Abstract
Background
Burn injuries are common in low- and middle-income countries (LMICs) and their associated disability is tragic. This study is the first to explore burn scars in rural communities in Mozambique. This work also validated an innovate burn assessment tool, the Morphological African Scar Contractures Classification (MASCC), used to determine surgical need.
Methods
Using a stratified, population-weighted survey, the team interviewed randomly selected households from September 2012 to June 2013. Three rural districts (Chókwè, Nhamatanda, and Ribáuè) were selected to represent the southern, central and northern regions of the country. Injuries were recorded, documented with photographs, and approach to care was gathered. A panel of residents and surgeons reviewed the burn scar images using both the Vancouver Scar Scale and the MASCC, a validated visual scale that categorizes patients into four categories corresponding to levels of surgical intervention.
Results
Of the 6104 survey participants, 6% (n = 370) reported one or more burn injuries. Burn injuries were more common in females (57%) and most often occurred on the extremities. Individuals less than 25 years old had a significantly higher odds of reporting a burn scar compared to people older than 45 years. Based on the MASCC, 12% (n = 42) would benefit from surgery to treat contractures.
Conclusion
Untreated burn injuries are prevalent in rural Mozambique. Our study reveals a lack of access to surgical care in rural communities and demonstrates how the MASCC scale can be used to extend the reach of surgical assessment beyond the hospital through community health workers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Burns are a significant cause of preventable morbidity and mortality in sub-Saharan Africa [1]. Low-income countries, like Mozambique, disproportionately bear the burden of burns and may have inadequate resources to treat them [2]. Burn injuries are most common in children under 12 years old and limited access to surgical care negatively impact the outcomes of these injuries [3, 4] While incidence and severity of burns has been explored in emergency room admissions to large hospitals in different sub-Saharan African locations, the surgical burden of burn injuries outside these large centers is not well characterized [5, 6]. Community-level research is necessary to capture this information and inform the medical community of the true extent of burn injuries [7].
The World Health Organization (WHO) notes that burns are among the leading cause of daily-adjusted life years (DALYs) lost in low- and middle-income countries [8]. Roughly 180,000 deaths per year are attributed to burns with the majority occurring in sub-Saharan Africa. The Institute for Health Metrics and Evaluation estimates 172.07 per 100,000 DALYs lost because of fire, heat, and hot substances in Mozambique in 2019 [9]. Beyond mortality, burn injuries often require long hospital stay and can lead to debilitating long-term effects [10]. In areas where access to medical care is limited, burn survivors are forced to carry the significant physical and psychological burden these associated with these injuries [11]. Burn location is an important influence on management and long-term outcomes [12]. Burn injuries and the resulting scars, especially near joints or in the distal extremities, can lead to significant physical limitations and occasionally cause a permanent disability [13].
Scoring scars and qualifying the need for surgical intervention is vital to accurately assess need. Though multiple rating scales to assess burn scars exist in the literature, most require a comprehensive physical exam and standardized photographs to be effective [14, 15]. These data and the corresponding photographs gathered by community health workers in a large-scale survey require a simpler rating scale that can accurately reflect surgical need without necessitating complex techniques and expensive equipment.
This study sought to quantify the prevalence of burn scars in three rural communities in Mozambique, qualify these injuries with a novel scar scale, and determine the proportion amenable to surgical intervention.
Methods
Data collection
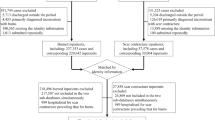
Approval was obtained from the UCSD Human Research Protection Program and the National Bioethics Committee in Mozambique. The research team queried a database outlined by Rose et al., who gathered a stratified, population-weighted household survey in three rural districts (Chókwè, Nhamatanda, and Ribáuè) of Mozambique in 2012 and 2013 (Fig. 1) [16]. They were chosen to represent the southern, central and northern regions of the country [16]. Each member of the selected households was surveyed and injuries were coded into six distinct anatomical areas: face/head/neck, chest/breast, back, abdomen, groin/genitals/buttocks, and extremities. Approach to treatment were also gathered. Photographs of the relevant condition were taken with a smartphone, coded to protect patient identity and linked to the individual’s responses. These data were stored on a password-protected server in a cloud storage environment. (Dropbox Inc. San Francisco, CA, USA).
