Abstract
Purpose
To determine whether instillation of normal saline solution for sealing the needle track reduces incidence of pneumothorax and chest tube placement after computed tomography-guided percutaneous lung biopsy.
Materials and Methods
A total of 242 computed tomography-guided percutaneous lung biopsies performed at a single institution were retrospectively reviewed, including 93 biopsies in which the needle track was sealed by instillation of 3–5 ml of normal saline solution during needle withdrawal (water seal group) and 149 biopsies without sealing (control group). Patient and lesion characteristics, procedure-specific variables, pneumothorax and chest tube placement rates were recorded.
Results
Baseline characteristics were comparable in both groups. There was a statistically significant decrease in the pneumothorax rate (19.4% [18/93] vs. 40.9% [61/149]; p < 0.001) and a numerically lower chest tube placement rate without significant reduction (4.3% [4/93] vs. 10.7% [16/149]; p = 0.126) with using normal saline instillation for sealing the needle track versus not using sealant material. Using a multiple logistic regression analysis, using normal saline instillation to seal the needle track, having a senior radiologist as operator of the procedure and putting patients in prone position were significantly associated with a decreased risk of pneumothorax. The presence of emphysema along the needle track was significantly associated with an increased risk of pneumothorax. No complication was observed due to normal saline injection.
Conclusion
Normal saline solution instillation for sealing the needle track after computed tomography-guided percutaneous lung biopsy is a simple, low-cost and safe technique resulted in significantly decreased pneumothorax occurrence and a numerically lower chest tube placement rate, and might help to reduce both hospitalization risks and costs for the healthcare system.
Level of evidence 3 Non-controlled retrospective cohort study.
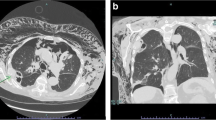
Graphical Abstract



Similar content being viewed by others
References
Manhire A. Guidelines for radiologically guided lung biopsy. Thorax. 2003;58(11):920–36.
Winokur R, Pua B, Sullivan B, Madoff D. Percutaneous lung biopsy: technique, efficacy, and complications. Semin Interv Radiol. 2013;30(02):121–7.
Wang Y, Jiang F, Tan X, Tian P. CT-guided percutaneous transthoracic needle biopsy for paramediastinal and nonparamediastinal lung lesions: diagnostic yield and complications in 1484 patients. Medicine (Baltimore). 2016;95(31): e4460.
Takeshita J, Masago K, Kato R, Hata A, Kaji R, Fujita S, et al. CT-guided fine-needle aspiration and core needle biopsies of pulmonary lesions: a single-center experience with 750 biopsies in Japan. Am J Roentgenol. 2015;204(1):29–34.
Yang W, Sun W, Li Q, Yao Y, Lv T, Zeng J, et al. Diagnostic accuracy of CT-guided transthoracic needle biopsy for solitary pulmonary nodules. PLOS ONE. 2015;10(6): e0131373.
Li Y, Du Y, Yang HF, Yu JH, Xu XX. CT-guided percutaneous core needle biopsy for small (≤20 mm) pulmonary lesions. Clin Radiol. 2013;68(1):e43–8.
Gupta S, Krishnamurthy S, Broemeling LD, Morello FA, Wallace MJ, Ahrar K, et al. Small (≤2-cm) subpleural pulmonary lesions: short- versus long-needle-path CT-guided biopsy—comparison of diagnostic yields and complications. Radiology. 2005;234(2):631–7.
Heerink WJ, de Bock GH, de Jonge GJ, Groen HJM, Vliegenthart R, Oudkerk M. Complication rates of CT-guided transthoracic lung biopsy: meta-analysis. Eur Radiol. 2017;27(1):138–48.
Gupta S, Wallace MJ, Cardella JF, Kundu S, Miller DL, Rose SC. Quality improvement guidelines for percutaneous needle biopsy. J Vasc Interv Radiol. 2010;21(7):969–75.
Gurley MB, Richli WR, Waugh KA. Outpatient management of pneumothorax after fine-needle aspiration: economic advantages for the hospital and patient. Radiology. 1998;209(3):717–22.
Lokhandwala T, Dann R, Johnson M, D’Souza AO. Costs of the diagnostic workup for lung cancer: a medicare claims analysis. Int J Radiat Oncol. 2014;90(5):S9-10.
Bourgouin PM, Shepard JA, McLoud TC, Spizarny DL, Dedrick CG. Transthoracic needle aspiration biopsy: evaluation of the blood patch technique. Radiology. 1988;166(1):93–5.
Herman SJ, Weisbrod GL. Usefulness of the blood patch technique after transthoracic needle aspiration biopsy. Radiology. 1990;176(2):395–7.
Lang EK, Ghavami R, Schreiner VC, Archibald S, Ramirez J. Autologous blood clot seal to prevent pneumothorax at CT-guided lung biopsy. Radiology. 2000;216(1):93–6.
