Abstract
Background
Neuroendocrine neoplasia (NEN) are rare and complex, with surgery as key therapy even in cases with metastasis. Little is known regarding the quality of life, prevalence of depression, anxiety and the impact of surgery.
Methods
This prospective, follow-up study included 90 consecutively recruited patients with NEN after surgery in a university hospital. The EORTC QLQ-C30, EORTC QLQ-GI-NET.21, and Hospital Anxiety and Depression Scale and a hospital specific questionnaire were completed during follow-up after 3 to 5 years (t1–t5).
Results
Mean age was 54 (SD 15) years, 13% had secondary malignancies and 11% had psychiatric diagnoses (depression n = 8, schizophrenia n = 2) pre-existent. Critical life events occurred in 51% within 5 years before diagnosis. Surgery was done in curative intention in 82% and R0-resection rate was 90%. The median survival was 25.3 years. The 10-year survival rate was 87%, 98%, 95% and 26% for all patients (n = 90), stage I/II (n = 45), stage III (n = 25) and stage IV (n = 20), respectively (p < .001). Anxiety score was pathological in 30% after 1 year (t1) and in 10% after 5 years, depression score in 25% (t1) and 30% (t5). Fatigue and muscle/body pain were elevated symptoms with > 50 and 40 points 3 years after surgery.
Conclusion
Depression rate remains high whereas anxiety declines over time. Fatigue and muscle/body pain were identified as relevantly elevated after surgery. Systematic screening and supportive therapy should be implemented during follow-up after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasia (NEN) of the gastrointestinal tract are a rare and heterogeneous tumour entity with estimated incidence of 4–6/100,000 per year. Survival rates are high even in metastatic disease resulting in a prevalence of 35/100,000 per year [1]. Median age at diagnosis is in the sixth decade although many patients with inherited syndromes are younger. Around 50% of the patients have distant metastases at time of diagnosis and up to 80% show locoregional lymph node metastases [2, 3]. Surgery is the key therapeutic option even in the presence of distant metastases and so far the only curative treatment. According to data of the German NET-Registry, surgery is applied up to the sixth line therapy along a NEN-patient career [2, 4]. Prognostic factors are tumour stage at diagnosis, primary localisation and tumour grading, dependent on Ki-67%, according to ENETS-proposal [5,6,7]. Since 2009 the TNM-classification for NEN was adopted to the ENETS-proposal and leaded to a practicable and widely accepted classification system [8,9,10].
Many NEN are slow-growing, chemotherapy-resistant G1- or G2-NET with a proliferation-index of Ki-67 < 20%. Even after complete and curative tumour resection a risk of recurrence remains. Tumour recurrences can occur even 10 to 20 years after curative resection [11, 12].
Functional activity is seen in around 20% of NEN-patients, most often carcinoid syndrome due to systemic hypersecretion of serotonin in case of hepatic metastases of GI and pulmonal NEN [13]. Psychiatric dysbalances like depressivity and sleeping disorders are described in 3–10% of the patients with carcinoid syndrome [14]. The serotonin-synthesis of functional active NEN may result in a tryptophan deficiency. Tryptophan is an essential amino-acid, which is generally converted into niacin and the precursor of multiple bioactive products. It is estimated that up to 60% of the resorpted dietary tryptophan may be consumed in case of small bowel NEN by the neoplasia itself [15, 16]. Deficiency of essential amino acids might influence the psychological status of the patients as well [17, 18]. The role of the central serotonergic system is not fully understood, yet the dysfunction of this system is associated with depression, anxiety, sleeping disorders, impaired social and cognitive function [19, 20]. Depression and anxiety are a major issue in cancer patients and can affect the immune system [21, 22]. This results in an impaired immune response by modulating the secretion of pro-inflammatory cytokines and thereby the response to infections and tumour response [23,24,25].
So, several mechanisms which influence quality of life, depression and anxiety are possible in NEN: these are long-term effects of surgery, lifelong tumour burden, danger of recurrence and possibly the lack and deficiency of essential amino acids in functional active NEN [16]. While data for quality of life (QoL) exist for advanced NEN from clinical studies, no data exists for NEN treated with surgery in curative intention [26, 27]. Aim of this study was to elucidate 1. The prevalence of pre-existent psychiatric comorbidities and 2. To describe anxiety, depression and quality of life in a surgically treated cohort of NEN-patients.