Map of three rural study sites in Mozambique adapted from Anderson et al. [21]
Primary analysis
All coded burns injuries were factored into overall prevalence, but those that were not matched with a photograph were removed from secondary data analysis because their anatomical location could not be verified.
Coding
Burn photographs were reclassified into the correct anatomical area when necessary. The Surgeons OverSeas Assessment of Surgical Need (SOSAS) guidelines were adapted for the reclassifications [17]. Burns that crossed joints were flagged for separate analysis.
Secondary analysis
A panel of general surgery residents and plastic surgeons reviewed the images using the Morphological African Scar Contractures Classification (MASCC) [18]. This scale uses three metrics, length, width and height compared to the joint a burn scar occupies, to categorize burns by the complexity of the surgery needed for their correction (Supplemental Material). The same panel of residents and surgeons also scored the images using the Vancouver Scar Scale, an established burn scar rating metric, to validate this novel tool [19, 20].
Statistical analysis
Descriptive statistics including age, gender, burn anatomical location and approach to care were calculated. Tables and plots were generated with divisions by age group and burn location. Statistical analysis was performed in R (Version 1.3.1093, RStudio Team (2020). RStudio: Integrated Development for R. RStudio, PBC, Boston, MA) using odds ratios to assess different sub-groups. Inter-rater reliability and inter-class correlation was calculated for the Vancouver Scar Scale, and Cohen’s Kappa was calculated for the categorical MASCC.
Results
Of the 6104 total survey respondents, 2383 (39%) were from Chókwè in the south, 1657 (27%) were from Nhamatanda in the central region, and 2064 (34%) were from Ribáuè in the north. There were slightly more females (3300, 54%) than males, and 22% of the total respondents were under 15 years of age.
A total of 370 (6%) individuals reported one or more burn injuries. Of the 370 individuals who reported a burn injury, 209 (57%) were female and 161 (43%) were male, but this observed difference was not statistically significant. As shown in Table 1, the age groups reporting the highest proportion of burns were 15–24 years (107, 8.22%), followed by the 5–14 years (68, 7.61%). Compared to individuals over 45 years of age, individuals in the age ranges 0–4, 5–14, and 15–24 all had statistically higher odds of reporting a burn scar. Of the 370 individuals reporting burns, 19 (5%) reported burns in multiple anatomical areas. After review of the data gathered, the accompanying photographs were used to verify anatomical location and recoded when necessary. A total of 47 individuals were excluded due to missing or inadequate photographs of the burns.
Accounting for this, a total of 322 individuals reported 347 unique burn injuries. As seen in Fig. 2, most of these injuries occurred in the extremities (76%) followed by the face/head/neck (8%) and the abdomen (6%). Burns in the extremity were most often reported on the lower leg. Thirty-five burns (10%) crossed a joint (Fig. 3). Regarding the timing of these injuries, 262 burns (76%) occurred more than 1 year prior, while the remaining 85 (24%) occurred within 1 year.
Table 2 shows the respondents’ approaches to seeking and receiving healthcare. Sixty-five percent of respondents (227) with burns sought healthcare at a facility. Most received dressings (203, 59%) and 16 (5%) received surgery. Of the minority that did not receive formal healthcare (105, 30%), “No need” was the most common response (42, 12%) followed by “No money for healthcare” (19, 5%). Fourteen respondents (4%) went to a traditional healer. Gender did not significantly affect the odds of seeking and receiving healthcare. Age and burn location significantly affected the odds of seeking healthcare, and burns crossing a joint were significantly more likely to receive surgery compared to burns that did not involve a joint (Table 2).
