Abstract
Background
The objective of this systematic review was to identify pre-existing quality performance indicators (QPIs) for the surgical management of oesophageal cancer (OC). These QPIs can be used to objectively measure and compare the performance of individual units and capture key elements of patient care to improve patient outcomes.
Methods
A systematic literature search of PubMed, MEDLINE, Scopus and Embase was conducted. Articles reporting on the quality of healthcare in relation to oesophageal neoplasm or cancer and the surgical treatment of OC available until the 1st of March 2022 were included.
Results
The final list of articles included retrospective reviews (n = 13), prospective reviews (n = 8), expert guidelines (n = 1) and consensus (n = 1). The final list of QPIs was categorized as process, outcome or structural measures. Process measures included multidisciplinary involvement, availability of multimodality diagnostic and treatment pathways and surgical metrics. Outcome measures included reoperation and readmission rates, the achievement of RO resection and length of hospital stay. Structural measures include multidisciplinary meetings.
Conclusions
This systematic review summarizes QPIs for the surgical treatment of OC. The data will serve as an introduction to establishing a quality initiative project for OC resections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oesophageal cancer (OC) is a lethal condition with a 5-year population-based survival rate of less than 20% [1]. Significant variation in approaches to the surgical and multimodality treatment for patients with OC exists and may contribute to differences in patient outcomes. Quality performance indicators (QPIs) capture key elements of patient care that can be utilized to objectively measure the quality of care, identify underperforming providers across jurisdictions and develop benchmarking standards. This differs from published guidelines on the management of oesophagogastric cancers, which aim to guide clinicians and patients in making decisions about oesophagogastric cancer. QPIs should translate to improvements in short- and long-term clinical outcomes for patients. The optimal treatment pathway for patients with OC is complex and multidisciplinary [2]. Despite the availability of published guidelines for the management of OC, there is a relative paucity of well-defined evidence-based standards for the evaluation of the quality of surgical care [3].
There is strong evidence in support of the concentration of the surgical treatment of OC in high-volume centres [2, 4,5,6]. Nevertheless, it is important to decipher specific reasons for these improvements in the outcome as they serve as an impetus for ongoing quality improvement projects. Individual QPIs highlighted should ideally include patient-reported outcomes even though these might be difficult to define and measure.
The primary aim of this review is to identify and characterize existing QPIs for the surgical management of OC in the literature. These QPIs are imperative to capture performance across all aspects of patient care and outcomes. In addition to this, it will allow for the comparison of outcomes between different units and thus highlight underperforming units.
Methods
Search terms included the following ‘Quality control OR Quality improvement OR Quality of healthcare OR Quality indicators’ OR ‘Benchmark’, AND ‘Oesophagectomy’ OR ‘Esophagectomy’ OR ‘Oesophageal neoplasm’ OR ‘Esophageal Neoplasm’ OR ‘Adenocarcinoma’ OR ‘Squamous Cell Cancer’ OR ‘Oesophageal resection’ OR ‘Esophageal Resection’ OR ‘Oesophageal cancer’ OR ‘Esophageal Cancer’ OR ‘Ivor Lewis’ OR ‘Oesophageal Surgery’ OR ‘Esophageal Surgery’. A systematic literature search of PubMed, MEDLINE, Scopus and Embase was conducted. All articles until the 1st of March 2022 were included. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was adhered [6]. Only papers in English were included, there were no geographical limits.
Study selection and analysis
Articles that discussed, evaluated or reported on QPIs relating to the management of OC were included in the final analysis. Any study that solely reported surgeon or hospital case volume was excluded from the final analysis. Two authors independently reviewed the publications according to the inclusion criteria. Discrepancies were resolved by consultation. All QPIs were identified from the articles and sub-categorized according to the Donabedian model, which places QPIs into structural, process or outcome indicators. Structural indicators refer to the physical attributes of the healthcare setting. Process indicators measure the activity performed by the healthcare providers such as diagnostic and therapeutic interventions. Outcome indicators are the effects of the care [7].
Pertinent details including study size, methodology and QPIs were recorded and rated according to the Oxford Centre for Evidence–Based Medicine [8]. All studies were categorized based on the level of evidence.
Level 1 Systematic reviews with homogeneity of randomized controlled trials. Individual randomized controlled trials.
Level 2 Homogenous cohort studies or low-quality randomized controlled trials (e.g. with < 80% follow-up).
Level 3 Systematic reviews with homogeneity of case–control studies or individual case–control studies.
Level 4 Case series.
Level 5 Expert opinion without critical appraisal.
