Abstract
Introduction
Optisphere (Teleflex, Wayne, PA, USA, currently distributed by Medtronic, Minneapolis, MN, USA) is a new, resorbable, calibrated spherical embolic agent. We aimed to evaluate its clinical safety and effectiveness for fibroid embolization through a prospective case series.
Method
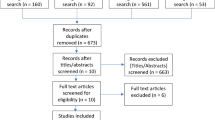
This prospective case series studied patients treated with fibroid embolization using Optisphere between July 2017 and June 2018. The primary outcomes were device-related adverse event assessments and MRI-determined percentage infarct of the dominant fibroid (DF %) and infarct of all fibroids (AF %) at 3 months post-embolization. Secondary outcomes included symptom improvement with the validated Uterine Fibroid Symptom Score and Quality of Life questionnaire (UFS-SS and UFS-QOL) at 3 months and 12 months post-embolization. Statistical analysis was through the Wilcoxon signed-rank test for nonparametric paired data.
Results
Twenty-three consecutive patients were treated with Optisphere (median age 44.0, uterine volume 484.0 ml, dominant fibroid volume 167.0 ml). The complete dominant fibroid infarction (DF %) rate was 91.3% (21/23 patients), and the complete all fibroid infarction rate (AF %) was 82.6% (19/23). No adverse device-related safety events were encountered. Significant improvement was demonstrated in 3-month UFS-SS (56 vs 19, p < 0.0001), UFS-QOL (40 vs 88, p = 0.0008), uterine volume (484 ml vs 246 ml, p < 0.0001) and dominant fibroid volume (167 vs 64 ml, p < 0.0001). Symptomatic improvement continued to 12 months (UFS-SS 56 vs 11, p = 0.0008, UFS-QOL 40 vs 98.7, p = 0.0008).
Conclusion
Optisphere is an effective embolic agent for fibroid embolization with good symptomatic response and percentage fibroid infarct.



Similar content being viewed by others
References
Ravina JH, Herbreteau D, Ciraru-Vigneron N, Bouret JM, Houdart E, Aymard A, et al. Arterial embolisation to treat uterine myomata. Lancet. 1995;346:671–2.
Ravina JH, Merland JJ, Herbreteau D, Houdart E, Bouret JM, Madelenat P. Preoperative embolization of uterine fibroma. Preliminary results (10 cases). Presse Med. 1994;23:1540.
Volkers NA, Hehenkamp WJK, Birnie E, Ankum WM, Reekers JA. Uterine artery embolization versus hysterectomy in the treatment of symptomatic uterine fibroids: 2 years’ outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2007;196:519.e1–11.
Critchley H, Horne A. Faculty of 1000 evaluation for Symptomatic uterine fibroids: treatment with uterine artery embolization or hysterectomy–results from the randomized clinical Embolisation versus Hysterectomy (EMMY) Trial. F1000—Post-publication peer review of the biomedical literature. 2008. https://doi.org/10.3410/f.1104365.560383.
Pelage J-P, Guaou NG, Jha RC, Ascher SM, Spies JB. Uterine fibroid tumors: long-term MR imaging outcome after embolization. Radiology. 2004;230:803–9.
Katsumori T, Kasahara T, Kin Y, Nozaki T. Infarction of uterine fibroids after embolization: relationship between postprocedural enhanced MRI findings and long-term clinical outcomes. Cardiovasc Intervent Radiol. 2008;31:66–72.
Worthington-Kirsch RL, Hughes LA. Uterine artery embolization—vascular anatomic considerations and procedure techniques. Uterine Fibroids. 2003. pp. 83–90. https://doi.org/10.1017/cbo9780511550218.013.
Das R, Champaneria R, Daniels JP, Belli A-M. Comparison of embolic agents used in uterine artery embolisation: a systematic review and meta-analysis. Cardiovasc Intervent Radiol. 2014;37:1179–90.
Mari G, Hanif F. Fetal doppler: umbilical artery, middle cerebral artery, and venous system. Semin Perinatol. 2008;32:253–7.
Eid ME-S, Eid ME-S, Taye AM. Impaired uterine perfusion in infertile women with repeated IVF-implantation failure as detected by uterine artery color Doppler study. Fertility and Sterility. 2009. p. S118. https://doi.org/10.1016/j.fertnstert.2009.07.1126.
Laurent A, Pelage J-P, Wassef M, Martal J. Fertility after bilateral uterine artery embolization in a sheep model. Fertility and Sterility. 2008. pp. 1371–1383. https://doi.org/10.1016/j.fertnstert.2007.03.058.
Laurent A, Moine L. The new biomaterials of embolization: the shift to degradable. Med Sci. 2017;33:25–31.