Based on the scale adapted from the MASCC, 42 (12%) burns would benefit from surgical correction to treat contractures. These burns had an average score on the VSS of 6.45 (IQR = 5–8). Most burn scars that could benefit from surgical correction are in the extremities and only five individuals (11.9%) had prior surgery (Table 3). Type D burns, characterized by long scars that occupy a larger portion of the related joint, were the most common across all raters, accounting for 53% of the surgical burns on average (Table 4). Interclass correlation (ICC) across all raters for the VSS was 0.951 (95% CI 0.923 – 0.971, p = < 0.001), and remained high when comparing within resident raters (ICC = 0.889, 95% CI 0.816 –0.937, p = < 0.001) and attending raters (ICC = 0.991, 95% CI 0.986–0.995, p = < 0.001) (Table 5). The MASCC showed moderate agreement between all raters (k = 0.421, 95% CI 0.365–0.478, p = < 0.001) and strong agreement between resident raters (k = 0.754, 95% CI 0.633–0.875, p = < 0.001). Across both scar scales, Type C and D burns had a higher average VSS score than their Type A and B counterparts (6.6 vs 5.6, p = 0.03). There was no significant difference in rating between the resident and attendings physician scorers.
Discussion
This study is the first of its kind to focus on the prevalence of burn scars in rural communities in Mozambique. The prevalence of burn scars as characterized by previous rural household surveys is between 6% (607 per 10,000) in Ghanaian children, and 4% (398 per 10,000) in Sierra Leone, which is similar to the prevalence found in this study of 6% (607 per 10,000) [10, 22]. While past community-based studies have focused on broadly-defined surgically correctable conditions, this work gathers individuals’ approach to care, photographs of relevant injuries, and is one of the first to focus exclusively on burn scars [23,24,25]. Using World Bank rural population estimates, there were an estimated 1.03 million individuals with burn scars in rural Mozambique in 2013 [26]. Using our findings that more than 12% of burn scars could benefit from surgical correction, this estimates that more than 130,000 individuals across rural Mozambique could benefit from corrective burn scar surgery.
This study shows that burns scars are common in rural Mozambique. While it has been documented that women are at an increased risk of sequelae from burn injuries, our data show no significant difference between men and women in healthcare sought or received [27,28,29]. Conversely, age and burn location have a significant influence on healthcare seeking behavior. Individuals ages 0–4 years, 5–14 years, and 25–45 years sought care at a significantly higher rate than individuals older than 45 years of age. Similarly, individuals reporting a burn to the face, head or neck were more likely to seek treatment than those who reported a burn to the chest or extremities. While most burns occurred more than 1 year before the time of the survey, one quarter of the burn injuries occurred within the year preceding the study. In addition to surgical correction of chronic burn scars, this highlights the importance of burn prevention strategies, such as safe cooking practices, in global burn care. In line with past reports in the literature, this study found that traditional healers do not play a large role in burn care [30].
There is limited access to safe surgical care in many LMICs [2, 31, 32]. Past work has cited burn depth to be the most important indication for surgery, but this work suggests the additional importance of joint involvement to the treatment paradigm [31]. In this study, burns that did not cross a joint were significantly more likely to be treated with dressings instead of a surgical procedure. Burns involving joints and the resulting contractures can severely limit range of motion and negatively impact function [12]. In rural communities such as those surveyed in this study, burns that involve joints should be carefully assessed for the need for surgical care to avoid potential long-term sequelae.
The adapted MASCC used in this study is an effective scale to qualify and rate burn scars by the complexity of the surgery needed for their correction. While previous research has considered acute burn care and the effectiveness of contracture release on functional outcomes, there has been limited work on primary evaluation of burn scars [33,34,35]. The significant agreement between attending physicians and residents shows the scales effectiveness across levels of surgical training. Nearly three quarters of the burns needing surgical correction would require an advanced reconstructive procedure like a perforator or cross flap. Most patients whose burn scars could benefit from surgical care had just received dressings for their injuries, and less than 15% reported a previous surgery. This outlines the unmet need for surgical burn care in rural communities in Mozambique. In the hands of a trained community health worker, this scale could be implemented to rate burn scars and qualify the degree of surgical complexity necessary for their correction. This could be used to more effectively allocate limited surgical resources in a country that in 2015 had an estimated 25 general surgeons serving a population of more than 29.5 million individuals [16].
