Abstract
Objective
To develop and assess the accuracy of an augmented reality (AR) needle guidance smartphone application.
Methods
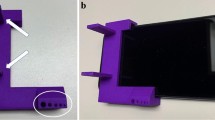
A needle guidance AR smartphone application was developed using Unity and Vuforia SDK platforms, enabling real-time displays of planned and actual needle trajectories. To assess the application’s accuracy in a phantom, eleven operators (including interventional radiologists, non-interventional radiology physicians, and non-physicians) performed single-pass needle insertions using AR guidance (n = 8) and CT-guided freehand (n = 8). Placement errors were measured on post-placement CT scans. Two interventional radiologists then used AR guidance (n = 3) and CT-guided freehand (n = 3) to navigate needles to within 5 mm of targets with intermediate CT scans permitted to mimic clinical use. The total time and number of intermediate CT scans required for successful navigation were recorded.
Results
In the first experiment, the average operator insertion error for AR-guided needles was 78% less than that for CT-guided freehand (2.69 ± 2.61 mm vs. 12.51 ± 8.39 mm, respectively, p < 0.001). In the task-based experiment, interventional radiologists achieved successful needle insertions on each first attempt when using AR guidance, thereby eliminating the need for intraoperative CT scans. This contrasted with 2 ± 0.9 intermediate CT scans when using CT-guided freehand. Additionally, average procedural times were reduced from 13.1 ± 6.6 min with CT-guided freehand to 4.5 ± 1.3 min with AR guidance, reflecting a 66% reduction.
Conclusions
All operators exhibited superior needle insertion accuracy when using the smartphone-based AR guidance application compared to CT-guided freehand. This AR platform can potentially facilitate percutaneous biopsies and ablations by improving needle insertion accuracy, expediting procedural times, and reducing radiation exposures.




Similar content being viewed by others
References
Appelbaum L, Sosna J, Nissenbaum Y, Benshtein A, Goldberg SN. Electromagnetic navigation system for CT-guided biopsy of small lesions. AJR Am J Roentgenol. 2011;196(5):1194–200. https://doi.org/10.2214/ajr.10.5151.
Putzer D, Arco D, Schamberger B, Schanda F, Mahlknecht J, Widmann G, et al. Comparison of two electromagnetic navigation systems for CT-guided punctures: a phantom study. RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2016;188(5):470–8. https://doi.org/10.1055/s-0042-103691.
Kloeppel R, Weisse T, Deckert F, Wilke W, Pecher S. CT-guided intervention using a patient laser marker system. Eur Radiol. 2000;10(6):1010–4. https://doi.org/10.1007/s003300051054.
Rajagopal M, Venkatesan AM. Image fusion and navigation platforms for percutaneous image-guided interventions. Abdom Radiol. 2016;41(4):620–8. https://doi.org/10.1007/s00261-016-0645-7.
Xu S, Krishnasamy V, Levy E, Li M, Tse ZTH, Wood BJ. Smartphone-guided needle angle selection during CT-guided procedures. AJR Am J Roentgenol. 2018;210(1):207–13. https://doi.org/10.2214/ajr.17.18498.
Hiraki T, Matsuno T, Kamegawa T, Komaki T, Sakurai J, Matsuura R, et al. Robotic insertion of various ablation needles under computed tomography guidance: accuracy in animal experiments. Eur J Radiol. 2018;105:162–7. https://doi.org/10.1016/j.ejrad.2018.06.006.
Kettenbach J, Kronreif G. Robotic systems for percutaneous needle-guided interventions. Minim Invasive Ther Allied Technol MITAT. 2015;24(1):45–53. https://doi.org/10.3109/13645706.2014.977299.
Won HJ, Kim N, Kim GB, Seo JB, Kim H. Validation of a CT-guided intervention robot for biopsy and radiofrequency ablation: experimental study with an abdominal phantom. Diagn Interv Radiol. 2017;23(3):233–7. https://doi.org/10.5152/dir.2017.16422.
Guha D, Alotaibi NM, Nguyen N, Gupta S, McFaul C, Yang VXD. Augmented reality in neurosurgery: a review of current concepts and emerging applications. Can J Neurol Sci. 2017;44(3):235–45. https://doi.org/10.1017/cjn.2016.443.
Heinrich F, Joeres F, Lawonn K, Hansen C. Comparison of projective augmented reality concepts to support medical needle insertion. IEEE Trans Vis Comput Gr. 2019. https://doi.org/10.1109/tvcg.2019.2903942.
Besharati Tabrizi L, Mahvash M. Augmented reality-guided neurosurgery: accuracy and intraoperative application of an image projection technique. J Neurosurg. 2015;123(1):206–11. https://doi.org/10.3171/2014.9.Jns141001.
Marker DR, Paweena U, Thainal TU, Flammang AJ, Fichtinger G, Iordachita II, et al. 1.5 T augmented reality navigated interventional MRI: paravertebral sympathetic plexus injections. Diagn Interv Radiol. 2017;23(3):227–32. https://doi.org/10.5152/dir.2017.16323.
Eftekhar B. A smartphone app to assist scalp localization of superficial supratentorial lesions-technical note. World Neurosurg. 2016;85:359–63. https://doi.org/10.1016/j.wneu.2015.09.091.
