Abstract
Purpose
To evaluate the safety and efficacy of prostatic artery embolization (PAE) using polyethylene glycol microspheres (PEGM) in patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia (BPH).
Materials and methods
This multicentric prospective study enrolled 81 patients who underwent PAE with 400 ± 75 µm PEGM (HydroPearl®, Terumo, Japan). Results from baseline and 1-, 3-, 6-, and 12-month follow-ups were assessed for subjective outcomes including International Prostate Symptoms Score (IPSS), Quality of life (QoL), and International Index of Erectile Function, and objective outcomes such as peak urinary flow (Qmax) and post-void residual volume (PVR). The visual analogue scale, satisfaction questionnaire, prostatic volume, and prostatic specific antigen levels were also evaluated. Complications were documented using the modified Clavien–Dindo classification.
Results
Technical success was obtained in all patients. Clinical success was achieved in 78.5% of patients. Before PAE, 54.3% of patients had an indwelling catheter which was removed in 75% of them after procedure. A statistically significant decrease was observed in IPSS and QoL from baseline to 12 months (20.14 vs 5.89; 4.8 vs 0.63, P < .01), respectively. Objective outcomes also showed a statistically significant improvement in Qmax (+ 114.9%; P < .01), achieving a maximum urinary flow of 14.2 mL/sec, and PVR (decrease 58%; P < .05) at 12 months. Minor complications (Clavien–Dindo grades I–II) occurred in 13.6% of patients, without major complications observed.
Conclusion
PAE with PEGM is safe and effective treatment in patients with symptomatic BPH, with a significant improvement in both subjective and objective outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostatic artery embolization (PAE) as a minimally invasive technique has been widely used in the management of lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH) during the last decade. Recent systematic reviews and meta-analyses have demonstrated that PAE is efficacious and safe to improve functional parameters such as the International Prostate Symptom Score (IPSS), quality of life (QOL), peak urinary flow rate (Qmax), and post-void residual volume (PVR) after PAE and can significantly relieve LUTS for 24 months [1,2,3].
As new embolic agents continue to be developed, the use of various embolic particles with different particle sizes in PAE has been reported in clinical practice, including non-spherical polyvinyl alcohol (PVA) particles (Contour), spherical PVA (Bead Block), trisacryl gelatin microspheres (Embosphere), and polyzene-coated hydrogel microspheres (Embozene) [4,5,6,7,8,9,10]. Recently, an embolic agent, polyethylene glycol microspheres (PEGM, HydroPearl) was cleared for use in PAE procedure by the US Food and Drug Administration in January 2020.
HydroPearl microspheres are spherical, biocompatible, and non-resorbable particles, which are engineered for accurate embolization at the target area. Compared to the commonly used Embosphere in PAE, HydroPearl microspheres are less rigid and more compressible with a higher deformation in the vitro study. These characteristics of PEGM are believed to have the potential to induce more distal occlusion within the prostatic vasculature, thus enhancing the therapeutic effect in PAE [11]. Another feature of HydroPearl microspheres is the tight calibration with more than 90% of the particles falling within the size range as indicated on the labels (e.g., 400 ± 75 µm), resulting in tighter luminal packing when delivered into target vessels, and ultimately causing greater tissue necrosis [12]. Although PAE with PEGM has shown promising results in the canine model [13], the safety and efficacy of PEGM used in PAE remain to be proven clinical practice. The aim of this study was to assess the effectiveness and safety of PAE with PEGM for LUTS secondary to BPH.
Materials and Methods
Study Design and Patients
This multi-center prospective cohort study was conducted in accordance with the Declaration of Helsinki [14] and the standards of Good Clinical Practice [15], with approval from the institutional review board. Informed consent was obtained from all patients. The study was conducted by the Interventional Radiology and Urology Departments of the Hospital Universitario de Navarra. This article follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) recommendations for reporting observational studies [16].
