;10(4):585–98.
Lam SW, Lingsma HF, van Beeck EF, Leenen LP. Validation of a base deficit-based trauma prediction model and comparison with TRISS and ASCOT. Eur J Trauma Emerg Surg. 2016;42(5):627–33.
Maeshima K, Yamamoto R, Sasaki J. Trauma-Angio score as a predictor of urgent angioembolization for blunt trauma: development and validation using independent cohorts. Eur J Trauma Emerg Surg. 2022;48(6):4837–45.
Raux M, Sartorius D, Le Manach Y, David JS, Riou B, Vivien B. What do prehospital trauma scores predict besides mortality? J Trauma. 2011;71(3):754–9.
Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163(12):1149–56.
Bugaev N, Como JJ, Golani G, et al. Thromboelastography and rotational thromboelastometry in bleeding patients with coagulopathy: practice management guideline from the Eastern association for the surgery of trauma. J Trauma Acute Care Surg. 2020;89(6):999–1017.
Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471–82.
Bilello JF, Sharp VL, Dirks RC, Kaups KL, Davis JW. After the embo: predicting non-hemorrhagic indications for splenectomy after angioembolization in patients with blunt trauma. Trauma Surg Acute Care Open. 2018;3(1):e000159.
Gill S, Hoff J, Mila A, Sanchez C, McKenney M, Elkbuli A. Post-traumatic splenic injury outcomes for nonoperative and operative management: a systematic review. World J Surg. 2021;45(7):2027–36.
Coccolini F, Montori G, Catena F, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg. 2017;12:40.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Stassen NA, Bhullar I, Cheng JD, et al. Nonoperative management of blunt hepatic injury: an Eastern Association for the surgery of trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 Suppl 4):S288-293.
Acknowledgements
None
Funding
There is no funding source in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant conflicts of interest to disclose.
Ethical Approval
This study was approved by the Institutional Review Board of the Keio University School of Medicine (application number: 20090087). The requirement for informed consent was waived because of the anonymous nature of the data being used.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamamoto, R., Maeshima, K., Funabiki, T. et al. Immediate Angiography and Decreased In-Hospital Mortality of Adult Trauma Patients: A Nationwide Study. Cardiovasc Intervent Radiol 47, 472–480 (2024). https://doi.org/10.1007/s00270-024-03664-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-024-03664-6