Malone LJ, Stanfill RM, Wang H, Fahey KM, Bertino RE. Effect of intraparenchymal blood patch on rates of pneumothorax and pneumothorax requiring chest tube placement after percutaneous lung biopsy. Am J Roentgenol. 2013;200(6):1238–43.
Graffy P, Loomis SB, Pickhardt PJ, Lubner MG, Kitchin DR, Lee FT, et al. Pulmonary intraparenchymal blood patching decreases the rate of pneumothorax-related complications following percutaneous CT–guided needle biopsy. J Vasc Interv Radiol. 2017;28(4):608-613.e1.
Maybody M, Muallem N, Brown KT, Moskowitz CS, Hsu M, Zenobi CL, et al. Autologous blood patch injection versus hydrogel plug in CT-guided lung biopsy: a prospective randomized trial. Radiology. 2019;290(2):547–54.
Petsas T, Siamblis D, Giannakenas C, Tepetes K, Dougenis D, Spiropoulos K, et al. Fibrin glue for sealing the needle track in fine-needle percutaneous lung biopsy using a coaxial system: part II–clinical study. Cardiovasc Intervent Radiol. 1995;18(6):378–82.
Engeler CE, Hunter DW, Castaneda-Zuniga W, Tashjian JH, Yedlicka JW, Amplatz K. Pneumothorax after lung biopsy: prevention with transpleural placement of compressed collagen foam plugs. Radiology. 1992;184(3):787–9.
Zaetta JM, Licht MO, Fisher JS, Avelar RL. A lung biopsy tract plug for reduction of postbiopsy pneumothorax and other complications: results of a prospective, multicenter, randomized, controlled clinical study. J Vasc Interv Radiol. 2010;21(8):1235-1243.e3.
Ahrar JU, Gupta S, Ensor JE, Mahvash A, Sabir SH, Steele JR, et al. Efficacy of a self-expanding tract sealant device in the reduction of pneumothorax and chest tube placement rates after percutaneous lung biopsy: a matched controlled study using propensity score analysis. Cardiovasc Intervent Radiol. 2017;40(2):270–6.
Grage RA, Naveed MA, Keogh S, Wang D. Efficacy of a dehydrated hydrogel plug to reduce complications associated with computed tomography–guided percutaneous transthoracic needle biopsy. J Thorac Imaging. 2017;32(1):57–62.
Tran AA, Brown SB, Rosenberg J, Hovsepian DM. Tract embolization with gelatin sponge slurry for prevention of pneumothorax after percutaneous computed tomography-guided lung biopsy. Cardiovasc Interv Radiol. 2014;37(6):1546–53.
Baadh AS, Hoffmann JC, Fadl A, Danda D, Bhat VR, Georgiou N, et al. Utilization of the track embolization technique to improve the safety of percutaneous lung biopsy and/or fiducial marker placement. Clin Imaging. 2016;40(5):1023–8.
Huo YR, Chan MV, Habib AR, Lui I, Ridley L. Post-biopsy manoeuvres to reduce pneumothorax incidence in CT-guided transthoracic lung biopsies: a systematic review and meta-analysis. Cardiovasc Intervent Radiol. 2019;42(8):1062–72.
Billich C, Muche R, Brenner G, Schmidt SA, Krüger S, Brambs HJ, et al. CT-guided lung biopsy: incidence of pneumothorax after instillation of NaCl into the biopsy track. Eur Radiol. 2008;18(6):1146–52.
Li Y, Du Y, Luo TY, Yang HF, Yu JH, Xu XX, et al. Usefulness of normal saline for sealing the needle track after CT-guided lung biopsy. Clin Radiol. 2015;70(11):1192–7.
Babu SB, Srinivasan S, Chung R, Chawla A, Tan HK, Lohan R. Tract sealing with normal saline after percutaneous transthoracic lung biopsies. J Med Imaging Radiat Oncol. 2020;64(2):211–4.
Huo YR, Chan MV, Habib AR, Lui I, Ridley L. Pneumothorax rates in CT-Guided lung biopsies: a comprehensive systematic review and meta-analysis of risk factors. Br J Radiol. 2020;93(1108):20190866.
Cox JE, Chiles C, McManus CM, Aquino SL, Choplin RH. Transthoracic needle aspiration biopsy: variables that affect risk of pneumothorax. Radiology. 1999;212(1):165–8.
Lim CS, Tan LE, Wang JY, Lee CH, Chang HC, Lan CC, et al. Risk factors of pneumothorax after CT-guided coaxial cutting needle lung biopsy through aerated versus nonaerated lung. J Vasc Interv Radiol. 2014;25(8):1209–17.
McCartney R, Tait D, Stilson M, Seidel GF. A technique for the prevention of pneumothorax in pulmonary aspiration biopsy. Am J Roentgenol. 1974;120(4):872–5.
McCartney RL. Further observations on the lung patch technique: with analysis of the first 50 cases. Am J Roentgenol. 1975;124(3):397–403.