Results
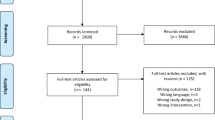
A total of 6722 article titles were screened (Fig. 1). The search strategy is detailed in Fig. 2. The only structure-based QPIs reported were MDT and hospital patient/procedure volume [9]. Case volume was excluded from our analysis as per the pre-defined exclusion criteria. Twenty-three articles were included in the final analyses as shown in Table 1. Table 2 details the extracted process and outcome QPIs. The selected studies included retrospective review (n = 13), prospective review (n = 8), expert guidelines (n = 1) and consensus (n = 1).
PRISMA [7] diagram describing the results of the systematic literature search and review
Structural indicator
Multidisciplinary team (MDT)
The delivery of high-quality OC management mandates multidisciplinary cooperation [9]. The efficient delivery and sequencing of different diagnostic and therapeutic interventions require discussion and documentation of all OC patients in an MDT meeting. Patient selection, investigation and management of patients with OC eligible for oesophagectomy by an MDT team resulted in improved survival compared to patients managed by surgeons alone [10]. The MDT should ideally include upper gastrointestinal surgeons, radiologists, pathologists and oncologists.
Formal standardized oesophagectomy care pathways and enhanced recovery pathways involving a multidisciplinary team including anaesthesia, intensive care, nursing, dietary and physical therapy was critical in achieving improved post-operative outcomes including median intensive care unit (ICU) stay, length of hospital stay and blood loss [11].
Process indicators
Multimodality treatment
The role of induction therapy and the timing of surgery post-induction therapy for patients with OC are important quality indicators. Adhia et al. concluded that based on existing studies and guidelines, induction therapy in the form of chemotherapy and /or radiation to clinical stage III OC should be completed before surgery. In this group of patients, surgery should be performed no more than 60 days after the completion of induction therapy [9]. Samson et al. [1] corroborate the salient point that while early-stage patients may proceed directly to endoscopic or surgical resection, patients who are deemed operable with locally advanced (Stage IIb/IIIb) OC should be considered for induction therapy, typically chemoradiation followed by resection. Of note, patients receiving induction chemoradiation were less likely to have positive margins. This approach is supported by the National Comprehensive Cancer Network (NCCN) [12].
RO resection and lymphadenectomy
One of the quality indicators reflective of a successful oesophagectomy is the number of retrieved lymph nodes [13]. Most investigators emphasize the importance of adequate dissection, however, the exact number of lymph nodes required varied between studies. Most of the articles considered the evaluation of 15 or more lymph nodes ideal [1, 9, 14, 15].
However, some expert centres advocated for more lymph nodes to be sampled or to be sampled in a stage-dependent manner. For example, Kalff et al. [16] record 20 or more lymph nodes. Helminen used the benchmark value of 23 or more lymph nodes [17]. Achieving a complete surgical resection with negative microscopic surgical margins (R0 Resection) remains a key QPI for both early and locally advanced OC [1, 9, 18, 19].
Failure to rescue
Failure to rescue (FTR) is the failure or delay in recognizing and responding to a hospitalized patient experiencing complications from a disease process or medical intervention [20].
Busweiler et al. emphasized that ‘failure to rescue’ is the most important quality parameter after mortality and morbidity. In addition to this, the timely recognition and early effective management of complications have a great effect on post-operative mortality after a major surgical complication [19].
Outcome indicators
Mortality is a key performance indicator in OC patients. Short- and long-term mortality rates are critical QPIs for patients undergoing oesophagectomy as deaths related to complications of surgery or cancer recurrence reflect the quality of surgical care delivered to the patient, and 30-day and 90-day mortality after oesophagectomy are well-documented performance indicators [18, 21,22,23,24,25,26,27]. Nevertheless, Talsma et al. [23] conclude that 90-day mortality rates are an improved quality indicator compared to the 30-day mortality rate and in-hospital mortality. Other outcome indicators were primarily focused on important post-operative complication rates such as an anastomotic leak, pulmonary complication rates, length of stay, readmission, reintervention rates as well as short- and long-term disease and overall survival rates.
Discussion
Despite advancements in the management of OC, it remains a lethal malignancy with a relatively dismal prognosis. It is a significant global health issue with a 5-year survival rate of 20% overall [1] and less than 50% for locally advanced disease [28].
The modernization of surgical and endoscopic techniques for the management of early OC and complications have contributed to improved patient outcome. Nevertheless, much of the improvement in OC outcomes can be attributed to better patient selection through improved pre-operative staging and the delivery of multimodal induction therapy. The multidimensional nature of OC therapy has mandated the sequential coordination of care delivered by different specialist groups to ensure optimized outcomes. QPIs allow for the objective measurement of all aspects of the patient pathway.