Previously, all patients were evaluated by the urologist and were obtained a complete medical history, physical examination including rectal examination, IPSS, QoL, and sexual function using the International Index of Erectile Function (IIEF) questionnaire. Uroflowmetry to measure Qmax, and blood tests for prostate-specific antigen (PSA) were also performed. Imaging studies prior to the procedure included transabdominal ultrasound (US), computed tomography (CT) angiography, and multiparametric magnetic resonance imaging (mpMRI). PVR was measured by transabdominal US. Prostate volume (PV) was assessed by mpMRI. Prostate biopsy was performed whenever a suspicious focal lesion was detected on mpMRI or digital rectal examination, or when the PSA was > 4 mg/mL.
From July 2015 to March 2020, 92 patients with LUTS secondary to BPH were assessed for study eligibility. The inclusion criteria were age > 40 years; PV ≥ 30 cm3; BPH-related LUTS refractory to medical treatment for at least 6 months or intolerance to medical treatment; IPSS > 8 points; QoL ≥ 3 points; Qmax ≤ 12 mL/sec, or urinary retention. The exclusion criteria included the presence of advanced atherosclerosis and tortuosity of the iliac arteries, non-visualization of the prostatic artery or other accessory arteries supplying the prostate on CT angiography, glomerular filtration rate of less than 30 mL/min, acute infection (e.g., prostatitis), the presence of prostate cancer, and previous diagnostic of urethral stenosis, detrusor muscle failure or neurogenic bladder.
From 92 patients evaluated for eligibility, 11 patients were excluded due to the presence of prostate cancer (n = 2), advanced atherosclerosis (n = 7), and neurogenic bladder (n = 2). Finally, 81 patients were enrolled, of whom 79 patients were followed up at least once. Clinical follow-up could not be performed in two patients, one lost to follow-up and a further one deceased by ischemic stroke unrelated to the procedure. Patients were evaluated in the urology consultation at 3, 6, and 12 months to assess BPH medication discontinuation.
Procedure
PAE was performed by 3 interventional radiologists (I.I., A.S.O., S.S.; with 8, 7 and 6 years of experience in this technique, respectively). Embolization was performed under local anesthesia via unilateral femoral approach, most commonly right, and only in a few patients via left radial access. A 5-F hydrophilic Roberts uterine catheter (Cook Medical, Bloomington, Indiana) or Cobra 1 catheter (Terumo, Tokyo, Japan) were used to catheterize both internal iliac arteries. All arteries supplying the prostate were catheterized using a Progreat α 2.0 microcatheter (Terumo), a 0.014-inch Synchro Soft guidewire (Stryker Neuro-vascular, Fremont, California), 0.014–0.016-inch Glidewire GT double-angled or a 90º-angled micro–guide wire (Terumo). When the microcatheter was selectively placed into the prostatic artery, embolization was carried out using 400 ± 75 µm PEGM (HydroPearl®, Terumo, Japan). The microspheres were delivered in 20-mL syringes containing 2 mL of microspheres diluted with 4 mL of NaCl and mixed with 3 mL of contrast (Visipaque 320, GE Healthcare, Little Chalfont, UK) and 1 mL of saline to achieve an adequate particle suspension. The embolization end point was achieved when stasis of contrast with disruption of arterial flow and opacification of prostate gland were present.
Most patients were discharged within 24 h following PAE, and some patients were discharged 4–5 h after the procedure when radial access or femoral closure device was used.
Outcomes
Primary outcomes assessed were QoL, IPSS, and Qmax, and the secondary outcomes were PV, IIEF, PVR, and PSA. All outcomes were measured before the procedure, and at 1-, 3-, 6-, and 12-month follow-ups, except in Qmax and PVR which were measured before the procedure, and at 3, 6, and 12 months.
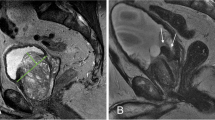
In addition, the presence of prostate infarction as well as the volume of infarction was assessed by mpMRI at one month after PAE. The volume of ischemia tissue was calculated on contrast-enhanced T1-weighted images using Philips IntelliSpace Portal 3D volume software (Amsterdam, the Netherlands).
Technical success was defined as embolization of at least one prostatic artery. Clinical success included the presence of the following [17]: a decrease of at least 25% in IPSS from baseline with a final IPSS score ≤ 18 points; a decrease of at least 1 point in QoL score from baseline with a final score of ≤ 3 points; removal of the indwelling catheter with subsequent spontaneous micturition in patients with a urinary catheter before PAE.
