Abstract
Purpose
To perform a post hoc cost–utility analysis of a randomized controlled clinical trial comparing prostatic artery embolization (PAE) and transurethral resection of the prostate (TURP) in patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia.
Materials and Methods
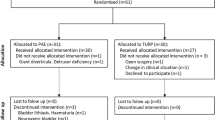
We conducted a cost–utility analysis over a 5-year period to compare PAE versus TURP from a Spanish National Health System perspective. Data were collected from a randomized clinical trial performed at a single institution. Effectiveness was measured as quality-adjusted life years (QALYs), and an incremental cost-effectiveness ratio (ICER) was derived from the cost and QALY values associated with these treatments. Further sensitivity analysis was performed to account for the impact of reintervention on the cost-effectiveness of both procedures.
Results
At the 1-year follow-up, PAE resulted in mean cost per patient of €2904.68 and outcome of 0.975 QALYs per treatment. In comparison, TURP had cost €3846.72 per patient and its outcome was 0.953 QALYs per treatment. At 5 years, the cost for PAE and TURP were €4117.13 and €4297.58, and the mean QALY outcome was 4.572 and 4.487, respectively. Analysis revealed an ICER of €2121.15 saved per QALY gained when comparing PAE to TURP at long-term follow-up. Reintervention rate for PAE and TURP was 12% and 0%, respectively.
Conclusions
Compared to TURP, in short term, PAE could be considered a cost-effective strategy within the Spanish healthcare system for patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia. However, in long term, the superiority is less apparent due to higher reintervention rates.



Similar content being viewed by others
References
Lim KB. Epidemiology of clinical benign prostatic hyperplasia. Asian J Urol. 2017;4(3):148–51.
Gravas S, Cornu JN DM et al. EAU Guidelines: management of non-neurogenic male LUTS [Internet]. 2020. https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/
Insausti I, Sáez de Ocáriz A, Galbete A, Capdevila F, Solchaga S, Giral P, et al. Randomized comparison of prostatic artery embolization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia. J Vasc Interv Radiol. 2020;31(6):882–90.
Abt D, Müllhaupt G, Hechelhammer L, Markart S, Güsewell S, Schmid H-P, et al. Prostatic artery embolisation versus transurethral resection of the prostate for benign prostatic hyperplasia: 2-year outcomes of a randomised, open-label single-centre trial. Eur Urol. 2021;80(1):34–42.
Gao Y, Huang Y, Zhang R, Yang Y, Zhang Q, Hou M, et al. Benign prostatic hyperplasia: prostatic arterial embolization versus transurethral resection of the prostate–a prospective, randomized, and controlled clinical trial. Radiology. 2014;270(3):920–8.
Carnevale FC, Iscaife A, Yoshinaga EM, Moreira AM, Antunes AA, Srougi M. Transurethral resection of the prostate (TURP) versus original and PErFecTED prostate artery embolization (PAE) due to benign prostatic hyperplasia (BPH): preliminary results of a single center, prospective urodynamic-controlled analysis. Cardiovasc Intervent Radiol. 2016;39(1):44–52.
Pisco JM, Bilhim T, Pinheiro LC, Fernandes L, Pereira J, Costa NV, et al. Medium- and long-term outcome of prostate artery embolization for patients with benign prostatic hyperplasia: results in 630 patients. J Vasc Interv Radiol. 2016;27(8):1115–22.
Patel NR, Elterman DS, Thulasidasan N, Altman R, Tai E, Zener R, et al. Initial Canadian experience of prostate artery embolization for symptomatic benign prostatic hyperplasia: midterm outcomes. Can Assoc Radiol J = J l’Assoc Can des Radiol. 2021;72(4):876–82.
Ray AF, Powell J, Speakman MJ, Longford NT, DasGupta R, Bryant T, et al. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int. 2018;122(2):270–82.
Uflacker A, Haskal ZJ, Bilhim T, Patrie J, Huber T, Pisco JM. Meta-analysis of prostatic artery embolization for benign prostatic hyperplasia. J Vasc Interv Radiol. 2016;27(11):1686-1697.e8.
National Institute for Health and Care Excellence. Guidance on Prostate artery embolization for benign prostatic hyperplasia 2018. [Internet]. https://www.nice.org.uk/guidance/ipg611/chapter/1-Recommendations
Foster HE, Barry MJ, Dahm P, Gandhi MC, Kaplan SA, Kohler TS, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. J Urol. 2018;200(3):612–9.