Process QPIs were heterogenous but broadly fell into two groups. These were specifically accepted surgical metrics and the utilization of specialized staging, endoscopic and the active involvement of a multidisciplinary team. Process indicators included lymphadenectomy of 15 or more lymph nodes, the administration of induction therapy, the surgical approach including endoscopic and minimally invasive oesophagectomy and the utilization of specific oesophagectomy pathways [29]. The complexity and ever-evolving nature of modern diagnostic and therapeutic options for OC mandates the discussion of all OC cases at a specialized MDT. In addition to this, the early involvement of a palliative care team in an MDT is imperative albeit not commonly instituted. Although the added value can be hard to measure, it would seem intuitive as a significant proportion of patients with OC are non-operable and referred for the best supportive care [29].
Processes involving perioperative care including prompt identification and management of patients with surgical complications are significant QPIs. Failure to rescue patients with complications after OC surgery is an important QPI. The early identification and expedient management of complications is dependent upon several key factors including consultant-led services with clear escalation pathways, the availability of resources and expertise such as ICUs, theatre availability and diagnostic and interventional radiology services [19]. Other less measurable concepts that improve this include attitudes, behaviours and departmental culture. Early escalation and discussion with other senior surgeons combined with other specialities are key to ensuring early patient care.
Surprisingly, aside from the volume-outcome correlation and involvement of the MDT, validated structural QPIs for OC such as level of staffing, presence of a specific surgical ICU and staff skill composition were limited. The lack of QPIs in this area holds the promise of improvement. In addition to improved surgical technique and higher quality perioperative care, improvements in mortality and morbidity in high-volume units may be attributed to possessing standardized pathways as a central component of enhanced recovery programmes. Formal oesophagectomy care pathways have demonstrated promising results in improving perioperative care, post-operative mortality and operative textbook outcomes as well as improved efficiency in quality health care delivery. Textbook outcome measures encompass a bundle of clinical outcomes, which represents the ideal post-operative course in patients with OC [30]. In addition to this, care pathways have also been shown to reduce the length of stay and costs involved in oesophagectomy [31].
There is significant heterogeneity in the specific operative approach to a patient with resectable OC. The decision-making is complex and should consider tumour location, patient comorbidities, surgeon and institutional experience. Regarding operative approach and technique, a meta-analysis has shown no clear-cut difference in short- or long-term outcomes between different techniques [31]. Minimally invasive surgery for OC surgery improves patient recovery without jeopardizing the quality of oncological resection. The MIRO trial demonstrated a lower incidence of intraoperative and post-operative major complications, specifically pulmonary complications in the hybrid minimally invasive oesophagectomy group compared to open oesophagectomy without compromising oncological outcome [32]. This was supported by the TIME and RAMIE trial, which demonstrated no difference in disease-free and overall, 3-year survival [33, 34]. Despite its advantages, minimally invasive resection is not as widely disseminated as it is in colorectal surgery. This may be attributed to several factors including operative complexity, surgeon and lack of robust long-term data on patients undergoing minimally invasive oesophagectomy (MIO). There is limited evidence to suggest that MIO should be a QPI. Bolger et al. concluded that when MIO was included as an outcome measure, patients achieving a textbook outcome measure demonstrated improved overall survival rates. Appropriate surgeon training in ideally high-volume centres is critical in achieving high-quality surgery. A review by Stall et al. identified three studies reporting the influence of subspecialty training on outcomes. Two studies demonstrated lower post-operative mortality if operated on by cardiothoracic surgeons compared to patients operated on by general surgeons. A third study demonstrated no difference in outcome between general and thoracic surgeons. To date, there have been no studies comparing dedicated oesophagogastric surgeons and thoracic surgeons. This highlights the potential importance of surgical sub-specialization and areas of training [3].
Outcome measures included specific complication rates, post-operative morbidity, recovery and mortality at the 30-and 90-day post-operative mortality data. This is commensurate with the National Institute for Health and Care Excellence (NICE) guidelines, Dutch Upper GI Cancer audit group and Queensland Oesophagogastric Surgery Quality index including no intraoperative complications, tumour-negative resection margins, minimum 15 lymph nodes, no severe post-operative complications, no reintervention/readmission to ICU, no prolonged hospitalization (21 days or less) and no readmission after discharge or post-operative mortality [9, 35, 36].
