Abstract
Purpose
To assess the safety and efficacy of ultrasound-guided percutaneous radiofrequency ablation (RFA) for the treatment of refractory non-nodular hyperthyroidism.
Methods
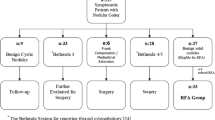
This was a single-center retrospective study in 9 patients with refractory non-nodular hyperthyroidism (2 males, 7 females; median age, range, 36 years, 14–55 years) who underwent RFA between August 2018 and September 2020. The incidence of post-procedural complications, changes in thyroid volume, thyroid function and the use and dosages of anti-thyroid drugs, were compared pre- and post-RFA.
Results
All patients completed the procedure successfully, and no serious complications occurred. Three months after ablation, thyroid volumes were significantly decreased with the mean volumes of the right and left lobes reduced to 45.6% (10.9 ± 2.2 ml/23.9 ± 7.2 ml, p < 0.001) and 50.2% (10.8 ± 7.4 ml/21.5 ± 11.4 ml, p = 0.001) of the volumes within 1 week after ablation. The thyroid function was gradually improved in all patients. At 3 months post-ablation, the levels of FT3 and FT4 were returned to the normal range (FT3, 4.9 ± 1.6 pmol/L vs. 8.7 ± 4.2 pmol/L, p = 0.009; FT4, 13.1 ± 7.2 pmol/L vs. 25.9 ± 12.6 pmol/L, p = 0.038), the TR-Ab level was significantly lower (4.8 ± 3.9 vs. 16.5 ± 16.4 IU/L, p = 0.027), and the TSH level was significantly higher (0.76 ± 0.88 vs. 0.03 ± 0.06, p = 0.031) than that before-ablation. Additionally, three months after RFA, the anti-thyroid medication dosages were reduced to 31.25% compared to baseline (p < 0.01).
Conclusion
Ultrasound-guided RFA in the treatment of refractory non-nodular hyperthyroidism was safe and effective in this small group of patients with limited follow-up. Further studies with larger cohorts and longer follow-up are needed to validate this potential new application of thyroid thermal ablation.





Similar content being viewed by others
References
Smith TJ, Hegedus L. Graves’ disease. N Engl J Med. 2016;375(16):1552–65.
Nystrom HF, Jansson S, Berg G. Incidence rate and clinical features of hyperthyroidism in a long-term iodine sufficient area of Sweden (Gothenburg) 2003–2005. Clin Endocrinol (Oxf). 2013;78(5):768–76.
Ross DS, Burch HB, Cooper DS, et al. 2016 American thyroid association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26(10):1343–421.
Bahn Chair RS, Burch HB, Cooper DS, et al. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American thyroid association and American association of clinical endocrinologists. Thyroid. 2011;21(6):593–646.
Abraham P, Avenell A, McGeoch SC, et al. Antithyroid drug regimen for treating Graves’ hyperthyroidism. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.CD003420.pub4/abstract.
Marcocci C, Watt T, Altea MA, et al. Fatal and non-fatal adverse events of glucocorticoid therapy for Graves’ orbitopathy: a questionnaire survey among members of the European thyroid association. Eur J Endocrinol. 2012;166(2):247–53.
Walasik-Szemplinska D, Kaminski G, Sudol-Szopinska I. Life-threatening complications of high doses of intravenous methylprednisolone for treatment of Graves’ orbitopathy. Thyroid Res. 2019;12:13.
Cepkova J, Horacek J, Vizda J, et al. Radioiodine treatment of Graves’ disease—dose/response analysis. Acta Medica (Hradec Kralove). 2014;57(2):49–55.
Bojic T, Paunovic I, Diklic A, et al. Total thyroidectomy as a method of choice in the treatment of graves ‘disease—analysis of 1432 patients. BMC Surg. 2015;15:39.
Nwatsock JF, Taieb D, Tessonnier L, et al. Radioiodine thyroid ablation in Graves’ hyperthyroidism: merits and pitfalls. World J Nucl Med. 2012;11(1):7–11.
Reid JR, Wheeler SF. Hyperthyroidism: diagnosis and treatment. Am Fam Physician. 2005;72(4):623–30.
Ginsberg J. Diagnosis and management of Graves’ disease. CMAJ. 2003;168(5):575–85.
Chen DY, Schneider PF, Zhang XS, et al. Striving for euthyroidism in radioiodine therapy of Graves’ disease: a 12 year prospective, randomized, open-label blinded end point study. Thyroid. 2011;21(6):647–54.
Berber E, Bernet V, Fahey TJ, et al. American thyroid association statement on remote-access thyroid surgery. Thyroid. 2016;26(3):331–7.
Jeong WK, Baek JH, Rhim H, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008;18(6):1244–50.
Baek JH, Kim YS, Lee D, et al. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol. 2010;194(4):1137–42.
Monchik JM, Donatini G, Iannuccilli J, et al. Radiofrequency ablation and percutaneous ethanol injection treatment for recurrent local and distant well-differentiated thyroid carcinoma. Ann Surg. 2006;244(2):296–304.
Tang X, Cui D, Chi J, et al. Evaluation of the safety and efficacy of radiofrequency ablation for treating benign thyroid nodules. J Cancer. 2017;8(5):754–60.
Kim HJ, Cho SJ, Baek JH, et al. Efficacy and safety of thermal ablation for autonomously functioning thyroid nodules: a systematic review and meta-analysis. Eur Radiol. 2021;31(2):605–15.
Na DG, Lee JH, Jung SL, et al. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012;13(2):117–25.
Chen Y, Liang L, Fang Y, et al. Iodine 131 joint radio frequency ablation treatment for child with hyperthyroidism goiter: one case report. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2017;46(1):89–91.
Zhu JE, Zhang HL, Yu SY, et al. US-guided percutaneous microwave ablation for hyperthyroidism and immediate treatment response evaluation with contrast-enhanced ultrasound. Clin Hemorheol Microcirc. 2021;79(3):435–44.
Xiaoyin T, Ping L, Dan C, et al. Risk assessment and hydrodissection technique for radiofrequency ablation of thyroid benign nodules. J Cancer. 2018;9(17):3058–66.
Sacks D, McClenny TE, Cardella JF, et al. Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14(9 Pt 2):S199-202.
Acknowledgments
Xiaoyin Tang, Bingwei Lu and Min Ding collected the data of the patients, designed the pipeline of the analysis and drafted the manuscript. Bo Zhai and Ping Li conceived and coordinated the overall study and revised the manuscript. All authors read and approved the final manuscript
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiaoyin, T., Bingwei, L., Min, D. et al. Preliminary Results of Utrasound-Guided Percutaneous Radiofrequency Ablation in the Treatment of Refractory Non-nodular Hyperthyroidism. Cardiovasc Intervent Radiol 46, 1015–1022 (2023). https://doi.org/10.1007/s00270-023-03401-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03401-5