Patel N, Yung N, Vigneswaran G, de Preux L, Maclean D, Harris M, et al. 1-year cost-utility analysis of prostate artery embolization (PAE) versus transurethral resection of the prostate (TURP) in benign prostatic hyperplasia (BPH). BMJ Surg Interv Heal Technol. 2021;3(1):e000071.
Ontario Health (Quality). Prostatic artery embolization for benign prostatic hyperplasia: a health technology assessment. Ont Health Technol Assess Ser. 2021;21(6):1–139.
Rink JS, Froelich MF, McWilliams JP, Gratzke C, Huber T, Gresser E, et al. Prostatic artery embolization for treatment of lower urinary tract symptoms: a Markov model-based cost-effectiveness analysis. J Am Coll Radiol. 2022;19(6):733–43.
Wu X, Zhou A, Heller M, Kohlbrenner R. Prostatic artery embolization versus transurethral resection of the prostate for benign prostatic hyperplasia: a cost-effectiveness analysis. J Vasc Interv Radiol. 2022;33(12):1605–15.
Capdevila F, Insausti I, Galbete A, Sanchez-Iriso E, Montesino M. Prostatic artery embolization versus transurethral resection of the prostate: a post hoc cost analysis of a randomized controlled clinical trial. Cardiovasc Intervent Radiol. 2021;44(11):1771–7.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Value Heal J Int Soc Pharmacoeconom Outcomes Res. 2013;16(2):e1-5.
Napa lLecumberri S, Insausti Gorbea I, de Sáez Ocáriz García A, Solchaga Álvarez S, Cebrián Lostal JL, Monreal Beortegui R, et al. Prostatic artery embolization versus transurethral resection of the prostate in the treatment of benign prostatic hyperplasia: protocol for a non-inferiority clinical trial. Res Rep Urol. 2018;10:17–22.
Vallejo-Torres L, García-Lorenzo B, Serrano-Aguilar P. Estimating a cost-effectiveness threshold for the Spanish NHS. Health Econ. 2018;27(4):746–61.
Kok ET, McDonnell J, Stolk EA, Stoevelaar HJ, Busschbach JJV. The valuation of the international prostate symptom score (IPSS) for use in economic evaluations. Eur Urol. 2002;42(5):491–7.
Bermingham SL, Hodgkinson S, Wright S, Hayter E, Spinks J, Pellowe C. Intermittent self catheterisation with hydrophilic, gel reservoir, and non-coated catheters: a systematic review and cost effectiveness analysis. BMJ. 2013;346:e8639.
Müllhaupt G, Hechelhammer L, Engeler DS, Güsewell S, Betschart P, Zumstein V, et al. In-hospital cost analysis of prostatic artery embolization compared with transurethral resection of the prostate: post hoc analysis of a randomized controlled trial. BJU Int. 2019;123(6):1055–60.
Bagla S, Smirniotopoulos J, Orlando J, Piechowiak R. Cost analysis of prostate artery embolization (PAE) and transurethral resection of the prostate (TURP) in the treatment of benign prostatic hyperplasia. Cardiovasc Intervent Radiol. 2017;40(11):1694–7.
Bilhim T, Costa NV, Torres D, Pinheiro LC, Spaepen E. Long-term outcome of prostatic artery embolization for patients with benign prostatic hyperplasia: single-centre retrospective study in 1072 patients over a 10-year period. Cardiovasc Intervent Radiol. 2022;45(9):1324–36.
Gilfrich C, May M, Fahlenbrach C, Günster C, Jeschke E, Popken G, et al. Surgical reintervention rates after invasive treatment for lower urinary tract symptoms due to benign prostatic syndrome: a comparative study of more than 43,000 patients with long-term followup. J Urol. 2021;205(3):855–63.
Malde S, Umbach R, Wheeler JR, Lytvyn L, Cornu J-N, Gacci M, et al. A systematic review of patients’ values, preferences, and expectations for the diagnosis and treatment of male lower urinary tract symptoms. Eur Urol. 2021;79(6):796–809.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was reviewed and approved by the Institutional Review Board (Comité Ético de Investigación con medicamentos de Navarra).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Appendix 1
See Tables
4,
5 and
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Capdevila, F., Insausti, I., San Miguel, R. et al. Cost–Utility Analysis of Prostatic Artery Embolization for Treatment of Lower Urinary Tract Symptoms. Cardiovasc Intervent Radiol 46, 1025–1035 (2023). https://doi.org/10.1007/s00270-023-03443-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03443-9