Abstract
Background
Splenectomy for proximal gastric cancer was found to have no survival benefit in a randomized trial clarifying the role of splenectomy (JCOG0110 study). However, since tumor with invasion to the greater curvature and Type 4 tumor were excluded in JCOG0110, the benefit of splenectomy for these tumors is not known.
Methods
A multicenter dataset of patients with gastric cancer who underwent gastrectomy between 2010 and 2014 was created. From the dataset, 114 eligible patients with proximal advanced gastric cancer with invasion to the greater curvature or Type 4 tumor were enrolled. There were 60 patients in the gastrectomy with splenectomy (Spx) group and 54 patients in the spleen-preserving (Prs) group. To balance the essential variables, propensity score analysis was performed, estimating the propensity score with a logistic regression model. Adjusted overall survival (OS) and adjusted disease-free survival (DFS) were estimated using the inverse probability of treatment weighting (IPTW) method.
Results
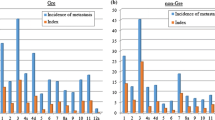
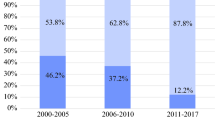
There were significant differences in age, performance status, comorbidity, macroscopic type, and clinical T stage between the Spx and Prs groups. The model for estimating the propensity score was well adapted (c-statistic: 0.830, 95%CI: 0.754–0.906). Adjusted OS was identical between the two groups (HR = 1.089, 95%CI: 0.759–1.563; p = 0.644). The DFS curve of Prs group was consistently tended to be lower than Spx, but the difference was not significant (HR = 0.813, 95%CI: 0.572–1.156; p = 0.249).
Conclusions
The efficacy of splenectomy was minimal for proximal advanced gastric cancer even with invasion to the greater curvature or Type 4 tumor.



Similar content being viewed by others
References
Chen XL, Yang K, Zhang WH et al (2014) Metastasis, risk factors and prognostic significance of splenic hilar lymph nodes in gastric adenocarcinoma. PLoS One 9:e99650
Hong ZL, Chen QY, Zheng CH et al (2017) A preoperative scoring system to predict the risk of No.10 lymph node metastasis for advanced upper gastric cancer: a large case report based on a single-center study. Oncotarget 8:80050–80060
Huang CM, Zhang JR, Zheng CH et al (2014) A 346 case analysis for laparoscopic spleen-preserving no 10 lymph node dissection for proximal gastric cancer: a single center study. PLoS One 9:108480
Jeong O, Jung MR, Ryu SY (2019) Clinicopathological features and prognostic impact of splenic hilar lymph node metastasis in proximal gastric carcinoma. Eur J Surg Oncol 45:432–438
Kosuga T, Ichikawa D, Okamoto K et al (2011) Survival benefits from splenic hilar lymph node dissection by splenectomy in gastric cancer patients: relative comparison of the benefits in subgroups of patients. Gastric Cancer 14:172–177
Sasada S, Ninomiya M, Nishizaki M et al (2009) Frequency of lymph node metastasis to the splenic hilus and effect of splenectomy in proximal gastric cancer. Anticancer Res 29:3347–3351
Shin SH, Jung H, Choi SH et al (2009) Clinical significance of splenic hilar lymph node metastasis in proximal gastric cancer. Ann Surg Oncol 16:1304–1309
National Comprehensive Cancer Network Gastric Cancer (Version 3.2020)
Yu W, Choi GS, Chung HY (2006) Randomized clinical trial of splenectomy versus splenic preservation in patients with proximal gastric cancer. Br J Surg 93:559–563
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Sano T, Sasako M, Mizusawa J et al (2017) Randomized controlled trial to evaluate splenectomy in total gastrectomy for proximal gastric carcinoma. Ann Surg 265:277–283
Japanese Gastric Cancer Association (2020) Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 24:1–21
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14:101–112
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Cole SR, Hernan MA (2004) Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed 75:45–49
Xie J, Liu C (2005) Adjusted Kaplan-Meier estimator and log-rank test with inverse probability of treatment weighting for survival data. Stat Med 24:3089–3110
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424
Thomas L, Li F, Pencina M (2020) Using propensity score methods to create target populations in observational clinical research. JAMA 323:466–467
Csendes A, Burdiles P, Rojas J et al (2002) A prospective randomized study comparing D2 total gastrectomy versus D2 total gastrectomy plus splenectomy in 187 patients with gastric carcinoma. Surgery 131:401–407
Yang K, Chen XZ, Hu JK et al (2009) Effectiveness and safety of splenectomy for gastric carcinoma: a meta-analysis. World J Gastroenterol 15:5352–5359
Ohkura Y, Haruta S, Shindoh J et al (2017) Efficacy of prophylactic splenectomy for proximal advanced gastric cancer invading greater curvature. World J Surg Oncol 15:106
Kikuchi H, Miyata H, Konno H et al (2017) Development and external validation of preoperative risk models for operative morbidities after total gastrectomy using a Japanese web-based nationwide registry. Gastric Cancer 20:987–997