Materials and methods
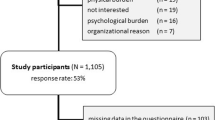
Patients for this study were consecutively recruited after surgery for NEN in the department for surgery at the university hospital Schleswig–Holstein (UKSH), Campus Luebeck, at the first follow-up visit after surgery in the outpatient clinic. Recruitment period was from 01/2009 to 12/2015. All patients had to give written consent for participation in the local NEN registry. Recruitment started within 3 month after surgery to reduce bias driven by anxiety and excitement before surgery and study questionnaire was completed at each further follow-up visit. The study questionnaire included questions on clinical aspects, sociodemographic data and validated questionnaires for assessing anxiety and depression (HADS-D) and health-related quality of life (EORTC QLQ-C30) and since 2012 EORTC QLQ-Gi.NET 21. The third battery of hospital specific questionnaires included questions on important life events (such as death of a beloved, divorce, serious diseases), on additional cancer treatment (radio-, / chemo-, immunotherapy), use of complementary alternative medicine and on psychological support (psychotherapy, patient groups). Time periods were defined as t1 = 3–12 month, t2 = 13–24 month, t3 = 25–36 month, t4 > 36 and t5 > 60 month after surgery. For HADS-D t1 to t5 are available, for EORTC QLQ-C30 and GI.NET 21 t1–t3 is available only, because this questionnaires were introduced later.
Hads-D
The German version of the Hospital Anxiety and Depression Scale (HADS-D) consists of 14 items in total, of which each seven are grouped to the subscales anxiety and depression. The four possible answers per item are coded zero (absence of problem) to three (most severe problem); thus, the subscale scores range from zero to 21. The higher the score, the higher is the level of anxiety and depression. A score of eight to ten indicates at least borderline anxiety, a score over 10 a manifest anxiety and depression [28].
EORTC QLQ-C30 and EORTC QLQ-GINET21
The QLQ-C30 consists of 30 items covering five function subscales (physical, role, emotional, cognitive, social function C30), nine symptom subscales/items (fatigue, nausea/vomiting, pain, dyspnoea, insomnia, appetite loss, constipation, diarrhoea, financial difficulties) and a global health/QoL subscale [29]. The GINET21 includes 21 items covering four single-item assessments relating to muscle and/or bone pain (MBP), body image (BI), information (INF) and sexual functioning (SX) as well as 17 items organised into five symptom scales: endocrine symptoms (ED; 3 items), GI symptoms (GI; 5 items), treatment-related symptoms (TR; 3 items), and disease-related worries (DRW; 3 items) and one function scale (social function GINET21/SF21, 3 items) [29, 30]. With the exception of the last two questions of the QLQ-C30 (7-point Likert scale) all questions are answered on a 4-point Likert scale (ranging from “not at all” to “very much”).
According to the guidelines provided by the EORTC, all scores of the QLQ-C30 and -GINET21 were transformed linearly so that all scales range from 0 to 100. In the function scales, higher scores represents a better level of functioning. While in the symptom scales/items, a higher score marks a worsening of the symptoms [29].
Statistics
For the purpose of this analysis, follow-up data derived by 141 follow-up questionnaires were grouped into five groups: Follow-up visit within 12 months after surgery (t1, n = 52 patients), within 13–24 months (t2, n = 33 patients), within 25–36 months (t3, n = 21 patients), within 37 to 60 months (t4, n = 11 patients) and more than 60 months after surgery (t5, n = 24 patients). Standard descriptive statistic measures were used to describe the study population and subgroups in regard to clinical and sociodemographic data and the QoL measures. Survival analysis was conducted using the Kaplan–Meier method, differences between survival curves were tested with the log-rank test. A p value of < 0.05 was considered as statistically significant.
Ethics
All patients provided written informed consent prior to study participation. Ethical approval was achieved for the local NET-registry including the questionnaire-based interrogation by the Ethic committee of the university.
Results
The study cohort (n = 90) consisted of 43 females and 47 males, which were selected consecutively at time of the first postoperative visit in the outpatient clinic of the department for surgery, which was usually scheduled within the first 3 month after surgery (Table 1). For preoperative symptoms and comorbidities see figure (Figs. 1 and 2).
