Abstract
Background
Preoperative malnutrition is believed to contribute to increased postoperative complications. Preoperative serum prealbumin level was reported to be a predictor of nutritional status and postoperative complications after gastrointestinal surgery, including gastrectomy. Gastric outlet obstruction caused by gastric cancer leads to insufficient nutritional status. However, the impact of preoperative enteral nutrition using naso-jejunal feeding tubes for patients with gastric outlet obstruction is not fully understood.
Methods
From July 2010 to June 2020, 50 patients with gastric cancer-induced outlet obstruction who underwent gastrectomy following preoperative enteral nutrition via feeding tube were included. We investigated the relationship between changes in nutritional status after preoperative enteral nutrition and postoperative complications. Postoperative complications were defined as grade ≥II based on the Clavien–Dindo classification.
Results
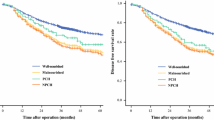
The median period of preoperative enteral nutrition was 10 days. The median increase rate of the serum prealbumin level was 10.5% (interquartile range, 0.63–38.2%), and patients with an increase rate ≥ 10% were defined as the elevated group. Postoperative morbidity was significantly higher in the non-elevated group (P = 0.0031). Univariate and multivariate analyses showed that an increased rate of the serum prealbumin level was an independent risk factor of postoperative complications for patients with gastric outlet obstruction caused by gastric cancer (P = 0.0025 and P = 0.009, respectively).
Conclusions
Preoperative enteral nutrition improved the serum prealbumin level of patients with gastric cancer-induced outlet obstruction, and an increased rate of prealbumin can be an indicator of sufficient preoperative enteral nutrition and decreased postoperative morbidity.


Similar content being viewed by others
Data availability
All data associated with this study.
References
Arends J, Baracos V, Bertz H et al (2017) ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr 36(5):1187–1196
Adiamah A, Skorepa P, Weimann A et al (2019) The impact of preoperative immune modulating nutrition on outcomes in patients undergoing surgery for gastrointestinal cancer: a systematic review and meta-analysis. Ann Surg 270(2):247–256
Weimann A, Braga M, Carli F et al (2017) ESPEN guideline: clinical nutrition in surgery. Clin Nutr 36(3):623–650
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 71(3):209–249
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Society AC (2017) Cancer Facts & Figures 2017
Johnson CD, Ellis H (1990) Gastric outlet obstruction now predicts malignancy. Br J Surg 77(9):1023–1024
Shetty PS, Watrasiewicz KE, Jung RT et al (1979) Rapid-turnover transport proteins: an index of subclinical protein-energy malnutrition. Lancet 2(8136):230–232
Zhou J, Hiki N, Mine S et al (2017) Role of prealbumin as a powerful and simple index for predicting postoperative complications after gastric cancer surgery. Ann Surg Oncol 24(2):510–517
Japanese Gastric Cancer A (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 14(2): 101–12
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Katayama H, Kurokawa Y, Nakamura K et al (2016) Extended Clavien-Dindo classification of surgical complications: Japan clinical oncology group postoperative complications criteria. Surg Today 46(6):668–685
Consultation WHOE (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363(9403):157–163
Gakuhara A, Fukuda S, Tsujimoto T et al (2020) Successful management of gastric remnant necrosis after proximal gastrectomy using a double elementary diet tube: a case report. Surg Case Rep 6(1):296
Wada T, Takeuchi H, Yoshikawa T et al (2014) Successful management of anastomotic leakage and lung fistula after esophagectomy. Ann Thorac Surg 97(3):1071–1073
Fujitani K, Tsujinaka T, Fujita J et al (2012) Prospective randomized trial of preoperative enteral immunonutrition followed by elective total gastrectomy for gastric cancer. Br J Surg 99(5):621–629
Zheng Y, Li F, Qi B et al (2007) Application of perioperative immunonutrition for gastrointestinal surgery: a meta-analysis of randomized controlled trials. Asia Pac J Clin Nutr 16(Suppl 1):253–257
Saito M, Seo Y, Yano Y et al (2012) Short-term reductions in non-protein respiratory quotient and prealbumin can be associated with the long-term deterioration of liver function after transcatheter arterial chemoembolization in patients with hepatocellular carcinoma. J Gastroenterol 47(6):704–714
Devoto G, Gallo F, Marchello C et al (2006) Prealbumin serum concentrations as a useful tool in the assessment of malnutrition in hospitalized patients. Clin Chem 52(12):2281–2285
Mantovani A, Allavena P, Sica A et al (2008) Cancer-related inflammation. Nature 454(7203):436–444
Keller U (2019) Nutritional Laboratory Markers in Malnutrition. J Clin Med. 8(6):775
Fearon K, Strasser F, Anker SD et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12(5):489–495
Toiyama Y, Miki C, Inoue Y et al (2011) Evaluation of an inflammation-based prognostic score for the identification of patients requiring postoperative adjuvant chemotherapy for stage II colorectal cancer. Exp Ther Med 2(1):95–101
McMillan DC (2009) Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 12(3):223–226
Bickenbach KA, Denton B, Gonen M et al (2013) Impact of obesity on perioperative complications and long-term survival of patients with gastric cancer. Ann Surg Oncol 20(3):780–787
Acknowledgements
We would like to thank Preethi Ravindranathan for a critical reading of the manuscript. We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
DI, SI, and SN contributed to study concept and design; DI, SI, RM, KK, MW, TS, and SN were specimen providers; DI, SI, MH, RM, KK, MW, TS, and SN contributed to acquisition of clinical data; DI, SI, and SN performed analysis and interpretation of data, statistical analysis, and drafting of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests for this article.
Informed consent
The protocol for this research project has been approved by a suitably constituted Ethics Committee of the institution and it conforms to the provisions of the Declaration of Helsinki. Committee of the Cancer Institute Hospital of the Japanese Foundation for Cancer Research, Approval No. 2017–1029. All informed consent was obtained from the subjects or guardians.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Izumi, D., Ida, S., Hayami, M. et al. Increased Rate of Serum Prealbumin Level after Preoperative Enteral Nutrition as an Indicator of Morbidity in Gastrectomy for Gastric Cancer with Outlet Obstruction. World J Surg 46, 624–630 (2022). https://doi.org/10.1007/s00268-021-06384-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06384-x