Safety of PAE was assessed by the number and severity of adverse events, which were graded according to modified Clavien–Dindo classification system [18]. Pain and satisfaction with the procedure were measured at 24 h following PAE by phone call, as described in previous studies [19]. Other complementary parameters were assessed such as arterial access site, type of anesthesia, fluoroscopy time, radiation dose, length of post-procedure hospital stay, and interruption of medical therapy.
Statistical Analysis
Descriptive analysis was performed and expressed by mean and standard deviation for quantitative variables and by frequency and percentage for categorical variables. The statistical differences at different follow-up time-points were analyzed using student t-test for paired data, showing mean difference from baseline with 95% confidence interval and percentage change. All comparisons were two-sided with a significance level of 0.05.
Results
Baseline Characteristics
The baseline characteristics of the included patients are shown in Table 1. The mean age was 73.87 ± 10.21 years (range, 54–92 years) with IPSS 20.14 ± 4.33 points, PV 96.24 ± 47.1 ml, and Qmax 6.99 ± 2.8 mL/s. The most frequent symptom in urology consultation was urine retention. Prior to PAE, 92.6% (75/81) of the patients were on medical treatment for LUTS secondary to BPH.
Perioperative and Postoperative Data
Perioperative and postoperative data are shown in Table 2. Technical success was obtained in 100% (81/81) of the patients. Bilateral PAE was performed in 69 (85.2%) patients, whereas unilateral PAE was due to the impossibility of catheterization of the prostate artery (n = 3), the presence of anastomoses to the rectum or penis not suitable for embolization (n = 4), and sub-occlusive arterial atheromatous disease (n = 5).
The mean procedure time was 135.13 ± 76.24 min, and the mean fluoroscopy time was 41.82 ± 26.57 min. The mean dose radiation was 203.2 ± 38.6 Gy/cm2. The mean amount of microspheres injected into each prostate artery was 2.65 ml (range, 1–6 ml).
Regarding hospital stay, 69 patients (85.2%) were admitted for 24 h after PAE, and 12 patients (14.8%) were treated on an outpatient basis. All patients were discharged without immediate complications. The mean PSA at 24 h was 77.68 ng/dL (range 0.01–2000 ng/dL). Furthermore, pain measured by visual analogue scale (VAS) was 1.24 ± 0.44 points, and the mean satisfaction measured on a scale of 0 (very dissatisfied) to 100 (very satisfied) was of 81.4 ± 10.2 points at 24 h after PAE. The percentage of patients who stopped taking medication for LUTS secondary to BPH after PAE was 91.3% at 3 months, 95% at 6 months, and 97.5% at 12 months. Only 2.5% of the patients continued with medical treatment at 12 months.
Primary and Secondary Outcomes
Primary and secondary outcome data are shown in Table 3 and Fig. 1. Statistically significant improvements at 12 months of follow-up compared with baseline data were observed in IPSS (reduction of 63.3%, P < 0.01), in QoL (reduction of 85%, P < 0.01), in Qmax (increase of 114.9%, P < 0.01), and in PVR (reduction of 32.3%, P < 0.05).
At 12 months after PAE, PSA decreased 58.6% (6.08 ± 18.91 ng/dL), and IIEF was 4.13 ± 8.80 points (increase of 87%, P = 0.0347), but both differences were statistically not significant.
PV measured on MRI showed a statistically significant decrease of 32.3% (P < 0.05) from baseline to 12 months post-PAE. Prostatic infarction was present in 64.4% patients at one month after PAE, with a mean volume of 9.4 ± 1.5 cm3 (range 0.3–60 cm3).
Clinical Success
Clinical success was obtained in 78.5% of the patients; of whom 45.7% were non-catheterized patients and 54.3% had urinary catheter. Among the non-catheterized patients, there were 6.25% clinical failures in the first month, 0% in the third month, 12.9% in the sixth month, and 8.4% in the twelfth month. Clinical success was higher in patients with bilateral PAE (81% vs 67%; P = 0.287).