This study has several limitations. First, it does not measure the total burden of burns in Mozambique because of its focus on burn scars. As an example, deaths from more severe burns are not captured in our study. Second, because our survey was done almost 10 years ago (2012–2013), we cannot be sure that our results represent the current state of burn care in rural areas of Mozambique. Nevertheless, because few investments have been made in improving surgical care in the more remote areas of Mozambique during the past 10 years, we are confident that our burn data still reflects the current situation in rural areas. Finally, our results are not generalizable to the entire population of Mozambique because rural and urban areas likely differ in burn epidemiology.
In conclusion, this community-based survey provides insight into the prevalence and severity of burn scars in rural Mozambique. This work can inform prevention and treatment strategies in regions where access to medical and surgical care is limited. Future research should work to characterize trends in burn scar incidence and prevention in rural settings and put this novel scale into practice to assess surgical need in a prospective study.
Data availability material
The dataset analyzed and the excel spread sheets for the analysis are available upon reasonable request from the corresponding author: pbarba@health.ucsd.edu.
References
Nthumba PM (2016) Burns in sub-Saharan Africa: a review. Burns 42:258–266. https://doi.org/10.1016/j.burns.2015.04.006
Stokes MAR, Johnson WD (2017) Burns in the Third World: an unmet need. Ann Burns Fire Disasters 30:243–246 (PubMed PMID: 29983673)
Albertyn R, Bickler SW, Rode H (2006) Paediatric burn injuries in Sub Saharan Africa-an overview. Burns 32:605–612. https://doi.org/10.1016/j.burns.2005.12.004
Barradas R, Cliff J (1996) Burns incidence in low-income suburbs of Maputo City, Mozambique. Burns J Int Soc Burn Injuries 22:167. https://doi.org/10.1016/s0305-4179(96)90035-2
De Sousa PD, Keyes CE, Wright DW, Click LA, Sasser SM, Macleod JBA (2010) The epidemiology of childhood injury in Maputo, Mozambique. Int J Emerg Med 3:157–163. https://doi.org/10.1007/s12245-010-0182-z
Taibo CLA, Moon TD, Joaquim OA, Machado CR, Merchant A, McQueen K et al (2016) Analysis of trauma admission data at an urban hospital in Maputo, Mozambique Int J Emerg Med 9:1–7. https://doi.org/10.1186/s12245-016-0105-8
Vos T (2009) Improving the quantitative basis of the surgical burden in low-income countries. PLoS Med 6:e1000149. https://doi.org/10.1371/journal.pmed.1000149 (PubMed PMID: 19771153)
Organization TWH. Burns. 2018.
Evaluation IfHMa. GBD Compare Seattle, WA: IHME University of Washington; 2022. Available from: https://vizhub.healthdata.org/gbd-compare/.