Tumour stage
In 45 cases no locoregional lymph node or distant metastases were seen, so this patients were grouped stage I and II, 25 patients had positive locoregional lymph node metastases without distant metastases (stage III) and 20 patients had distant metastases (stage IV). For localization of the metastases, see Fig. 3a.
a Site of metastases, lymph node metastases were locoregional b A histological tumour free resection margin (R0) was seen in 81 patients, one patient with CUP had a macroscopic residual tumour (R2), in another patient with CUP complete tumour resection was performed, but the primary was not detected, so this patient was classified RX, in 7 patients no data concerning resection margin were available
Intention of surgery and rate of complete tumour resection
All included patients received an operative procedure, which was in curative intention in 74 (82%) and in palliative intention in 16 (18%) patients. In one case of the palliative group, a diagnostic laparoscopy without resection was performed and in seven cases a complete tumour resection with histological tumour free margin was achieved in this group with initially palliative intention (Fig. 3b). The operative procedures are seen in Fig. 4.
Tumour grading and survival
For grading see Fig. 5. The 5- and 10-year survival rate (ysr) were 93 and 87% for all patients. In nodal negative NEN (tumour stage I/II, n = 45), 5- and 10-ysr were 98%. In nodal positive NEN (stage III, n = 25) 5- and 10-ysr were both 95%. In distant metastases 5- and 10-ysr were 79 and 26.5% (n = 20, p = 0.01, Fig. 6).
Complications after surgery
Postoperative complications were seen in 37 of the patients (41%), in 3 cases a major complication with operative revision and in 34 patients minor-complications were seen (Table 2).
Perisurgical and additional therapy
One patient received a platinum-based chemotherapy before surgery for a high grade gastric cancer, initially misdiagnosed as adenocarcinoma. Seventy-four patients had no other therapy after surgery, 16 patients had a further therapy. Information on additional treatment and support were provided by 51 (t1: < 13 months), 33 (t2: 13–24 months) and 21 (t3: 25–36 months after diagnosis) patients, respectively (Fig. 7).
Critical life events
Critical life events within 5 years before the diagnosis of NEN were reported by a total of 61 patients (Fig. 8).
Hads-D
HADS-D was completed 129 times. Pathological scores for anxiety (> 10 points) increased from 20% at t1 to 30% at t2 and decreased to 10% at t5 (5 years after surgery). Pathological scores for depression (> 8 points) increased from 25% at t1 to 28% at t2 and remained stable with 30% at t5, i.e. 5 years after treatment (Fig. 9).
EORTC QLQ-C30 and -GI-NET.21
For the EORTC QLQ-C30 and GI-NET.21 symptom scales a value of 0 means best (i.e. the absence of symptoms), 100 means worst symptoms. In the function scale 0 means worst, 100 means best function, a relevant difference is seen with 10 points difference.
EORTC QLQ-C30 is available 44 × at t1, 23 × at t2 and 14 × at t3.
The six function domains are global quality of life/health status, physical role, emotional, cognitive and social function. Scores on all function domains decreased between t1 and t3, with the exception of cognitive and social function (C30) for which scores at t3 are higher than at t2. For the latter the highest score of nearly 80 points, and thus highest social function, is reached 25–36 months after surgery. Emotional and cognitive function showed a decrease of more than 10 points, which means a clinical worsening (Fig. 10).
The nine symptom items/scales in the QLQ-C30 questionnaire were fatigue, pain, dyspnoea, diarrhoea, nausea and vomiting, constipation, loss of appetite, sleep and financial difficulties. Fatigue, pain, dyspnoea, appetite loss and diarrhoea are among the symptoms that were considered most troublesome as indicated by high scores. An initial increase (between t1 and t2), but a further decrease in symptoms (between t2 and t3) is observed for nausea and vomiting, sleep, constipation and diarrhoea. Fatigue seem to increase in a clinical relevant manner from t1 to t3 and remains high with > 50 points (Fig. 10).
According GI-NET.21 social function showed the same level at all time points with scores around 50. A high level of bother as indicated by scores > 40 points was observed for muscle and/or body pain at t3 and disease-related worries at all time points. Clinical relevant changes were seen for muscle and/or body pain (increase in symptoms) and body image (decrease in symptoms, Fig. 10).