In patients with urinary retention, removal of the catheter with subsequent spontaneous micturition was achieved in 75% of them (33/44) at first three months after PAE (76% within the first month, and 24% from first to third month). Patients with bilateral PAE achieved higher percentage of catheter removal (76.92 vs 50%; P = 0.13). Before PAE, the mean time from urinary catheter insertion was 8.5 months (254.31 ± 375.45 days). After PAE, the mean time to removal of the urinary catheter was 25.8 days (range 1–90 days).
Prior to PAE, 59.46% (22/37) of patients had severe LUTS, and 40.54% (15/37) had moderate LUTS. At 12 months after PAE, 77.78% (21/27) of the patients had mild LUTS, 22.22% (6/27) had moderate LUTS, and there were no patients with severe LUTS (Table 4).
Safety
After PAE, 11 patients (13.6%) had 13 minor complications. The distribution of complications according to the modified Clavien–Dindo classification was 30.8% (4/13) grade I, 69.2% (9/13) grade II, with no grade III or IV complications. The complications were urinary tract infection (3/11 patients, 27.3%), urinary retention (3/11 patients, 27.3%), post-embolization syndrome (3/11 patients, 27.3%), erectile dysfunction (1/11 patient, 9%), and femoral artery dissection (1/11 patient, 9%). The patients with urinary retention after PAE were treated by TURP, while patients with urinary tract infection required medical treatment; the remaining adverse events were spontaneously resolved, and all patients recovered without sequelae.
Discussion
This study has shown statistically significant improvements in subjective (QoL, IPSS, IIEF, pain and satisfaction scores) and objective (Qmax, PVR, PV, prostatic infarct) outcomes in patients treated with PAE using PEGM, achieving a clinical success of 78.5%. These results are comparable to those previously published with PVA [5, 6] and other types of microspheres [4, 19,20,21,22,23,24], where PAE improved BPH-related LUTS in patients.
Most of the improvements in objective and subjective parameters were observed between the first and third month after PAE, except for PSA. After 3 months, a plateau or slight improvement was observed in all outcomes (Fig. 1). This fact confirms the fast effect of PAE on relief of LUTS described in patients [7, 25]. In addition, PSA increased at one month after PAE, and subsequently decreased up to 66% at 3 months of follow-up compared with baseline data. Early rise in PSA may owe to the initial inflammatory effect associated to prostatic ischemia induced by PAE [26].
The size of PEGM used in the present study was 400 ± 75 µm. Compared to other commonly used microspheres in PAE, such as Embosphere (300–500 µm) and Bead Block (300–500 µm), the tight calibration has a technical advantage of the tighter luminal packing of microsphere once delivered into the target vessels, resulting in greater tissue necrosis [12]. In a report of 186 patients with moderate to severe LUTS who underwent PAE with Bead Block (300–500 µm) [4], the mean IPSS decreased by 12.1 at 1-year follow-up, which is similar to the corresponding data of 12.81 in the present study. However, in the same time period, our data of the mean difference from baseline was superior in QoL score (− 4.09 vs − 1.83), Qmax (8.03 vs 2.33 mL/sec), and PV (− 34.87 vs − 15.2 cm3). By contrast, another clinical trial using Embosphere (300–500 µm) in PAE in 88 consecutive patients showed the 1-year outcomes with the mean difference from baseline by − 13.58, -2.9, 9.61 mL/sec, and − 58.11 cm3, respectively, in IPSS, QoL score, Qmax, and PV [21]. In addition, Embozene is also a tightly calibrated spherical embolic agent. In a report of preliminary results of PAE in 20 patients [27], clinical success at 6 months was obtained in 76.5%, whereas our data using the same criteria for clinical success showed 87.1% at 6 months after PAE. Nevertheless, to further address and compare the clinical efficacy in PAE among various embolic agents, randomized controlled trials and meta-analyses are needed in the future.
Multiple studies have shown the safe, effective, and durable effect of PAE in patients with urinary retention [28,29,30,31,32,33]. In those studies, between 70 and 91% of patients with urinary retention were able to void spontaneously after PAE. Carnevale et al. reported a 91% catheter removal rate in 11 men after PAE, with a mean catheter removal time of 12 days [29]. In our study, 54.3% of the patients treated with PAE had urinary retention, with successful removal of the urinary catheter in 75% of them, and a mean time of 25.8 days. This longer time for catheter removal in our study may be explained by the longer period of catheterization prior to PAE (148.5 days).