Wong EG, Groen RS, Kamara TB, Stewart KA, Cassidy LD, Samai M et al (2014) Burns in Sierra Leone: a population-based assessment. Burns 40:1748–1753. https://doi.org/10.1016/j.burns.2014.03.007
Mashreky SR, Rahman A, Chowdhury SM, Giashuddin S, Svanström L, Linnan M et al (2008) Consequences of childhood burn: findings from the largest community-based injury survey in Bangladesh. Burns. https://doi.org/10.1016/j.burns.2008.05.002 (PubMed PMID: 18674863)
Goverman J, Mathews K, Goldstein R, Holavanahalli R, Kowalske K, Esselman P et al (2017) Adult contractures in burn injury: a burn model system National Database Study. J Burn Care Res 38:e328–e336. https://doi.org/10.1097/BCR.0000000000000380 (PubMed PMID: 27380122)
Forjuoh SN, Guyer B, Ireys HT (1996) Burn-related physical impairments and disabilities in Ghanaian children: prevalence and risk factors. Am J Public Health 86:81–83. https://doi.org/10.2105/AJPH.86.1.81
Mecott GA, Finnerty CC, Herndon DN, Al-Mousawi AM, Branski LK, Hegde S et al (2015) Reliable scar scoring system to assess photographs of burn patients. J Surg Res 199:688–697. https://doi.org/10.1016/j.jss.2014.10.055
Tyack Z, Wasiak J, Spinks A, Kimble R, Simons M (2013) A guide to choosing a burn scar rating scale for clinical or research use. Burns 39:1341–1350. https://doi.org/10.1016/j.burns.2013.04.021 (PubMed PMID: 23768711)
Rose J, Bendix P, Funzamo C, Vaz F, da Costa AA, Bickler S et al (2015) Universities form research partnership to improve care in Mozambique. Bull Am Coll Surg 100:27–34. https://doi.org/10.1016/j.physbeh.2017.03.040 (PubMed PMID: 25626263)
Groen RS, Samai M, Stewart KA, Cassidy LD, Kamara TB, Yambasu SE et al (2012) Untreated surgical conditions in Sierra Leone: a cluster randomised, cross-sectional, countrywide survey. Lancet 380:1082–1087. https://doi.org/10.1016/S0140-6736(12)61081-2
Musolas A, Quinodoz P, Eriksen E, Mengiste A, Dumont L (2015) Severe skin contractures management: basic principles, pp 15–35. Epub Volume 1.
Baryza MJ, Baryza GA (1995) The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil 16(5):535–538. Epub 1995/09/01. https://doi.org/10.1097/00004630-199509000-00013. PubMed PMID: 8537427.
Nedelec B, Shankowsky HA, Tredget EE (2000) Rating the resolving hypertrophic scar: comparison of the Vancouver Scar Scale and scar volume. J Burn Care Rehabil 21(3):205–212. Epub 2000/06/13. https://doi.org/10.1067/mbc.2000.104750. PubMed PMID: 10850901.
Anderson JE, Erickson A, Funzamo C, Bendix P, Assane A, Rose J, Vaz F, Noormahomed EV, Bickler SW (2014). Surgical conditions account for the majority of admissions to three primary referral hospitals in rural Mozambique. World J Surg 38(4):823-829. https://doi.org/10.1007/s00268-013-2366-1
Forjuoh SN, Keyl PM, Diener-West M, Smith GS, Guyer B (1995) Prevalence and age-specific incidence of burns in Ghanaian children. J Trop Pediatr 41(5):273–277. Epub 1995/10/01. https://doi.org/10.1093/tropej/41.5.273. PubMed PMID: 8531257.
Gupta S, Ranjit A, Shrestha R, Wong EG, Robinson WC, Shrestha S et al (2014) Surgical needs of Nepal: pilot study of Population Based Survey in Pokhara. Nepal World J Surg 38(12):3041–3046. https://doi.org/10.1007/s00268-014-2753-2.PubMedPMID:WOS:000345103900002
Ademuyiwa AO, Odugbemi TO, Bode CO, Elebute OA, Alakaloko FM, Alabi EO et al (2019) Prevalence of surgically correctable conditions among children in a mixed urban-rural community in Nigeria using the SOSAS survey tool: Implications for paediatric surgical capacity-building. Plos One 14(10). ARTN e0223423. https://doi.org/10.1371/journal.pone.0223423. PubMed PMID: WOS:000532467000063.
Gupta S, Groen RS, Kyamanywa P, Ameh EA, Labib M, Clarke DL et al (2015 Surgical care needs of low-resource populations: an estimate of the prevalence of surgically treatable conditions and avoidable deaths in 48 countries. Lancet 385:1. PubMed PMID: WOS:000360573400002.
Bank TW (2019) Population, total—Mozambique: The World Bank Group; 2019 [cited 2022 January 20]. Available from: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=MZ.
Carini L, Grippaudo FR, Bartolini A (2005) Epidemiology of burns at the Italian Red Cross Hospital in Baghdad. Burns 31(6):687–691. Epub 2005/09/01. https://doi.org/10.1016/j.burns.2005.04.003. PubMed PMID: 16129222.