Medtronic Minneapolis U. Instructions for Use-Optisphere Embospheres. 2018 Oct. Available: http://manuals.medtronic.com/content/dam/emanuals/spinal/102339_rD_IFUOptiSphere_Embolization_Spheres_Intl_LLC.pdf.
Vaidya S, Tozer K, Chen J. An overview of embolic agents. Semin Intervent Radiol. 2008;25:204–15. https://doi.org/10.1055/s-0028-1085930.
Yadavali R, Ananthakrishnan G, Sim M, Monaghan K, McNaught G, Hamoodi I, et al. Randomised trial of two embolic agents for uterine artery embolisation for fibroids: Gelfoam versus Embospheres (RAGE trial). CVIR Endovascular. 2019. https://doi.org/10.1186/s42155-018-0044-y.
Norman R. Assessing ovarian reserve—AMH and its opportunities and disadvantages. Pathology. 2017;49:S15–6.
Spies JB, Allison S, Flick P, Cramp M, Bruno J, Jha RC, et al. Spherical polyvinyl alcohol versus tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: results of a limited randomized comparative study. J Vasc Interv Radiol. 2005;16:1431–7.
Siskin GP, Beck A, Schuster M, Mandato K, Englander M, Herr A. Leiomyoma infarction after uterine artery embolization: a prospective randomized study comparing tris-acryl gelatin microspheres versus polyvinyl alcohol microspheres. J Vasc Interv Radiol. 2008;19:58–65.
Spies JB, Allison S, Flick P, McCullough M, Sterbis K, Cramp M, et al. Polyvinyl alcohol particles and tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: results of a randomized comparative study. J Vasc Interv Radiol. 2004;15:793–800.
Katsumori T, Kasahara T, Akazawa K. Long-term outcomes of uterine artery embolization using gelatin sponge particles alone for symptomatic fibroids. AJR Am J Roentgenol. 2006;186:848–54.
Morimoto K, Chono S, Kosai T, Seki T, Tabata Y. Design of Cationic Microspheres Based on Aminated Gelatin for Controlled Release of Peptide and Protein Drugs. Drug Delivery. 2008. pp. 113–117. https://doi.org/10.1080/10717540801905124.
Tamilvanan S. Progress in the design of biodegradable polymer-based microspheres for parenteral controlled delivery of therapeutic peptide/protein. Pharmaceutical Manufacturing Handbook. pp. 393–441. https://doi.org/10.1002/9780470259818.ch12.
Bengtsson J, Cwikiel W, Sundgren PC, Karlstam E, Gavier-Widén D, Keussen I. The effects of uterine artery embolization with a new degradable microsphere in an experimental study. Acta Radiol. 2017;58:1334–41. https://doi.org/10.1177/0284185117694510.
Iezzi R, Pompili M, Rinninella E, Annicchiarico E, Garcovich M, Cerrito L, et al. TACE with degradable starch microspheres (DSM–TACE) as second-line treatment in HCC patients dismissing or ineligible for sorafenib. Eur Radiol. 2019;29:1285–92.
Cheung R, Ying Y, Rauth A, Marcon N, Yuwu X. Biodegradable dextran-based microspheres for delivery of anticancer drug mitomycin C. Biomaterials. 2005;26:5375–85. https://doi.org/10.1016/j.biomaterials.2005.01.050.
Forster REJ, Thürmer F, Wallrapp C, Lloyd AW, Macfarlane W, Phillips GJ, et al. Characterisation of physico-mechanical properties and degradation potential of calcium alginate beads for use in embolisation. J Mater Sci Mater Med. 2010;21:2243–51. https://doi.org/10.1007/s10856-010-4080-y.
Owen RJ, Nation PN, Polakowski R, Biliske JA, Tiege PB, Griffith IJ. A preclinical study of the safety and efficacy of Occlusin™ 500 artificial embolization device in sheep. Cardiovasc Intervent Radiol. 2012;35:636–44.
Funding
This study was fully funded by a grant from Teleflex (Wayne, Pennsylvania, USA) who produce Optisphere. Representatives from the company were involved in reviewing and critiquing the study design, report and publication draft. They also conducted a quality audit of the study data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Nigel Hacking has received honoraria from Boston Scientific and Celonova as a speaker and has been on Advisory boards for BTG. Tim Bryant has proctored for Boston Scientific and Terumo and has received speaker honorariums from Boston Scientific. Sachin Modi has received a speaker honorarium from Boston Scientific. The other authors declare no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This study was approved by the institutional review board (IRB), regional ethics committee and national regulatory body.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hacking, N., Maclean, D., Vigneswaran, G. et al. Uterine Fibroid Embolization (UFE) with Optisphere: A Prospective Study of a New, Spherical, Resorbable Embolic Agent. Cardiovasc Intervent Radiol 43, 897–903 (2020). https://doi.org/10.1007/s00270-020-02460-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02460-2