PAE is a minimally invasive technique showing a lower adverse event profile, less pain, higher satisfaction, and faster recovery time when compared to surgery [20, 34, 35]. No major adverse events were observed in the study, while minor adverse events were reported in 13.6% of patients. The most frequent complications were acute urinary retention, urinary tract infection, and post-embolization syndrome, including dysuria and local pain. A single patient of sexual dysfunction was reported, and there was no incidence of post-procedure retrograde ejaculation or ejaculatory disorders. Our results are comparable with the low rate of complications in the sexual sphere described in other studies [34, 36, 37]. According to published evidence and to our study results, patients with a contraindication to surgery or those who want to preserve ejaculatory and sexual function may benefit from PAE, since it improves urinary symptoms without deteriorating sexual activity due to no urethral manipulation [38].
This observational study had several limitations. Despite being a prospective multicenter study, randomization and comparison with other treatments were not performed. On the other hand, the number of patients was relatively small with a significant lost to follow-up, possibly because of the advanced age of the patients. Furthermore, the IIEF could only be analyzed in a few patients who were sexually active. Another limitation was the medium-term follow-up period limited to 12 months.
In conclusion, PAE with PEGM is a safe and effective technique in the treatment of LUTS secondary to BPH, allowing success in removing the urinary catheter with subsequent spontaneous micturition in a high percentage of patients treated. Comparative studies are needed to assess the potential benefits of this specific embolic agent over the previously reported ones.
Change history
24 January 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00270-023-03371-8
References
Uflacker A, Haskal ZJ, Bilhim T, Patrie J, Huber T, Pisco JM. Meta-analysis of prostatic artery embolization for benign prostatic hyperplasia. J Vasc Interv Radiol. 2016;27(11):1686-1697.e8.
Knight GM, Talwar A, Salem R, Mouli S. Systematic review and meta-analysis comparing prostatic artery embolization to gold-standard transurethral resection of the prostate for benign prostatic hyperplasia. Cardiovasc Intervent Radiol. 2021;44(2):183–93.
Xiang P, Guan D, Du Z, Hao Y, Yan W, Wang Y, et al. Efficacy and safety of prostatic artery embolization for benign prostatic hyperplasia: a systematic review and meta-analysis of randomized controlled trials. Eur Radiol. 2021;31(7):4929–46.
Bilhim T, Pisco J, Pereira JA, Costa NV, Fernandes L, Pinheiro LC, et al. Predictors of clinical outcome after prostate artery embolization with spherical and nonspherical polyvinyl alcohol particles in patients with benign prostatic hyperplasia. Radiology. 2016;281(1):289–300.
Bilhim T, Pisco J, Campos Pinheiro L, Rio Tinto H, Fernandes L, Pereira JA, et al. Does polyvinyl alcohol particle size change the outcome of prostatic arterial embolization for benign prostatic hyperplasia? Results from a single-center randomized prospective study. J Vasc Interv Radiol. 2013;24(11):1595–602.
Wang MQ, Zhang JL, Xin HN, Yuan K, Yan J, Wang Y, et al. Comparison of clinical outcomes of prostatic artery embolization with 50-μm Plus 100-μm polyvinyl alcohol (PVA) particles versus 100-μm PVA particles alone: a prospective randomized trial. J Vasc Interv Radiol. 2018;29(12):1694–702.
Torres D, Costa NV, Pisco J, Pinheiro LC, Oliveira AG, Bilhim T. Prostatic artery embolization for benign prostatic hyperplasia: prospective randomized trial of 100–300 μm versus 300–500 μm versus 100- to 300-μm + 300- to 500-μm embospheres. J Vasc Interv Radiol. 2019;30(5):638–44.
Bilhim T. Endovascular resection of the prostate: how much is enough for prostate artery embolization? J Vasc Interv Radiol. 2019;30(2):225–7.
Isaacson AJ, Raynor MC, Yu H, Burke CT. Prostatic artery embolization using embosphere microspheres for prostates measuring 80–150 cm(3): early results from a US trial. J Vasc Interv Radiol. 2016;27(5):709–14.
