Abstract
Purpose
To evaluate the protective effect of using thermo-sensitive basement membrane extract (Matrigel) for hydrodissection to minimize thermal injury to nearby structures and to evaluate its heat sink effect on the ablation zone in radiofrequency ablation (RFA) of the liver.
Materials and Methods
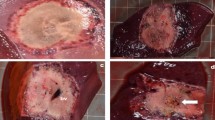
First, the viscosity profile and heat sink effect of Matrigel were assessed during RFA in vitro and ex vivo. Fresh pig liver tissue was used, and the temperature changes in Matrigel and in 5% dextrose in water (D5W) during RFA were recorded. Then, the size of the ablation zone in the peripheral liver after RFA was measured. Second, in an in vivo study, 45 Sprague–Dawley rats were divided into three groups of 15 rats each (Matrigel, D5W and control). In the experimental groups, artificial ascites with 10 ml of Matrigel or D5W were injected using ultrasound guidance prior to RFA. The frequency of thermal injury to the nearby organs was compared among the three groups, with assessments of several locations: near the diaphragm, the abdominal wall and the gastrointestinal (GI) tract. Finally, the biological degradation of Matrigel by ultrasound was evaluated over 60 days.
Results
First, Matrigel produced a greater heat retention (less heat sink) effect than D5W during ex vivo ablation (63 ± 9 vs. 26 ± 6 °C at 1 min on the surface of the liver, P < 0.001). Hepatic ablation zone volume did not differ between the two groups. Second, thermal injury to the nearby structures was found in 14 of 15 cases (93.3%) in the control group, 8 of 15 cases (53.3%) in the D5W group, and 1 of 15 cases (6.7%) in the Matrigel group. Significant differences in the thermal injury rates for nearby structures were detected among the three groups (P < 0.001). The most significant difference in the thermal injury rate was found in locations near the GI tract (P = 0.003). Finally, Matrigel that was injected in vivo was gradually degraded during the following 60 days.
Conclusions
Using thermo-sensitive Matrigel as a hydrodissection material might help reduce the frequency of collateral thermal injury to nearby structures, especially in locations close to the GI tract, compared to conventional D5W. Additionally, Matrigel did not increase the heat sink effect on the ablation zone during ablation and was degraded over time in vivo.





Similar content being viewed by others
References
Gao J, Wang SH, Ding XM, et al. Radiofrequency ablation for single hepatocellular carcinoma 3 cm or less as first-line treatment. World J Gastroenterol. 2015;21(17):5287–94.
Yan K, Chen MH, Yang W, et al. Radiofrequency ablation of hepatocellular carcinoma: long-term outcome and prognostic factors. Eur J Radiol. 2008;67:336–47.
Lee YH, Hsu CY, Chu CW, et al. Radiofrequency ablation is better than surgical resection in patients with hepatocellular carcinoma within the Milan criteria and preserved liver function: a retrospective study using propensity score analyses. J Clin Gastroenterol. 2015;49(3):242–9.
Yang W, Yan K, Goldberg SN, et al. Ten-year survival of hepatocellular carcinoma patients undergoing radiofrequency ablation as a first-line treatment. World J Gastroenterol. 2016;22(10):2993–3005.
Solbiati L, Ahmed M, Cova L, Ierace T, Brioschi M, Goldberg SN. Small liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-up. Radiology. 2012;265:958–68.
Chen MH, Wei Y, Yan K, et al. Treatment strategy to optimize radiofrequency ablation for liver malignancies. J Vasc Interv Radiol. 2006;17:671–83.
Osaki Y, Nishikawa H. Treatment for hepatocellular carcinoma in Japan over the last three decades: our experience and published work review. Hepatol Res. 2015;45(1):59–74.
Kim JW, Shin SS, Heo SH, et al. Ultrasound-guided percutaneous radiofrequency ablation of liver tumors: how we do it safely and completely. Korean J Radiol. 2015;16(6):1226–39.
Farrell MA, Charboneau JW, Callstrom MR, Reading CC, Engan DE, Blute ML. Paranephric water instillation: a technique to prevent bowel injury during percutaneous renal radiofrequency ablation. AJR Am J Roentgenol. 2003;181:1315–7.
Rhim H, Lim HK, Kim YS, Choi D. Percutaneous radiofrequency ablation with artificial ascites for hepatocellular carcinoma in the hepatic dome: initial experience. AJR Am J Roentgenol. 2008;190:91–8.
Raman SS, Aziz D, Chang X, Sayre J, Lassman C, Lu D. Minimizing diaphragmatic injury during radiofrequency ablation: efficacy of intraabdominal carbon dioxide insufflation. AJR Am J Roentgenol. 2004;183:197–200.
Yamakado K, Nakatsuka A, Akeboshi M, Takeda K. Percutaneous radiofrequency ablation of liver neoplasms adjacent to the gastrointestinal tract after balloon catheter interposition. J Vasc Interv Radiol. 2003;14(9 Pt 1):1183–6.
Kleinman HK, Martin GR. Matrigel: basement membrane matrix with biological activity. Semin Cancer Biol. 2005;15:378–86.
Vukicevic S, Kleinman HK, Luyten FP, Roberts AB, Roche NS, Reddi AH. Identification of multiple active growth factors in basement membrane Matrigel suggests caution in interpretation of cellular activity related to extracellular matrix components. Exp Cell Res. 1992;202:1–8.
Fu JJ, Wang S, Guan RH, Yang W, Yan K, Chen MH. Effect of thermo-sensitive Matrigel on minimization of thermal injury to the nearby structures in radiofrequency ablation of subcapsular hepatic tumors in a rat model. Natl Med J China. 2016;96:43–7. doi:10.3760/cma.j.issn.0376-2491.2016.01.010 PMID: 26792607.