Kenngott HG, Preukschas AA, Wagner M, Nickel F, Muller M, Bellemann N, et al. Mobile, real-time, and point-of-care augmented reality is robust, accurate, and feasible: a prospective pilot study. Surg Endosc. 2018;32(6):2958–67. https://doi.org/10.1007/s00464-018-6151-y.
van Oosterom MN, van der Poel HG, Navab N, van de Velde CJH, van Leeuwen FWB. Computer-assisted surgery: virtual- and augmented-reality displays for navigation during urological interventions. Curr Opin Urol. 2018;28(2):205–13. https://doi.org/10.1097/mou.0000000000000478.
Cutolo F, Meola A, Carbone M, Sinceri S, Cagnazzo F, Denaro E, et al. A new head-mounted display-based augmented reality system in neurosurgical oncology: a study on phantom. Comput Assist Surg. 2017;22(1):39–53. https://doi.org/10.1080/24699322.2017.1358400.
Maruyama K, Watanabe E, Kin T, Saito K, Kumakiri A, Noguchi A, et al. Smart glasses for neurosurgical navigation by augmented reality. Oper Neurosurg. 2018;15(5):551–6. https://doi.org/10.1093/ons/opx279.
Witowski J, Darocha S, Kownacki L, Pietrasik A, Pietura R, Banaszkiewicz M, et al. Augmented reality and three-dimensional printing in percutaneous interventions on pulmonary arteries. Quant Imaging Med Surg. 2019;9(1):23–9. https://doi.org/10.21037/qims.2018.09.08.
Racadio JM, Nachabe R, Homan R, Schierling R, Racadio JM, Babic D. Augmented reality on a C-arm system: a preclinical assessment for percutaneous needle localization. Radiology. 2016;281(1):249–55. https://doi.org/10.1148/radiol.2016151040.
Rosenthal M, State A, Lee J, Hirota G, Ackerman J, Keller K, et al. Augmented reality guidance for needle biopsies: an initial randomized, controlled trial in phantoms. Med Image Anal. 2002;6(3):313–20.
Wacker FK, Vogt S, Khamene A, Jesberger JA, Nour SG, Elgort DR, et al. An augmented reality system for MR image-guided needle biopsy: initial results in a swine model. Radiology. 2006;238(2):497–504. https://doi.org/10.1148/radiol.2382041441.
Fichtinger G, Deguet A, Masamune K, Balogh E, Fischer GS, Mathieu H, et al. Image overlay guidance for needle insertion in CT scanner. IEEE Trans Bio-med Eng. 2005;52(8):1415–24. https://doi.org/10.1109/tbme.2005.851493.
Solbiati M, Passera KM, Rotilio A, Oliva F, Marre I, Goldberg SN, et al. Augmented reality for interventional oncology: proof-of-concept study of a novel high-end guidance system platform. Eur Radiol Exp. 2018;2:18. https://doi.org/10.1186/s41747-018-0054-5.
Negussie AH, Partanen A, Mikhail AS, Xu S, Abi-Jaoudeh N, Maruvada S, et al. Thermochromic tissue-mimicking phantom for optimisation of thermal tumour ablation. Int J Hyperth. 2016;32(3):239–43. https://doi.org/10.3109/02656736.2016.1145745.
Grasso RF, Faiella E, Luppi G, Schena E, Giurazza F, Del Vescovo R, et al. Percutaneous lung biopsy: comparison between an augmented reality CT navigation system and standard CT-guided technique. Int J Comput Assist Radiol Surg. 2013;8(5):837–48. https://doi.org/10.1007/s11548-013-0816-8.
Beca F, Polyak K. Intratumor heterogeneity in breast cancer. Adv Exp Med Biol. 2016;882:169–89. https://doi.org/10.1007/978-3-319-22909-6_7.
Kyrochristos ID, Ziogas DE, Roukos DH. Drug resistance: origins, evolution and characterization of genomic clones and the tumor ecosystem to optimize precise individualized therapy. Drug Discov Today. 2019. https://doi.org/10.1016/j.drudis.2019.04.008.
Asvadi NH, Anvari A, Uppot RN, Thabet A, Zhu AX, Arellano RS. CT-guided percutaneous microwave ablation of tumors in the hepatic dome: assessment of efficacy and safety. J Vasc Interv Radiol JVIR. 2016;27(4):496–502. https://doi.org/10.1016/j.jvir.2016.01.010quiz 3.
de Baere T, Tselikas L, Catena V, Buy X, Deschamps F, Palussiere J. Percutaneous thermal ablation of primary lung cancer. Diagn Interv Imaging. 2016;97(10):1019–24. https://doi.org/10.1016/j.diii.2016.08.016.
Shady W, Petre EN, Gonen M, Erinjeri JP, Brown KT, Covey AM, et al. Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes—a 10-year experience at a single center. Radiology. 2016;278(2):601–11. https://doi.org/10.1148/radiol.2015142489.
Acknowledgements
This research was supported by the Intramural Research Program of the NIH Center for Interventional Oncology. The authors thank Elizabeth Levin, Reza Seifabadi, Michal Mauda-Havakuk, Ivane Bakhutashvili, and Andrew Mikhail for contributing their time as operators in Experiment 1. We also thank Ayele Negussie for constructive conversations on the design of the test phantoms.
Funding
This work was supported by the Center for Interventional Oncology in the Intramural Research Program of the National Institutes of Health (NIH) by intramural NIH Grants NIH Z01 1ZID BC011242 and CL040015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hecht, R., Li, M., de Ruiter, Q.M.B. et al. Smartphone Augmented Reality CT-Based Platform for Needle Insertion Guidance: A Phantom Study. Cardiovasc Intervent Radiol 43, 756–764 (2020). https://doi.org/10.1007/s00270-019-02403-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-019-02403-6