Discussion
Little is known about how patients with neuroendocrine neoplasia deal with the demanding situation caused by the disease with its risk for late tumour recurrence followed by multimodal treatment after surgery. These are the first long-term data for QoL over 3 years after surgery in a mostly curatively treated cohort of NEN-patients as in 81/90 patients a complete tumour resection (R0) was achieved. In general, we see a stabilization of all functions and a decrease in symptoms over time. For endocrine, gastrointestinal and treatment-related symptoms we find ranges between 10 and 30 points 3 years after surgery, which means nearly normal situation. Fatigue shows an increasing with > 50 points and muscle/body pain with > 40 points after 3 years, so patients should be monitored for this even after curative treatment. Possible bias are the high rate of G1/G2 tumours (88%) and the low rate of G3-NEC (12%) resulting in high 10-years-survival rates (98, 95 and 79% for stage I/stage II, stage III, stage IV). The impact of distant metastases at time of diagnosis is seen after 10 years with a survival rate of 26%, only (p < 0.001, Fig. 6). Another limitation of our study is, that we did not differ the outcome of the questionnaires between patients with and without tumour persistence or tumour recurrence. Another limitation of our study is the lacking comparison group, which could be other cancer survivors like colorectal carcinoma. More homogeneous groups and a possible influence of gender should be analysed in the future studies.
Quality of life
Watson et al. published a systematic literature review concerning QoL in NEN-patients: 43 publications were eligible: 8 in GI-NET only and 6 studies in pancreatic NEN. Most commonly, EORTC-QoL-C30 was used, 6 studies used the additional battery of GI-NET21. Not surprisingly, there was no surgical cohort and the result was, there was no difference between placebo and treatment arm (biotherapy, chemotherapy, molecular-targeted therapy and PRRT) within 12 month except in the NETTER-1-study, in which the active treatment improved QoL [31, 32]. Milanetto et al. published a study with 100 patients with Si-NET after surgery and found male gender, younger age, treatment with Somatostatin analogues, non-symptomatic tumour and small intestinal surgery associated with better quality of life [33]. Karpinnen et al. studied QoL in 134 SI-NEN-patients with SF-36 and 15D and compared this to the general Swedish population (n = 1153). The study population differed from our concerning primary (SI only), 91% had a metastatic situation, around 79% received biotherapy (SSTRA). They found an overall impairment, especially for diarrhoea, sleep, depression, vitality and sexual activity. Interestingly, they found a correlation with number of medication and a high prevalence of depression in carcinoid syndrome with 35–50% [34].
According to Larsson et al. patients with endocrine GI tumours enjoy a relatively good quality of life, which we could not find in our cohort [35]. Compared to the data of the EORTC QLQ-C30 of the German population the NEN-patients have worse function and aggravation of symptoms in nearly every domain [36]. The impairment of QoL was lasting during the follow-up period and showed no tendency towards normalization. Scores on all functional domains decreased over 3 years after surgery, representing a worsening of function. Fatigue is a general problem in patients with cancer diagnoses [35]. According to Bower et al. approximately 20% of the cancer survivors report persistent fatigue after curative treatment, which we find in our cohort, too [37]. It is noteworthy that this remains a problem in a patient cohort of which 90% had a curative tumour resection.
Anxiety and depression
The prevalence of psychiatric disorders at time of diagnoses in NEN in our cohort is high with 12% (10/90) but comparable to other cancer cohorts such as breast cancer. History of major depression in a small series of breast cancer patients was reported in 10% [38]. Zhu et al. found in only 4.49% of cancer patients previous mental disorder in a Swedish population of 218.000 cancer patients. The cancer stage was comparable to our group with advanced stages only in 8% [23]. According to Mitchell et al. the rate of depression is 2–4 times higher in cancer patients compared to normal population [39]. They found around 30–50% of patients in cancer suffering from psychiatric disorders. The rate of anxiety and depression according to HADS-D was high in the postsurgical period. Anxiety shows the tendency towards normalization, but scores for depression remain high with 30% during follow-up. Lewis et al. found a pathological anxiety score (> 8/21) in 26% and a pathological depression score (> 8/21) in 10% in a group of 50 patients with advanced NEN [40]. The history of major depressive disorder is a general risk factor for poor psychological adjustment to stress, including a cancer diagnosis and may also influence cancer-related fatigue and outcome [37, 41] Sleep disturbance is common in cancer patients and survivors and is strongly correlated with fatigue, too [42].
The rate of critical lifetime events seems to be very high within 5 years before diagnosis of NEN. So far, there is no known causality between this and the onset of diagnoses of NEN. But further studies with comparative groups are needed to shed light on this finding.
Conclusion
Quality of life in patients with NEN in a group with high rate of curation remains stable after surgery and shows no tendency to worsening within 3 years of follow-up. Fatigue and muscle/body pain remain symptoms with clinical relevance, though. Anxiety decreases over time, but the rate of depression remains high with 30% in our cohort. Studies with focus on the long-term effects of surgery in this complex patient group are necessary. As depression and psychiatric disorders can reduce cancer survival due to different reason, a clinical focus should be on diagnosing the patients at risk and refer them to further treatment. HADS-D is an appropriate instrument in NEN-patients for screening for anxiety and depression and should be implemented into the follow-up even after curative resection. The authors see an urgent need for monitoring quality of life and mental health as important clinical oncological issue also in a surgical cohort.
