Abstract
Purpose
To retrospectively assess the safety and efficacy of coil embolization for catheter-directed true common and proper hepatic artery aneurysm exclusion.
Materials and Methods
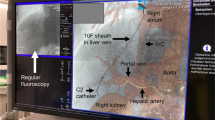
Nine consecutive patients (2005–2021) in two university centers presenting with true common and proper hepatic artery aneurysms (> 2 cm in diameter) were treated with ‘frontdoor-backdoor’ coil embolization. Patients presenting with a hepatic artery pseudoaneurysm, mycotic aneurysm or patients with small (< 2 cm diameter) aneurysms and followed up by imaging were excluded. Technical and clinical success was defined as complete coil-exclusion of the aneurysm on completion angiography and absence of post-embolization adverse events, in particular mass effect or hemorrhage, respectively. Patient characteristics, technical and clinical success, liver function tests and follow-up results were assessed based on the patients’ electronic medical records.
Results
Technical and 30-day clinical success was achieved in all procedures (100%). No major procedural complications were reported. Liver function test values were available in 6/9 patients, showing transient elevation of bilirubin in one patient. No end organ ischemia was reported. The mean clinical follow-up period of the study patients was 72 months (12–168 months). Long-term stable occlusion of the hepatic aneurysms was achieved in 9/9 patients (100%). One patient showed late complication (3 years) with coil migration into a bulbar ulcer, without aneurysm recanalization, however with fatal outcome.
Conclusion
Coil embolization for the endovascular exclusion of true common and proper hepatic artery aneurysms is safe and effective.




Similar content being viewed by others
References
Jesinger RA, Thoreson AA, Lamba R. Abdominal and pelvic aneurysms and pseudoaneurysms: imaging review with clinical, radiologic, and treatment correlation. Radiographics. 2013;33:E71–96.
Rebonato A, Rossi M, Rebonato S, Cagini L, Scialpi M. Giant hepatic artery aneurysm: a fatal evolution. J Emerg Med. 2013;45:e217–9.
Stark J, Eisenberg N, Mafeld S, McGilvray I, Roche-Nagle G, Howe K. Assessment of open surgical and endovascular management of true hepatic artery aneurysms over 20 years highlights increased rupture risk in females. J Vasc Surg. 2022;75:1334–42.
Abbas M, Fowl R, Stone W, Panneton J, Oldenburg W, Bower T, et al. Hepatic artery aneurysm: factors that predict complications. J Vasc Surg. 2003;38:41–5.
Belli AM, Markose G, Morgan R. The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc Interv Radiol. 2012;35:234–43.
Barrionuevo P, Malas MB, Nejim B, Haddad A, Morrow A, Ponce O, et al. A systematic review and meta-analysis of the management of visceral artery aneurysms. J Vasc Surg. 2019;70(5):1694–9.
Chaer R, Abularrage C, Coleman D, Eslami M, Kashyap V, Rockman C, Murad H. The society for vascular surgery clinical practice guidelines on the management of visceral aneurysms. J Vasc Surg. 2020;72:3S-39S.
Venturini M, Marra P, Colombo M, Panzeri M, Gusmini S, Sallemi C, et al. Endovascular repair of 40 visceral artery aneurysms and pseudoaneurysms with the viabahn stent-graft: technical aspects, clinical outcome and mid-term patency. Cardiovasc Interv Radiol. 2018;41:385–97.
Erben Y, De Martino R, Bjarnason H, Duncan A, Kalra M, Oderich G, et al. Operative management of hepatic artery aneurysms. J Vasc Surg. 2015;62:610–5.
Chirica M, Alkofer B, Sauvanet A, Vullierme MP, Levy Y, Belghiti J. Hepatic artery ligation: a simple and safe technique to treat extrahepatic aneurysms of the hepatic artery. Am J Surg. 2008;196:333–8.
Rossi U, Petrocelli F. Hepatic artery aneurysms: endovascular therapeutic options. Ann Hepatobiliary Pancreat Surg. 2021;25:167–70.
Filippiadis DK, Binkert C, Pellerin O, Hoffman RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Interv Radiol. 2017;40:1141–6.
Angle JF, Siddiqi NH, Wallace MJ, Kundu S, Stokes L, Wojak JC, et al. Quality improvement guidelines for percutaneous transcatheter embolization. Society of interventional radiology standards of practice committee. J Vasc Interv Radiol. 2010;21(10):1479–86.
Ramesh Babu CS, Sharma M. Biliary tract anatomy and its relationship with venous drainage. J Clin Exp Hepatol. 2014;4:S18–26.
Charnsangavej C, Chuang VP, Wallace S, Soo CS, Bowers T. Angiographic classification of hepatic arterial collaterals. Radiology. 1982;144:485–94.
Mine T, Murata S, Ueda T, Takeda M, Onozawa S, Yamaguchi H, et al. Contribution of extrahepatic collaterals to liver parenchymal circulation after proper hepatic artery embolization. J Gastroenterol Hepatol. 2014;29:1515–21.
Pedersoli F, Van den Bosch V, Sieben P, Barzakova E, Schulze-Hagen M, Isfort P, et al. Stent graft placement by pseudoaneurysm of the hepatic arteries: efficacy and patency rate in follow-up. Cardiovasc Intervent Radiol. 2022;45:21–8.
Tipaldi M, Krokidis M, Orgera G, Pignatelli M, Ronconi E, Laurino F, Laghi A, Rossi M. Endovascular management of giant visceral artery aneurysms. Sci Rep. 2021;11:700.
Pellerin O, Maleux G, Déan C, Pernot S, Golzarian J, Sapoval M. Microvascular plug: a new embolic material for heaptic arterial skeletonization. Cardiovasc Interv Radiol. 2014;37:1597–601.
Lumsden A, Mattar S, Allen R, Bacha E. Hepatic artery aneurysms: the management of 22 patients. J Surg Res. 1996;60:345–50.
Nomura Y, Gotake Y, Okada T, Yamaguchi M, Sugimoto K, Okita Y. Coil migration to the duodenum 1 year following embolisation of a ruptured giant common hepatic artery aneurysm. EJVES Short Rep. 2018;39:33–6.
Pratap A, Pokala B, Vargas LM, Oleynikov D, Kothari V. Laparoscopic endoscopic combined surgery for removal of migrated coil after embolization of ruptured splenic artery aneurysm. J Surg Case Rep. 2018;2:1–4.
Caragher S, Wang D, Moonsany P, Fagerholz P. Hepatic arterial haemorrhage caused by duodenal ulcer. BMJ Case Rep. 2022;15:e249523.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of the text and they all read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Consent Information
For this type of study, informed consent is not required.
Consent of Publication
For this type of study, consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Van Holsbeeck, A., Dhondt, E., Marrannes, J. et al. Coil Embolization of True, Common and Proper, Hepatic Artery Aneurysms: Technique, Safety and Outcome. Cardiovasc Intervent Radiol 46, 480–487 (2023). https://doi.org/10.1007/s00270-023-03379-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03379-0