Carnevale FC, Moreira AM, Antunes AA. The “PErFecTED technique”: proximal embolization first, then embolize distal for benign prostatic hyperplasia. Cardiovasc Intervent Radiol. 2014;37(6):1602–5.
Bilhim T. Prostatic artery embolization for benign prostatic hyperplasia: a 10-year update. Endovasc Today. 2020;19:40–4.
Patetta MA, Isaacson AJ, Stewart JK. Initial experience with hydropearl microspheres for uterine artery embolization for the treatment of symptomatic uterine fibroids. CVIR Endovasc. 2021;4(1):1–7.
Lucas Cava V, Sánchez Margallo FM, Báez Díaz C, Dávila Gómez L, Lima Rodríguez JR, Sun F. Prostatic artery embolization with polyethylene glycol microspheres: evaluation in a canine spontaneous benign prostatic hyperplasia model. CVIR Endovasc. 2020;3(1):1–8.
World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373–4.
Dixon JRJ. The international conference harmonization good clinical practice guideline. Qual Assur. 1998;6(2):65–74.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–4.
Cornelis FH, Bilhim T, Hacking N, Sapoval M, Tapping CR, Carnevale FC. CIRSE standards of practice on prostatic artery embolisation. Cardiovasc Intervent Radiol. 2020;43(2):176–85.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Insausti I, Sáez de OcárizGalbete AA, Capdevila F, Solchaga S, Giral P, et al. Randomized comparison of prostatic artery embolization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia. J Vasc Interv Radiol. 2020;31(6):882–90.
Abt D, Hechelhammer L, Müllhaupt G, Markart S, Güsewell S, Kessler TM, et al. Comparison of prostatic artery embolisation (PAE) versus transurethral resection of the prostate (TURP) for benign prostatic hyperplasia: Randomised, open label, non-inferiority trial. BMJ. 2018. https://doi.org/10.1136/bmj.k2338.
Kurbatov D, Russo GI, Lepetukhin A, Dubsky S, Sitkin I, Morgia G, et al. Prostatic artery embolization for prostate volume greater than 80 cm3: results from a single-center prospective study. Urology. 2014;84(2):400–4.
Bagla S, Martin CP, van Breda A, Sheridan MJ, Sterling KM, Papadouris D, et al. Early results from a United States trial of prostatic artery embolization in the treatment of benign prostatic hyperplasia. J Vasc Interv Radiol. 2014;25(1):47–52.
Gonçalves OM, Carnevale FC, Moreira AM, Antunes AA, Rodrigues VC, Srougi M. Comparative study using 100–300 versus 300–500 μm microspheres for symptomatic patients due to enlarged-BPH prostates. Cardiovasc Intervent Radiol. 2016;39(10):1372–8.
Ayyagari R, Powell T, Staib L, Chapiro J, Raja A, Bhatia S, et al. Prostatic artery embolization using 100–300-μm trisacryl gelatin microspheres to treat lower urinary tract symptoms attributable to benign prostatic hyperplasia: a single-center outcomes analysis with medium-term follow-up. J Vasc Interv Radiol. 2020;31(1):99–107.
Pisco JM, Rio Tinto H, Campos Pinheiro L, Bilhim T, Duarte M, Fernandes L, et al. Embolisation of prostatic arteries as treatment of moderate to severe lower urinary symptoms (LUTS) secondary to benign hyperplasia: results of short- and mid-term follow-up. Eur Radiol. 2013;23(9):2561–72.
Sun F, Crisóstomo V, Báez-Díaz C, Sánchez FM. Prostatic artery embolization (PAE) for symptomatic benign prostatic hyperplasia (BPH): Part 2, insights into the technical rationale. Cardiovasc Intervent Radiol. 2016;39(2):161–9.
Costa NV, Pisco JM, Bilhim T, Pinheiro L, Fernandes L, Pereira JA, et al. The safety and efficacy of prostatic arteries embolization with polyzene-coated microspheres (Embozene) for benign prostatic hyperplasia—preliminary results. J Vasc Interv Radiol. 2015;26(2):S155.
Ayyagari R, Powell T, Staib L, Chapiro J, Perez-Lozada J-C, Bhatia S, et al. Prostatic artery embolization in nonindex benign prostatic hyperplasia patients: single-center outcomes for urinary retention and gross prostatic hematuria. Urology. 2020;136:212–7.