References
Öberg K, Knigge U, Kwekkeboom D et al (2012) ESMO guidelines working group neuroendocrine gastro-entero-pancreatic tumours: ESMO clinical practice guidelines for diagnosis treatment and follow-up. Ann Oncol 23(Suppl 7):124–130
Begum N, Maasberg S, Plöckinger U et al (2014) Neuroendocrine tumours of the GI tract–data from the German NET registry. Zentralbl Chir 139:276–283
Yao JC, Hassan M, Phan A et al (2008) One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumours in 35,825 cases in the United States. J Clin Oncol 26:3063–3072
Jann H, Roll S, Couvelard A et al (2011) Neuroendocrine tumours of midgut and hindgut origin: tumour-node-metastasis classification determines clinical outcome. Cancer 117(15):3332–3341
Pape UF, Bohmig M, Berndt U et al (2004) Survival and clinical outcome of patients with neuroendocrine tumours of the gastroenteropancreatic tract in a German referral center. Ann N Y Acad Sci 1014:222–233
Rindi G, Klöppel G, Alhman H et al (2006) TNM-staging of foregut (neuro)endocrine tumours: a consensus proposal including a grading system. Virchows Arch 449(4):395–401
Rindi G, Klöppel G, Couvelard A et al (2007) TNM staging of midgut and hindgut (neuro)endocrine tumours: a consensus proposal including a grading system. Virchows Arch 451(4):757–762
Sobin LH, Gospodarowicz MK, Wittekind C (2009) In: TNM classification of malignant tumours, 7th edn. Wiley, Hoboken
Lloyd RF, Osamura RY, Klöppel G et al (2017) In: WHO classification of tumours of endocrine organs, 4th edn. IARC, Lyon
Board Editorial (2019) In: WHO classification of tumours: digestive system tumours, 5th edn. IARC, Lyon
Frilling A, Sotiropoulos GC, Li J et al (2010) Multimodal management of neuroendocrine liver metastases. HPB (Oxford) 6:361–379
Begum N, Maasberg S, Pascher A et al (2020) Long-term outcome of surgical resection in patients with gastroenteropancreatic neuroendocrine neoplasia: results from a German nation-wide multi-centric registry. Langenbecks Arch Surg 405(2):145–154
Rosenbaum FF, Santer DG, Claudon DB (1953) Essential telangiectasia, pulmonic and tricuspid stenosis, and neoplastic liver disease, a possible new clinical syndrome. J Lab Clin Med 42:941
Schott M, Wiedenmann B, Plöckinger U (2014) Neuroendokrine tumoren des mitteldarms. In: Lehnert H, Anlauf M, Herausgeber (eds) Rationelle diagnostik und therapie in endokrinologie diabetologie und stoffwechsel, 4th edn. Thieme, Stuttgart, pp 212–25
Russo S, Nielen MM, Boon JC et al (2003) Neuropsychological investigation into the carcinoid syndrome. Psychopharmacology 168:324–328
Pasieka JL, Longman RS, Chambers AJ et al (2014) Cognitive impairment associated with carcinoid syndrome. Ann of Surg 259(2):355–359
Shah GM, Shah RG, Veillette H et al (2005) Biochemical assessment of niacin deficiency among carcinoid cancer patients. Am J Gastroenterol 100:2307–2314
Mendelsohn D, Riedel WJ, Sambeth A (2009) Effects of acute tryptophan depletion on memory, attention and executive functions: a systematic review. Neurosci Biobehav Rev 33:926–952
Frojd C, Larsson G, Lampic C et al (2007) Health related quality of life and psychosocial function among patients with carcinoid tumours, a longitudinal, prospective, and comparative study. Health Qual Life Outcomes 5(18):1–9
Trivedi S (1984) Psychiatric symptoms in carcinoid syndrome. J Indian Med Assoc 82:292–294
Walker J, Hansen CH, Martin P et al (2014) Prevalence, associations, and adequacy of treatment of major depression in patients with cancer: a cross-sectional analysis of routinely collected clinical data. Lancet Psychiat 5:343–350
Lee SA, Nam CM, Kim YH et al (2020) Impact of onset of psychiatric disorders and psychiatric treatment on mortality among patients with cancer. Oncologist 25(4):e733–e742
Zhu J, Sjölander A, Fall K et al (2018) Mental disorders around cancer diagnosis and increased hospital admission rate-a nationwide cohort study of Swedish cancer patients. BMC Cancer 18:322