Sasako M, McCulloch P, Kinoshita T et al (1995) New method to evaluate the therapeutic value of lymph node dissection for gastric cancer. Br J Surg 82:346–351
Watanabe M, Kinoshita T, Enomoto N et al (2016) Clinical significance of splenic hilar dissection with splenectomy in advanced proximal gastric cancer: an analysis at a single institution in Japan. World J Surg 40:1165–1171
Maezawa Y, Aoyama T, Yamada T et al (2018) Priority of lymph node dissection for proximal gastric cancer invading the greater curvature. Gastric Cancer 21:569–572
Yura M, Yoshikawa T, Otsuki S et al (2019) The therapeutic survival benefit of splenic hilar nodal dissection for advanced proximal gastric cancer invading the greater curvature. Ann Surg Oncol 26:829–835
Hayashi T, Yoshikawa T, Kamiya A et al (2020) Is splenectomy for dissecting splenic hilar lymph nodes justified for scirrhous gastric cancer? Gastric Cancer. Epub 2020 Mar 24
Sasako M, Sano T, Yamamoto S et al (2008) D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med 359:453–462
Griffith JP, Sue-Ling HM, Martin I et al (1995) Preservation of the spleen improves survival after radical surgery for gastric cancer. Gut 36:684–690
Wang S, Xu L, Wang Q et al (2019) Postoperative complications and prognosis after radical gastrectomy for gastric cancer: a systematic review and meta-analysis of observational studies. World J Surg Oncol 17:52
Kurokawa Y, Doki Y, Mizusawa J et al (2018) Bursectomy versus omentectomy alone for resectable gastric cancer (JCOG1001): a phase 3, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 3:460–468
Sakuramoto S, Sasako M, Yamaguchi T et al (2007) Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med 357:1810–1820
Fuse N, Bando H, Chin K et al (2017) Adjuvant capecitabine plus oxaliplatin after D2 gastrectomy in Japanese patients with gastric cancer: a phase II study. Gastric Cancer 20:332–340
Kaminishi M, Shimoyama S, Yamaguchi H et al (1994) Results of subtotal gastrectomy with complete dissection of the N2 lymph nodes preserving the spleen and pancreas in surgery for gastric cancer. Hepatogastroenterology 41:384–387
Hyung WJ, Lim JS, Song J et al (2008) Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. J Am Coll Surg 207:e6-11
Son T, Lee JH, Kim YM et al (2014) Robotic spleen-preserving total gastrectomy for gastric cancer: comparison with conventional laparoscopic procedure. Surg Endosc 28:2606–2615
Guo X, Peng Z, Lv X et al (2018) Randomized controlled trial comparing short-term outcomes of laparoscopic and open spleen-preserving splenic hilar lymphadenectomy for advanced proximal gastric cancer: An interim report. J Surg Oncol 118:1264–1270
Kinoshita T, Sato R, Akimoto E et al (2020) Can laparoscopic spleen-preserving splenic hilar lymph node dissection replace prophylactic splenectomy for proximal advanced gastric cancers that invade the greater curvature? Eur J Surg Oncol. Epub 2020 Nov 26
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Ito reports grants from MSD, grants from Ono Pharma, personal fees from Taiho Pharma, personal fees from Astra Zeneca, outside the submitted work. Dr. Kodera reports grants from Taiho Pharma, grants from Chugai Pharma, grants from Takeda, grants from MSD, grants from Nihon Kayaku, grants from Yakult, grants from Lilly Japan, grants from Ono Pharma, grants from Kaken Pharma, grants from Covidien, grants from EA Pharma, grants from Novartis, grants from KCI, grants from Maruho, grants from Daiichi Sankyo, grants from Otsuka, grants from Tsumura, grants from Sawai, personal fees from Taiho Pharma, personal fees from Chugai Pharma, personal fees from Lilly Japan, personal fees from Johnson & Johnson, personal fees from Takeda, personal fees from Yakult, personal fees from Otsuka, personal fees from Ono Pharma, personal fees from Covidien, personal fees from MSD, grants from Bristol, grants from Sanofi, outside the submitted work. Other authors have nothing to disclose.
Informed consent
Written, informed consent for use of clinical data was granted when required by the Institutional Review Board at each participating institute. In some institutions, opt-out recruitment was employed according to the policy of the Japanese government because this clinical research was conducted using only retrospective clinical data without intervention. The purpose, design, and objectives of the study were posted on the homepage of the Nagoya University Graduate School of Medicine to provide an opportunity for patients to decline to contribute to our study.
Human and animal rights
This study conformed fully to the ethical guidelines of the World Medical Association Declaration of Helsinki–Ethical Principles for Medical Research Involving Human Subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ito, S., Kanda, M., Mochizuki, Y. et al. Efficacy of Splenectomy for Proximal Gastric Cancer with Greater Curvature Invasion or Type 4 Tumor: a Propensity Score Analysis of a Multi-Institutional Dataset. World J Surg 45, 2840–2848 (2021). https://doi.org/10.1007/s00268-021-06173-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06173-6