Carnevale FC, Da Motta-Leal-Filho JM, Antunes AA, Baroni RH, Marcelino ASZ, Cerri LMO, et al. Quality of life and clinical symptom improvement support prostatic artery embolization for patients with acute urinary retention caused by benign prostatic hyperplasia. J Vasc Interv Radiol. 2013;24(4):535–42.
Rampoldi A, Barbosa F, Secco S, Migliorisi C, Galfano A, Prestini G, et al. Prostatic artery embolization as an alternative to indwelling bladder catheterization to manage benign prostatic hyperplasia in poor surgical candidates. Cardiovasc Intervent Radiol. 2017;40(4):530–6.
Bhatia S, Sinha VK, Kava BR, Gomez C, Harward S, Punnen S, et al. Efficacy of prostatic artery embolization for catheter-dependent patients with large prostate sizes and high comorbidity scores. J Vasc Interv Radiol. 2018;29(1):78-84.e1.
Kenny AG, Pellerin O, Amouyal G, Desgranchamps F, Méria P, De Gouvello A, et al. Prostate artery embolization in patients with acute urinary retention. Am J Med. 2019;132(11):e786–90.
Antunes AA, Carnevale FC, Da Motta Leal Filho JM, Yoshinaga EM, Cerri LMO, Baroni RH, et al. Clinical, laboratorial, and urodynamic findings of prostatic artery embolization for the treatment of urinary retention related to benign prostatic hyperplasia. a prospective single-center pilot study. Cardiovasc Intervent Radiol. 2013;36(4):978–86.
Carnevale FC, Iscaife A, Yoshinaga EM, Moreira AM, Antunes AA, Srougi M. Transurethral resection of the prostate (TURP) versus original and PErFecTED prostate artery embolization (PAE) due to benign prostatic hyperplasia (BPH): preliminary results of a single center, prospective. Urodyn-Controlled Anal Cardiovasc Intervent Radiol. 2016;39(1):44–52.
Hacking N, Vigneswaran G, Maclean D, Modi S, Dyer J, Harris M, et al. Technical and imaging outcomes from the UK registry of prostate artery embolization (UK-ROPE) study: focusing on predictors of clinical success. Cardiovasc Intervent Radiol. 2019;42(5):666–76.
Pisco JM, Bilhim T, Pinheiro LC, Fernandes L, Pereira J, Costa NV, et al. Medium- and long-term outcome of prostate artery embolization for patients with benign prostatic hyperplasia: results in 630 patients. J Vasc Interv Radiol. 2016;27(8):1115–22.
Pisco JM, Bilhim T, Costa NV, Torres D, Pisco J, Pinheiro LC, et al. Randomised clinical trial of prostatic artery embolisation versus a sham procedure for benign prostatic hyperplasia. Eur Urol. 2020;77(3):354–62.
Marzano L, Thiounn N, Pereira H, Pellerin O, Dariane C, Del Giudice C, et al. Prostatic artery embolization allows to maintain full sexual activity in patients suffering from bothersome lower urinary tracts symptoms related to benign prostatic hyperplasia. Cardiovasc Intervent Radiol. 2020;43(8):1202–7.
Funding
Terumo Europe NV has supported this project. The grant funded the study (including open access) and was managed by Navarrabiomed (Pamplona, Spain). The authors were responsible for the design, running and the analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants involved in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Please note correction of incorrect “Funding” in the original paper which says that “This study was not supported by any funding”. The “Funding” section should say “Terumo Europe NV has supported this project. The grant funded the study (including open access) and was managed by Navarrabiomed (Pamplona, Spain). The authors were responsible for the design, running and the analysis of the data”.
This article was updated to correct the tagging of José Ignacio Bilbao Jaureguízar name.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Insausti, I., Galbete, A., Lucas-Cava, V. et al. Prostatic Artery Embolization (PAE) Using Polyethylene Glycol Microspheres: Safety and Efficacy in 81 Patients. Cardiovasc Intervent Radiol 45, 1339–1348 (2022). https://doi.org/10.1007/s00270-022-03165-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03165-4