Kiecolt-Glaser JK, Marucha PT, Malarkey WB et al (1995) Slowing of wound healing by psychological stress. Lancet 346(8984):1194–1196
Rojas IG, Padgett DA, Sheridan JF et al (2002) Stress-induced susceptibility to bacterial infection during cutaneous wound healing. Brain Behav Immun 16(1):74–84
Strosberg J, Wolin E, Chasen B et al (2018) Health-related quality of life in patients with progressive midgut neuroendocrine tumours treated with 177 Lu-dotatate in the phase III NETTER-1 trial. JCO 36(25):2578–2584
Cella D, Beaumont JL, Hudgens S et al (2018) Relationship between symptoms and health-related quality-of-life benefits in patients with carcinoid syndrome: post hoc analyses from TELESTAR. Clin Ther 40(12):2006–2220
Hermann C, Buss U, Snaith RP (1995) In: HADS-D hospital anxiety and depression scale–German version. Verlag Hans Huber, Bern
Fayers PM, Aaronson NK, Bjordal K et al (2001) The EORTC QLQ–C30 scoring manual. In: Fayers PM, Aaronson NK, Bjordal K et al (eds) European organization for rese arch and treatment of cancer, 3rd edn. Brussels
Davies AH, Larsson G, Ardill J et al (2006) EORTC quality of life group: development of a disease-specific quality of life questionnaire module for patients with gastrointestinal neuroendocrine tumours. Eur J Cancer 42(4):477–484
Yadegarfar G, Friend L, Jones L et al (2013) Validation of the EORTC QLS-GINET21 questionnaire for assessing quality of life of patients with gastrointestinal neuroendocrine tumours. Br J Cancer 108:301–310
Watson C, Tallentire CW, Ramage JK et al (2020) Quality of life in patients with gastroenteropancreatic tumours: a systematic literature review. World J Gastroenterol 26(25):3686–3711
Milanetto AC, Nordenström E, Sundlöv A, Almquist M (2018) Health-Related quality of life after surgery for small intestinal neuroendocrine tumours. World J Surg 42(10):3231–3239. https://doi.org/10.1007/s00268-018-4638-2
Karppinen N, Lindén R, Sintonen H et al (2018) Health-Related quality of life in patients with small intestine neuroendocrine tumours. Neuroendocrinology 107:366–374
Larsson G, Sjoden PO, Öberg K et al (2001) Health-related quality of life, anxiety and depression in patients with midgut carcinoid tumours. Acta Oncol 40:825–831
Nolte S, Waldmann A, Liegle G et al (2020) Updated EORTC QLQ-C30 general population normdata for Germany. Eur J Cancer 138:161–170
Bower JE (2019) The role of neuro-immune interactions in cancer-related fatigue: biobehavioral risk factors and mechanisms. Cancer 125(3):353–364
Broeckel JA, Jacobsen PB, Horton J et al (1998) Characteristics and correlates of fatigue after adjuvant chemotherapy for breast cancer. J Clin Oncol 16(5):1689–1696
Mitchell AJ, Chan M, Bhatti H et al (2011) Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol 12:160–174
Lewis AR, Wang X, Magdalani L et al (2018) Health-related quality of life, anxiety, depression and impulsivity in patients with advanced gastroenteropancreatic neuroendocrine tumours. World J Gastroenterol 24(6):671–679
Stanton AL, Bower JE (2015) Psychological adjustment in breast cancer survivors. Adv Exp Med Biol 862:231–242
Ancoli-Israel S, Liu L, Rissling M et al (2014) Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: a 1-year longitudinal study. Supp Care Cancer 22(9):2535–2545
Acknowledgements
We thank Mrs. Claudia Killaitis and Mrs. Dana Varbelow from the Department for General Surgery of the University hospital Schleswig-Holstein (UKSH), Campus Lübeck, for their great effort concerning the maintenance of the data bank.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Informed consent
Informed consent were received for all patients contributing to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Begum, N., Hunold, H., Gerdes, B. et al. Anxiety, Depression and Quality of Life in Patients with Neuroendocrine Neoplasia After Surgery. World J Surg 46, 1408–1419 (2022). https://doi.org/10.1007/s00268-022-06479-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06479-z