One of the limitations of this study is that our search only identified healthcare-related QPIs and not patient-reported quality measures. This is increasingly being recognized as a cornerstone of OC surgical management. This is particularly important for the older, frail or palliative OC patient where the quality-of-life measures are imperative and must be incorporated into the greater framework of quality indicator measurements. Standard processes to prevent hospital-acquired complications such as deep venous thrombus and surgical wound infection rates are important considerations, which will be key QPIs for future studies.
The data from this review will be used to develop a set of internationally agreed and measurable QPIs for OC. QPIs that warrant further investigation include robotic approaches, ideal endoscopic therapeutic management of complications as well as the effect of further surgical subspecialty training. In conclusion, this paper summarizes the structural, process and outcome-based QPIs that are both clinically relevant and measurable. These QPIs can be utilized to provide objective measurements of outcomes and allow comparison between different units. These should ideally translate to improved short- and long-term patient outcomes and provide the basis for future quality improvement projects.
References
Samson P, Puri V, Broderick S et al (2017) Adhering to quality measures in esophagectomy is associated with improved survival in all stages of esophageal cancer. Ann Thorac Surg 103:1101–1108
Burton PR, Ooi GJ, Shaw K et al (2018) Assessing quality of care in oesophago-gastric cancer surgery in Australia. ANZ J Surg 88:290–295
Staal EFWC, Wouters MWJM, Boot H et al (2010) Quality-of-care indicators for oesophageal cancer surgery: a review. Eur J Surg Oncol 36:1035–1043
Birkmeyer JD, Stukel TA, Siewers AE et al (2003) Surgeon volume and operative mortality in the United States. N Engl J Med 349:2117–2127
Rouvelas I, Lagergren J (2010) The impact of volume on outcomes after oesophageal cancer surgery. ANZ J Surg 80:634–641
Gordon TA, Bowman HM, Bass EB et al (1999) Complex gastrointestinal surgery: impact of provider experience on clinical and economic outcomes. J Am Coll Surg 189:46–56
Rourke AJ (1957) Evaluating the quality of medical care. Hosp Prog 38:72–73
Centre for Evidence-Based Medicine (2023) OCEBM Levels of Evidence [Internet]. Nuffield department of primary care health sciences: university of Oxford; 2023 [Cited 5 June 2022.] Available from: https://www.cebm.net/2016/05/ocebm-levels-of-evidence/
Adhia A, Feinglass J, Schlick CJ et al (2020) Adherence to quality measures improves survival in esophageal cancer in a retrospective cohort of the national cancer database from 2004 to 2016. J Thorac Dis 12:5441–5459
Stephens MR, Lewis WG, Brewster AE et al (2006) Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus 19:164–171
Markar SR, Karthikesalingam A, Low DE (2015) Enhanced recovery pathways lead to an improvement in postoperative outcomes following esophagectomy: systematic review and pooled analysis. Dis Esophagus 28:468–475
Ajani JA, D’Amico TA, Bentrem DJ et al (2019) Esophageal and esophagogastric junction cancer version 2. J Natl Compr Canc Netw 17:855–883
Matsuda S, Kataga Y (2021) The potential of lymph node yield as a quality indicator of esophagectomy for esophageal cancer. Ann Surg Oncol 28:9–10
Merkow RP, Bilimoria KY, Chow WB et al (2012) Variation in lymph node examination after esophagectomy for cancer in the United States. Arch Surg 147:505–511
Schlick CJR, Khorfan R, Odell DD et al (2020) Adequate lymphadenectomy as a quality measure in esophageal cancer: Is there an association with treatment approach? Ann Surg Oncol 27:4443–4456
Kalff MC, van Berge Henegouwen MI (2021) Textbook outcome for esophageal cancer surgery: An international consensus-based update of a quality measure. Dis Esophagus 34:doab011
Helminen O, Mrena J, Sihvo E (2020) Benchmark values for transthoracic esophagectomy are not set as the defined “best possible”–a validation study. Ann Thorac Surg 109:383–388
Carroll PA, Jacob N, Yeung JC et al (2020) Using benchmarking standards to evaluate transition to minimally invasive esophagectomy. Ann Thorac Surg 109:383–388
Busweiler LA, Henneman D, Dikken JL et al (2017) Failure-to-rescue in patients undergoing surgery for esophageal or gastric cancer. Eur J Surg Oncol 43:1962–1969
