Abstract
Purpose
This study aims to evaluate the technical efficacy and local tumor progression-free survival (LTPFS) of a standardized workflow for thermal ablation of colorectal liver metastases (CRLM) consisting of CT during hepatic arteriography (CTHA)-based imaging analysis, stereotactic thermal ablation, and computer-based software assessment of ablation margins.
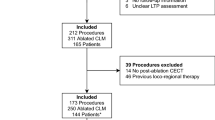
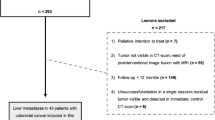
Materials and Methods
This investigator initiated, single-center, single-arm prospective trial will enroll up to 50 patients (≤ 5 CRLM, Measuring ≤ 5 cm). Procedures will be performed in an angio-CT suite under general anesthesia. The primary objective is to estimate LTPFS with a follow-up of up to 2 years and secondary objectives are analysis of the impact of minimal ablative margins on LTPFS, adverse events, contrast media utilization and radiation exposure, overall oncological outcomes, and anesthesia/procedural time. Adverse events (AE) will be recorded by CTCAE (Common Toxicity Criteria for Adverse Events), and Bayesian optimal phase-2 design will be applied for major intraprocedural AE stop boundaries. The institutional CRLM ablation registry will be used as benchmark for comparative analysis with the historical cohort.
Discussion
The STEREOLAB trial will introduce a high-precision and standardized thermal ablation workflow for CRLM consisting of CT during hepatic arteriography imaging, stereotactic guidance, and ablation confirmation.
Trial Registration ClinicalTrials.gov identifier: (NCT05361551).
Graphical Abstract




Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Network NCC NCCN Clinical practice guidelines in oncology (NCCN Guidelines) colon cancer. 2022
Van Cutsem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27(8):1386–422.
Lin YM, Paolucci I, Brock KK, Odisio BC. Image-guided ablation for colorectal liver metastasis: principles, current evidence, and the path forward. Cancers (Basel). 2021;13(16):3926.
Laimer G, Jaschke N, Schullian P, et al. Volumetric assessment of the periablational safety margin after thermal ablation of colorectal liver metastases. Eur Radiol. 2021;31(9):6489–99.
Ruiter SJS, Tinguely P, Paolucci I, et al. 3D quantitative ablation margins for prediction of ablation site recurrence after stereotactic image-guided microwave ablation of colorectal liver metastases: a multicenter study. Front Oncol. 2021;11: 757167.
Kaye EA, Cornelis FH, Petre EN, et al. Volumetric 3D assessment of ablation zones after thermal ablation of colorectal liver metastases to improve prediction of local tumor progression. Eur Radiol. 2019;29(5):2698–705.
Lin Y-M, Paolucci I, OConnor CS, et al. (2022) Ablative Margins of colorectal liver metastases by deformable CT image registration and auto-segmentation. Radiology, In Press
Paolucci I, Lin YM, Jones AK, Brock KK, Odisio BC. Use of contrast media during ct-guided thermal ablation of colorectal liver metastasis for procedure planning is associated with improved immediate outcomes. Cardiovasc Intervent Radiol. 2023. https://doi.org/10.1007/s00270-022-03333-6.
Puijk RS, Nieuwenhuizen S, van den Bemd BAT, et al. Transcatheter CT hepatic arteriography compared with conventional CT fluoroscopy guidance in percutaneous thermal ablation to treat colorectal liver metastases: a single-center comparative analysis of 2 historical cohorts. J Vasc Interv Radiol. 2020;31(11):1772–83.
Tinguely P, Paolucci I, Ruiter SJS, et al. Stereotactic and robotic minimally invasive thermal ablation of malignant liver tumors: a systematic review and meta-analysis. Front Oncol. 2021;11: 713685.
Laimer G, Schullian P, Putzer D, Eberle G, Goldberg SN, Bale R. Can accurate evaluation of the treatment success after radiofrequency ablation of liver tumors be achieved by visual inspection alone? Results of a blinded assessment with 38 interventional oncologists. Int J Hyperthermia. 2020;37(1):1362–7.
Bale R, Widmann G, Stoffner DI. Stereotaxy: breaking the limits of current radiofrequency ablation techniques. Eur J Radiol. 2010;75(1):32–6.
Bale R, Widmann G, Haidu M. Stereotactic radiofrequency ablation. Cardiovasc Intervent Radiol. 2011;34(4):852–6.
Brock KK, Mutic S, McNutt TR, Li H, Kessler ML. Use of image registration and fusion algorithms and techniques in radiotherapy: report of the AAPM radiation therapy committee task group no. 132. Med Phys. 2017;44(7):e43–76.
Anderson BM, Lin EY, Cardenas CE, et al. Automated contouring of contrast and noncontrast computed tomography liver images with fully convolutional networks. Adv Radiat Oncol. 2021;6(1): 100464.
Anderson BM, Rigaud B, Lin YM, et al. Automated segmentation of colorectal liver metastasis and liver ablation on contrast-enhanced CT images. Front Oncol. 2022;12: 886517.
Lin YM, Paolucci I, Anderson BM, et al. Study protocol COVER-ALL: clinical impact of a volumetric image method for confirming tumour coverage with ablation on patients with malignant liver lesions. Cardiovasc Intervent Radiol. 2022. https://doi.org/10.1007/s00270-022-03255-3.
Taiji R, Lin EY, Lin YM, et al. Combined angio-CT systems: a roadmap tool for precision therapy in interventional oncology. Radiol Imaging Cancer. 2021;3(5): e210039.
Puijk RS, Ahmed M, Adam A, et al. Consensus guidelines for the definition of time-to-event end points in image-guided tumor ablation: results of the SIO and DATECAN initiative. Radiology. 2021. https://doi.org/10.1148/radiol.2021203715.
Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria—a 10-year update. J Vasc Interv Radiol. 2014;25(11):1691–705.
Zhou H, Lee JJ, Yuan Y. BOP2: bayesian optimal design for phase II clinical trials with simple and complex endpoints. Stat Med. 2017;36(21):3302–14.
Kron P, Linecker M, Jones RP, Toogood GJ, Clavien PA, Lodge JPA. Ablation or resection for colorectal liver metastases? A systematic review of the literature. Front Oncol. 2019;9:1052.
Puijk RS, Ruarus AH, Vroomen L, van Tilborg A, Scheffer HJ, Nielsen K, et al. Colorectal liver metastases: surgery versus thermal ablation (COLLISION) - a phase III single-blind prospective randomized controlled trial. BMC Cancer. 2018;18(1):821.
Acknowledgements
We would like to thank iSYS Medizintechnik GmbH (Kitzbühel, Austria) for providing the aiming device.
Funding
This is an investigator-initiated trial.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kristy Brock received funding from RaySearch Laboratories AB through a Co-Development and Collaboration Agreement. Kristy Brock and Bruno Odisio have a licensing agreement with RaySearch Laboratories AB. Bruno C. Odisio received research grants from Siemens Healthineers. Kristy Brock and Iwan Paolucci received funding through a generous gift from the Apache Corporation. The other authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for Publication
For this type of study consent for publication is not required.
Informed Consent
Informed consent will be obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Paolucci, I., Albuquerque Marques Silva, J., Lin, YM. et al. Study Protocol STEREOLAB: Stereotactic Liver Ablation Assisted with Intra-Arterial CT Hepatic Arteriography and Ablation Confirmation Software Assessment. Cardiovasc Intervent Radiol 46, 1748–1754 (2023). https://doi.org/10.1007/s00270-023-03524-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03524-9