Subrahmanyam M (1996) Epidemiology of burns in a district hospital in western India. Burns 22(6):439–442. Epub 1996/09/01. https://doi.org/10.1016/0305-4179(96)00001-0. PubMed PMID: 8884001.
Groohi B, Alaghehbandan R, Lari AR (2002) Analysis of 1089 burn patients in province of Kurdistan, Iran. Burns 28(6):569–574. Epub 2002/09/11. https://doi.org/10.1016/s0305-4179(02)00099-2. PubMed PMID: 12220915.
Outwater AH, Van Braekel T (2019) Prehospital care of burn injuries in Africa: a review, 1990–2018. Burns, pp 1–9. https://doi.org/10.1016/j.burns.2019.08.009.
Botman M, Beijneveld JA, Negenborn VL, Hendriks TCC, Schoonmade LJ, Mackie DP et al (2019) Surgical burn care in sub-Saharan Africa: a systematic review. Burns Open 3:129–134. https://doi.org/10.1016/j.burnso.2019.07.001
Guzman KJ, Gemo N, Martins DB, Santos P, DeUgarte DA, Ademo F et al (2018) Current challenges of plastic surgical care in Sub-Saharan Africa (Maputo, Mozambique). Plastic and Reconstructive Surgery - Global Open 6:1–6. https://doi.org/10.1097/GOX.0000000000001893
Calland JF, Holland MC, Mwizerwa O, Petroze RT, Ntakiyiruta G, Patel K, et al. Burn management in sub-Saharan Africa: opportunities for implementation of dedicated training and development of specialty centers. Burns. 2014;40(1):157–63. Epub 2013/07/16. https://doi.org/10.1016/j.burns.2013.05.015. PubMed PMID: 23850364.
El Ezzi O, Dolci M, Dufour C, Bossou R, de Buys Roessingh A. Surgery on burns sequelae in developing countries. Ann Burns Fire Disasters. 2017;30(1):47–51. Epub 2017/06/09. PubMed PMID: 28592935; PubMed Central PMCID: PMCPMC5446909.
Hendriks TCC, Botman M, de Haas LEM, Mtui GS, Nuwass EQ, Jaspers MEH, et al. Burn scar contracture release surgery effectively improves functional range of motion, disability and quality of life: a pre/post cohort study with long-term follow-up in a Low- and Middle-Income Country. Burns. 2021;47(6):1285–94. Epub 2021/01/25. https://doi.org/10.1016/j.burns.2020.12.024. PubMed PMID: 33485727.
Acknowledgements
This research was supported by grant number R24TW008910 (MEPI linked surgery) from the Fogarty International Center. Additional support was obtained from the UCSD Hispanic Center of Excellence to complete the data analysis and develop the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Fogarty International Center, the NIH, or the University of California Global Health Institute.
Funding
This research was supported by grants from the Fogarty International Center (R24TW008910 and R25TW011216), the Fogarty International Clinical Research Scholars and Fellows Program (R24 TW007988), and a Fogarty International Center Research Training Grant (R25TW009343) through the University of California Global Health Institute.
Author information
Authors and Affiliations
Contributions
PB, DN, AG, and SWB conceptualized this article. JR, PB, MC, FA, FV, CF, VA, DN, and EN assisted in the study design and data gathering. PB, DN, MH, and CT accessed the study data and determined photograph viability. PB drafted the first version of the Article. AG, SWB, JS, MH, DN, PB, CT, EE, and SL made major contributions to the analysis and interpretation of the data. All authors read and met the ICMJE criteria for authorship and agree with the results and conclusions. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflicts of interests.
Ethics approval
This research was approved by the University of California San Diego Human Research Protection Program and the National Bioethics Committee in Mozambique.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barba, P., Neubauer, D.C., Cossa, M. et al. Prevalence and Severity of Burn Scars in Rural Mozambique. World J Surg 46, 2561–2569 (2022). https://doi.org/10.1007/s00268-022-06682-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06682-y