Hall KK, Lim A, Gale B (2020) Failure to rescue. In: Making healthcare safer III: a critical analysis of existing and emerging patient safety practices. Agency for Healthcare Research and Quality (US), Rockville, pp 102–117
Walters DM, McMurry TL, Isbell JM et al (2014) Understanding mortality as a quality indicator after esophagectomy. Ann Thorac Surg 98:502–506
Staiger RD, Gutschow CA (2019) Benchmark analyses in minimally invasive esophagectomy–impact on surgical quality improvement. J Thorac Dis 11:S771-776
Talsma AK, Lingsma HF, Steyerberg EW et al (2014) The 30-day versus in-hospital and 90-day mortality after esophagectomy as indicators for quality of care. Ann Surg 260:267–273
Al Azzawi M, Bolger J, Whooley J et al (2020) Textbook surgical outcomes in esophageal cancer: the influence of national key performance indicators. Dis Esophagus 33:doaa087-45
In H, Palis BE, Merkow RP et al (2016) Doubling of 30-day mortality by 90-days after esophagectomy: a critical measure of outcomes for quality improvement. Ann Surg 263:286–291
Schmidt HM, Gisbertz S, Moons J et al (2017) Defining benchmarks for transthoracic esophagectomy. Ann Surg 266:814–821
Kulshrestha S, Bunn C, Patel PM et al (2020) Textbook oncologic outcome is associated with increased overall survival after esophagectomy. Surgery 168:953–961
Ng SP, Leong T (2021) Indications for definitive chemoradiotherapy for oesophageal cancer. Ann Esophagus 4:43
Stordeur S, Vlayen J, Vrijens F et al (2015) Quality indicators for oesophageal and gastric cancer: a population-based study in Belgium, 2004–2008. Eur J Cancer Care 24:376–386
Bolger JC, Al Azzawi M, Whooley J et al (2021) Surgery by a minimally invasive approach is associated with improved textbook outcomes in oesophageal and gastric cancer. Eur J Surg Oncol 47:2332–2339
Markar SR, Schmidt H, Kunz S et al (2014) Evolution of standardized clinical pathways: refining multidisciplinary care and process to improve outcomes of the surgical treatment of esophageal cancer. J Gastrointest Surg 18:1238–1246
Mariette C, Markar SR, Dabakuyo-Yonli TS et al (2019) Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med 380:152–162
Straatman J, van der Wielen N, Cuesta MA et al (2017) Minimally invasive versus open esophageal resection: three-year follow-up of the previously reported randomized controlled trial: the TIME Trial. Ann Surg 266:232–236
Yang Y, Li B, Yi J et al (2022) Robot-assisted versus conventional minimally invasive esophagectomy for resectable esophageal squamous cell carcinoma: early results of a multicenter randomized controlled trial: the RAMIE trial. Ann Surg 275:646–653
Busweiler LAD, Wijnhoven BPL, van Berge Henegouwen MI et al (2016) The dutch upper GI cancer audit: 2011–2014. J Clin Oncol 34:309
Queensland Government (2017) Queensland oesophagogastric surgery quality index: indicators of safe, quality cancer care. Cancer surgery in public and private hospitals 2004–2013. Queensland Health, Brisbane
Low DE, Kuppusamy MK, Alderson D et al (2019) Benchmarking complications associated with esophagectomy. Ann Surg 269:291–298
Low DE, Kunz S, Schembre D et al (2007) Esophagectomy- it’s not just about mortality anymore: standardized perioperative clinical pathways improve outcomes in patients with esophageal cancer. J Gastrointest Surg 11:1395–1402
Busweiler LA, Schouwenburg MG, van Berge Henegouwen MI et al (2017) Textbook outcome as a composite measure in oesophageogastric cancer surgery. Br J Surg 104:742–750
Valsangkar N, Salfity HB, Timsina L et al (2018) Operative time in esophagectomy: does it affect outcomes? Surgery 164:866–871
Traverso LW, Shinchi H, Low DE (2004) Useful benchmarks to evaluate outcomes after esophagectomy and pancreaticoduodenectomy. Am J Surg 187:604–608
Khoushhal Z, Canner J, Schneider E et al (2016) Influence of specialty training and trainee involvement on perioperative outcomes of esophagectomy. Ann Thorac Surg 102:1829–1836
Allum W, Lordick F, Alsina M et al (2018) ECCO essential requirements for quality cancer care: oesophageal and gastric cancer. Crit Rev Oncol Hematol 122:179–193
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kulasegaran, S., Wang, Y., Woodhouse, B. et al. Quality Performance Indicators for the Surgical Management of Oesophageal Cancer: A Systematic Literature Review. World J Surg 47, 3262–3269 (2023). https://doi.org/10.1007/s00268-023-07216-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07216-w