Livraghi T, Solbiati L, Meloni MF, Gazelle GS, Halpern EF, Goldberg SN. Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology. 2003;226:441–51.
de Baere T, Risse O, Kuoch V, et al. Adverse events during radiofrequency treatment of 582 hepatic tumors. AJR Am J Roentgenol. 2003;181:695–700.
Dodd GD 3rd, Soulen MC, Kane RA, et al. Minimally invasive treatment of malignant hepatic tumors: at the threshold of a major breakthrough. RadioGraphics. 2000;20:9–27.
Raman SS, Lu DS, Vodopich DJ, Sayre J, Lassman C. Minimizing diaphragmatic injury during radio-frequency ablation: efficacy of subphrenic peritoneal saline injection in a porcine model. Radiology. 2002;222:819–23.
Rhim H. Complications of radiofrequency ablation in hepatocellular carcinoma. Abdom Imaging. 2005;30:409–18.
Ishikawa T, Kubota T, Horigome R, et al. Radiofrequency ablation during continuous saline infusion can extend ablation margins. World J Gastroenterol. 2013;19(8):1278–82.
Hasegawa T, Takaki H, Miyagi H, et al. Hyaluronic acid gel injection to prevent thermal injury of adjacent gastrointestinal tract during percutaneous liver radiofrequency ablation. Cardiovasc Interv Radiol. 2013;36:1144–6.
Langen HJ, Jochims M, Gunther RW. Artificial displacement of kidneys, spleen, and colon by injection of physiologic saline and CO2 as an aid to percutaneous procedures: experimental results. J Vasc Interv Radiol. 1995;6(3):411–6.
Song I, Rhim H, Lim HK, Kim YS, Choi D. Percutaneous radiofrequency ablation of hepatocellular carcinoma abutting the diaphragm and gastrointestinal tracts with the use of artificial ascites: safety and technical efficacy in 143 patients. Eur Radiol. 2009;19:2630–40.
Laeseke PF, Sampson LA, Brace CL, Winter TC III, Fine JP, Lee FT Jr. Unintended thermal injuries from radiofrequency ablation: protection with 5% dextrose in water. AJR Am J Roentgenol. 2006;186(5 Suppl):S249–54.
Chen EA, Neeman Z, Lee FT, Kam A, Wood B. Thermal protection with 5% dextrose solution blanket during radiofrequency ablation. Cardiovasc Interv Radiol. 2006;29:1093–6.
Hughes CS, Postovit LM, Lajoie GA. Matrigel: a complex protein mixture required for optimal growth of cell culture. Proteomics. 2010;10:1886–90.
Benton G, George J, Kleinman HK, Arnaoutova IP. Advancing science and technology via 3D culture on basement membrane matrix. J Cell Physiol. 2009;221:18–25.
Arnaoutova I, George J, Kleinman HK, Benton G. The endothelial cell tube formation assay on basement membrane turns 20. Angiogenesis. 2009;12:267–74.
Lu DS, Raman SS, Vodopich DJ, Wang M, Sayre J, Lassman C. Effect of vessel size on creation of hepatic radiofrequency lesions in pigs: assessment of the “heat sink” effect. AJR Am J Roentgenol. 2002;178:47–51.
Kim SK, Lim HK, Ryu JA, et al. Radiofrequency ablation of rabbit liver in vivo: effect of the pringle maneuver on pathologic changes in liver surrounding the ablation zone. Korean J Radiol. 2004;5:240–9.
Kim YS, Rhim H, Paik SS. Radiofrequency ablation of the liver in a rabbit model: creation of artificial ascites to minimize collateral thermal injury to the diaphragm and stomach. J Vasc Interv Radiol. 2006;17:541–7.
Hinshaw JL, Laeseke PF, Winter TC 3rd, Kliewer MA, Fine JP, Lee FT Jr. Radiofrequency ablation of peripheral liver tumors: intraperitoneal 5% dextrose in water decreases postprocedural pain. AJR Am J Roentgenol. 2006;186:S306–10.
Brace CL, Laeseke PF, Prasad V, Lee FT. Electrical isolation during radiofrequency ablation: 5% dextrose in water provides better protection than saline. Conf Proc IEEE Eng Med Biol Soc. 2002;28:5021–4.
Kondo Y, Yoshida H, Shiina S, Tateishi R, Teratani T, Omata M. Artificial ascites technique for percutaneous radiofrequency ablation of liver cancer adjacent to the gastrointestinal tract. Br J Surg. 2006;93:1277–82.
Bodily KD, Atwell TD, Mandrekar JN, et al. Hydrodisplacement in the percutaneous cryoablation of 50 renal tumors. AJR Am J Roentgenol. 2010;194:779–83.
Lee EJ, Rhim H, Lim HK, Choi D, Lee WJ, Min KS. Effect of artificial ascites on thermal injury to the diaphragm and stomach in radiofrequency ablation of the liver: experimental study with a porcine model. AJR Am J Roentgenol. 2008;190:1659–64.
Acknowledgements
This paper was founded by the National Natural Science Foundation of China (No. 81471768) and the National Natural Science Foundation of Beijing (No. 7152031).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Fu, JJ., Wang, S., Yang, W. et al. Protective and Heat Retention Effects of Thermo-sensitive Basement Membrane Extract (Matrigel) in Hepatic Radiofrequency Ablation in an Experimental Animal Study. Cardiovasc Intervent Radiol 40, 1077–1085 (2017). https://doi.org/10.1007/s00270-017-1617-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-017-1617-1