Clayton JD, Elicker BM, Ordovas KG, Kohi MP, Nguyen J, Naeger DM. Nonclotted blood patch technique reduces pneumothorax and chest tube placement rates after percutaneous lung biopsies. J Thorac Imaging. 2016;31(4):243–6. https://doi.org/10.1097/RTI.0000000000000215.
Khorochkov E, Garvin GJ, Potoczny S, Kozak RI. Injection of saline into the biopsy tract and rapid patient rollover decreases pneumothorax size following computed tomography-guided transthoracic needle biopsy. Can Assoc Radiol J. 2018;69(4):489–92.
Acknowledgements
The graphical abstract was partly generated using Servier Medical Art, provided by Servier, licensed under a Creative Commons Attribution 3.0 unported license.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Consent for Publication
For this type of study, consent for publication is not required.
Informed Consent
This study has obtained IRB approval from CERIM (Comité d’Ethique pour la Recherche en Imagerie Médicale), and the need for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Incidence of pneumothorax and chest tube placement in studies using a sealant material.
Study | Pneumothorax | Chest tube placement | ||||
|---|---|---|---|---|---|---|
Sealant (%) | Control (%) | OR [95% CI] | Sealant (%) | Control (%) | OR [95% CI] | |
Normal saline | ||||||
Billich [26] | 6/70 (8.6%) | 24/70 (34.3%) | 0.18 [0.07–0.48] | 1/70 (1.4%) | 8/70 (11.4%) | 0.11 [0.01–0.92] |
Li [27] | 10/161 (6.2%) | 42/161 (26.1%) | 0.19 [0.09–0.39] | 1/161 (0.6%) | 9/161 (5.6%) | 0.11 [0.01–0.84] |
Babu [28] | 32/100 (32%) | 46/100 (46%) | 0.55 [0.31–0.98] | 1/100 (1%) | 7/100 (7%) | 0.13 [0.02–1.11] |
Tract plug | ||||||
Engeler [19] | 2/25 (8%) | 7/25 (28%) | 0.22 [0.04–1.21] | 2/25 (8%) | 2/25 (8%) | 1 [0.13–7.72] |
Petsas [18] | 5/26 (19.2%) | 13/32 (40.6%) | 0.35 [0.10–1.16] | 1/26 (3.8%) | 6/32 (18.8%) | 0.17 [0.02–1.54] |
Zaetta [20] | 30/170 (17.6%) | 53/169 (31.4%) | 0.47 [0.28–0.78] | 6/170 (3.5%) | 18/169 (10.7%) | 0.31 [0.12–0.79] |
Baadh [24] | 11/125 (8.8%) | 26/124 (21%) | 0.36 [0.17–0.77] | 5/125 (4%) | 10/124 (8.1%) | 0.48 [0.16–1.43] |
Ahrar [21] | 66/317 (20.8%) | 104/317 (32.8%) | 0.54 [0.38–0.77] | 26/317 (8.2%) | 66/317 (20.8%) | 0.34 [0.21–0.55] |
Grage [22] | 29/100 (29%) | 31/100 (31%) | 0.91 [0.50–1.67] | 2/100 (2%) | 10/100 (10%) | 0.18 [0.04–0.86] |
Blood patch | ||||||
Bourgouin [12] | 15/52 (28.8%) | 30/88 (34.1%) | 0.85 [0.37–1.65] | 4/52 (7.7%) | 8/88 (9.1%) | 0.83 [0.24–2.92] |
Herman [13] | 11/46 (23.9%) | 14/47 (29.8%) | 0.74 [0.30–1.86] | 1/46 (2.2%) | 1/47 (2.1%) | 1.02 [0.06–16.8] |
Lang [14] | 5/50 (10%) | 18/50 (36%) | 0.20 [0.07–0.59] | 0/50 (0%) | 7/50 (14%) | 0.06 [0.00–1.03] |
Malone [15] | 32/123 (26%) | 42/119 (35.3%) | 0.64 [0.37–1.12] | 11/123 (8.9%) | 21/119 (17.6%) | 0.46 [0.21–1.00] |
Clayton [34] | 69/245 (28.2%) | 80/189 (42.3%) | 0.53 [0.36–0.80] | 10/245 (4.1%) | 30/189 (15.9%) | 0.23 [0.11–0.47] |
Graffy [16] | 145/482 (30.1%) | 154/352 (43.8%) | 0.55 [0.42–0.74] | 15/482 (3.1%) | 24/352 (6.8%) | 0.44 [0.23–0.85] |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bourgeais, G., Frampas, E., Liberge, R. et al. Pneumothorax Incidence with Normal Saline Instillation for Sealing the Needle Track After Computed Tomography-Guided Percutaneous Lung Biopsy. Cardiovasc Intervent Radiol 47, 604–612 (2024). https://doi.org/10.1007/s00270-023-03648-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03648-y